You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Travelers' Diarrhea
Español

Travelers' diarrhea is the most common travel-related illness. It can occur anywhere, but the highest-risk destinations are in Asia (except for Japan and South Korea) as well as the Middle East, Africa, Mexico, and Central and South America.
In otherwise healthy adults, diarrhea is rarely serious or life-threatening, but it can make a trip very unpleasant.
You can take steps to avoid travelers’ diarrhea
- Choose food and drinks carefully Eat only foods that are cooked and served hot. Avoid food that has been sitting on a buffet. Eat raw fruits and vegetables only if you have washed them in clean water or peeled them. Only drink beverages from factory-sealed containers, and avoid ice because it may have been made from unclean water.
- Wash your hands Wash your hands often with soap and water, especially after using the bathroom and before eating. If soap and water aren’t available, use an alcohol-based hand sanitizer. In general, it’s a good idea to keep your hands away from your mouth.
Learn some ways to treat travelers’ diarrhea

- Drink lots of fluids If you get diarrhea, drink lots of fluids to stay hydrated. In serious cases of travelers’ diarrhea, oral rehydration solution—available online or in pharmacies in developing countries—can be used for fluid replacements.
- Take over-the-counter drugs Several drugs, such as loperamide, can be bought over-the-counter to treat the symptoms of diarrhea. These drugs decrease the frequency and urgency of needing to use the bathroom, and may make it easier for you to ride on a bus or airplane while waiting for an antibiotic to take effect.
- Only take antibiotics if needed Your doctor may give you antibiotics to treat travelers’ diarrhea, but consider using them only for severe cases. If you take antibiotics, take them exactly as your doctor instructs. If severe diarrhea develops soon after you return from your trip, see a doctor and ask for stool tests so you can find out which antibiotic will work for you.
More Information
- Travelers’ Diarrhea- CDC Yellow Book
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
The treatment and prevention of travelers' diarrhea are discussed here. The epidemiology, microbiology, clinical manifestations, and diagnosis of travelers' diarrhea are discussed separately. (See "Travelers' diarrhea: Epidemiology, microbiology, clinical manifestations, and diagnosis" .)
Clinical approach — Management of travelers’ diarrhea depends on the severity of illness. Fluid replacement is an essential component of treatment for all cases of travelers’ diarrhea. Most cases are self-limited and resolve on their own within three to five days of treatment with fluid replacement only. Antimotility agents can provide symptomatic relief but should not be used when bloody diarrhea is present. Antimicrobial therapy shortens the disease duration, but the benefit of antibiotics must be weighed against potential risks, including adverse effects and selection for resistant bacteria. These issues are discussed in the sections that follow.
When to seek care — Travelers from resource-rich settings who develop diarrhea while traveling to resource-limited settings generally can treat themselves rather than seek medical advice while traveling. However, medical evaluation may be warranted in patients who develop high fever, abdominal pain, bloody diarrhea, or vomiting. Otherwise, for most patients while traveling or after returning home, medical consultation is generally not warranted unless symptoms persist for 10 to 14 days.
Fluid replacement — The primary and most important treatment of travelers' (or any other) diarrhea is fluid replacement, since the most significant complication of diarrhea is volume depletion [ 11,12 ]. The approach to fluid replacement depends on the severity of the diarrhea and volume depletion. Travelers can use the amount of urine passed as a general guide to their level of volume depletion. If they are urinating regularly, even if the color is dark yellow, the diarrhea and volume depletion are likely mild. If there is a paucity of urine and that small amount is dark yellow, the diarrhea and volume depletion are likely more severe.
- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
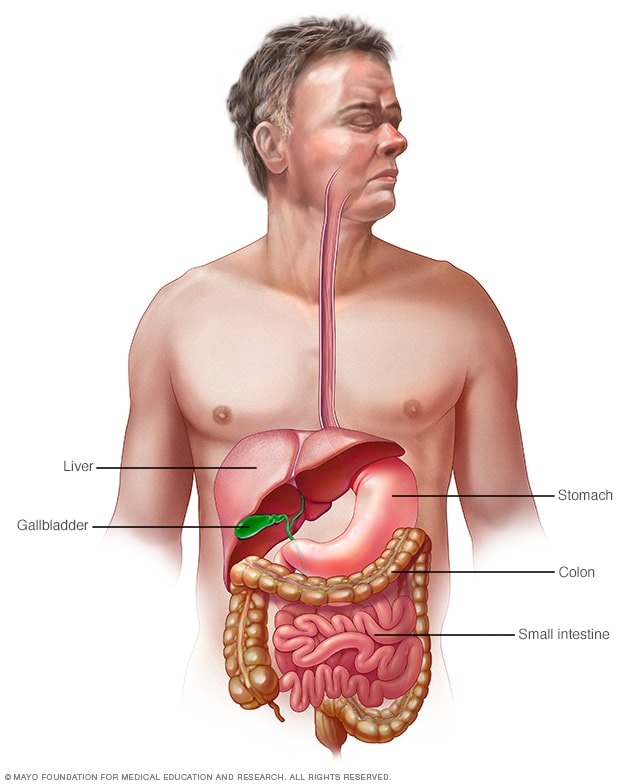
Gastrointestinal tract
Your digestive tract stretches from your mouth to your anus. It includes the organs necessary to digest food, absorb nutrients and process waste.
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant.
When you visit a place where the climate or sanitary practices are different from yours at home, you have an increased risk of developing traveler's diarrhea.
To reduce your risk of traveler's diarrhea, be careful about what you eat and drink while traveling. If you do develop traveler's diarrhea, chances are it will go away without treatment. However, it's a good idea to have doctor-approved medicines with you when you travel to high-risk areas. This way, you'll be prepared in case diarrhea gets severe or won't go away.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
Traveler's diarrhea may begin suddenly during your trip or shortly after you return home. Most people improve within 1 to 2 days without treatment and recover completely within a week. However, you can have multiple episodes of traveler's diarrhea during one trip.
The most common symptoms of traveler's diarrhea are:
- Suddenly passing three or more looser watery stools a day.
- An urgent need to pass stool.
- Stomach cramps.
Sometimes, people experience moderate to severe dehydration, ongoing vomiting, a high fever, bloody stools, or severe pain in the belly or rectum. If you or your child experiences any of these symptoms or if the diarrhea lasts longer than a few days, it's time to see a health care professional.
When to see a doctor
Traveler's diarrhea usually goes away on its own within several days. Symptoms may last longer and be more severe if it's caused by certain bacteria or parasites. In such cases, you may need prescription medicines to help you get better.
If you're an adult, see your doctor if:
- Your diarrhea lasts beyond two days.
- You become dehydrated.
- You have severe stomach or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
While traveling internationally, a local embassy or consulate may be able to help you find a well-regarded medical professional who speaks your language.
Be especially cautious with children because traveler's diarrhea can cause severe dehydration in a short time. Call a doctor if your child is sick and has any of the following symptoms:
- Ongoing vomiting.
- A fever of 102 F (39 C) or more.
- Bloody stools or severe diarrhea.
- Dry mouth or crying without tears.
- Signs of being unusually sleepy, drowsy or unresponsive.
- Decreased volume of urine, including fewer wet diapers in infants.
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become used to the bacteria and have developed immunity to them.
Risk factors
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of:
- Central America.
- South America.
- South Asia and Southeast Asia.
Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses some risk. However, your risk of traveler's diarrhea is generally low in Northern and Western Europe, Japan, Canada, Singapore, Australia, New Zealand, and the United States.
Your chances of getting traveler's diarrhea are mostly determined by your destination. But certain groups of people have a greater risk of developing the condition. These include:
- Young adults. The condition is slightly more common in young adult tourists. Though the reasons why aren't clear, it's possible that young adults lack acquired immunity. They may also be more adventurous than older people in their travels and dietary choices, or they may be less careful about avoiding contaminated foods.
- People with weakened immune systems. A weakened immune system due to an underlying illness or immune-suppressing medicines such as corticosteroids increases risk of infections.
- People with diabetes, inflammatory bowel disease, or severe kidney, liver or heart disease. These conditions can leave you more prone to infection or increase your risk of a more-severe infection.
- People who take acid blockers or antacids. Acid in the stomach tends to destroy organisms, so a reduction in stomach acid may leave more opportunity for bacterial survival.
- People who travel during certain seasons. The risk of traveler's diarrhea varies by season in certain parts of the world. For example, risk is highest in South Asia during the hot months just before the monsoons.
Complications
Because you lose vital fluids, salts and minerals during a bout with traveler's diarrhea, you may become dehydrated, especially during the summer months. Dehydration is especially dangerous for children, older adults and people with weakened immune systems.
Dehydration caused by diarrhea can cause serious complications, including organ damage, shock or coma. Symptoms of dehydration include a very dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness.
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Don't consume unpasteurized milk and dairy products, including ice cream.
- Don't eat raw or undercooked meat, fish and shellfish.
- Don't eat moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Don't drink unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Don't use locally made ice cubes or drink mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You also can chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They also can cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medicine for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medicines, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears, called tinnitus.
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
- Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Traveller's diarrhoea
Peer reviewed by Dr Colin Tidy, MRCGP Last updated by Dr Toni Hazell Last updated 10 Feb 2023
Meets Patient’s editorial guidelines
In this series: Amoebiasis Giardia
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. It is caused by consuming food and water, contaminated by germs (microbes) including bacteria, viruses and parasites. Other symptoms can include high temperature (fever), being sick (vomiting) and tummy (abdominal) pain. In most cases it causes a mild illness and symptoms clear within 3 to 4 days. Specific treatment is not usually needed but it is important to drink plenty of fluids to avoid lack of fluid in the body (dehydration). Always make sure that you get any advice that you need in plenty of time before your journey - some GPs offer travel advice but if yours doesn't then you may need to go to a private travel clinic.
In this article :
What is traveller's diarrhoea, what causes traveller's diarrhoea, are all travellers at risk, what are the symptoms of traveller's diarrhoea, how is traveller's diarrhoea diagnosed, when should i seek medical advice for traveller's diarrhoea, how is traveller's diarrhoea in adults treated, how is traveller's diarrhoea in children treated, side-effects of traveller's diarrhoea, how long does traveller's diarrhoea last, how can i avoid traveller's diarrhoea.
Continue reading below
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. Diarrhoea is defined as: 'loose or watery stools (faeces), usually at least three times in 24 hours.'
Traveller's diarrhoea is caused by eating food, or drinking water, containing certain germs (microbes) or their poisons (toxins). The types of germs which may be the cause include:
Bacteria: these are the most common microbes that cause traveller's diarrhoea. Common types of bacteria involved are:
Escherichia coli
Campylobacter
Viruses: these are the next most common, particularly norovirus and rotavirus.
Parasites: these are less common causes. Giardia, cryptosporidium and Entamoeba histolytica are examples of parasites that may cause traveller's diarrhoea.
Often the exact cause of traveller's diarrhoea is not found and studies have shown that in many people no specific microbe is identified despite testing (for example, of a stool (faeces) specimen).
See the separate leaflets called E. Coli (VTEC O157) , Campylobacter, Salmonella, Cryptosporidium , Amoebiasis (dysentery information), Shigella and Giardia for more specific details on each of the microbes mentioned above.
Note : this leaflet is about traveller's diarrhoea in general and how to help prevent it.
Traveller's diarrhoea most commonly affects people who are travelling from a developed country, such as the UK, to a developing country where sanitation and hygiene measures may not meet the same standards. It can affect as many as 2 to 6 in 10 travellers.
There is a different risk depending on whether you travel to high-risk areas or not:
High-risk areas : South and Southeast Asia, Central America, West and North Africa, South America, East Africa.
Medium-risk areas : Russia, China, Caribbean, South Africa.
Low-risk areas : North America, Western Europe, Australia and New Zealand.
Sometimes outbreaks of diarrhoea can occur in travellers staying in one hotel or, for example, those staying on a cruise ship. People travelling in more remote areas (for example, trekkers and campers) may also have limited access to medical care if they do become unwell.
By definition, diarrhoea is the main symptom. This can be watery and can sometimes contain blood. Other symptoms may include:
Crampy tummy (abdominal) pains.
Feeling sick (nausea).
Being sick (vomiting).
A high temperature (fever).
Symptoms are usually mild in most people and last for 3 to 4 days but they may last longer. Symptoms may be more severe in the very young, the elderly, and those with other health problems. Those whose immune systems are not working as well as normal are particularly likely to be more unwell. For example, people with untreated HIV infection, those on chemotherapy, those on long-term steroid treatment or those who are taking drugs which suppress their immune system, for example after a transplant or to treat an autoimmune condition
Despite the fact that symptoms are usually fairly mild, they can often mean that your travel itinerary is interrupted or may need to be altered.
Traveller's diarrhoea is usually diagnosed by the typical symptoms. As mentioned above, most people have mild symptoms and do not need to seek medical advice. However, in some cases medical advice is needed (see below).
If you do see a doctor, they may suggest that a sample of your stool (faeces) be tested. This will be sent to the laboratory to look for any microbes that may be causing your symptoms. Sometimes blood tests or other tests may be needed if you have more severe symptoms or develop any complications.
As mentioned above, most people with traveller's diarrhoea have relatively mild symptoms and can manage these themselves by resting and making sure that they drink plenty of fluids. However, you should seek medical advice in any of the following cases, or if any other symptoms occur that you are concerned about:
If you have a high temperature (fever).
If you have blood in your stools (faeces).
If it is difficult to get enough fluid because of severe symptoms: frequent or very watery stools or repeatedly being sick (vomiting).
If the diarrhoea lasts for more than 5-7 days.
If you are elderly or have an underlying health problem such as diabetes, inflammatory bowel disease, or kidney disease.
If you have a weakened immune system because of, for example, chemotherapy treatment, long-term steroid treatment, or HIV infection.
If you are pregnant.
If an affected child is under the age of 6 months.
If you develop any of the symptoms listed below that suggest you might have lack of fluid in your body (dehydration). If it is your child who is affected, there is a separate list for children.
Symptoms of dehydration in adults
Dizziness or light-headedness.
Muscle cramps.
Sunken eyes.
Passing less urine.
A dry mouth and tongue.
Becoming irritable.
Symptoms of severe dehydration in adults
Profound loss of energy or enthusiasm (apathy).
A fast heart rate
Producing very little urine.
Coma, which may occur.
Note : severe dehydration is a medical emergency and immediate medical attention is needed.
Symptoms of dehydration in children
Passing little urine.
A dry mouth.
A dry tongue and lips.
Fewer tears when crying.
Being irritable.
Having a lack of energy (being lethargic).
Symptoms of severe dehydration in children
Drowsiness.
Pale or mottled skin.
Cold hands or feet.
Very few wet nappies.
Fast (but often shallow) breathing.
Dehydration is more likely to occur in:
Babies under the age of 1 year (and particularly those under 6 months old). This is because babies don't need to lose much fluid to lose a significant proportion of their total body fluid.
Babies under the age of 1 year who were a low birth weight and who have not caught up with their weight.
A breastfed baby who has stopped being breastfed during their illness.
Any baby or child who does not drink much when they have a gut infection (gastroenteritis).
Any baby or child with severe diarrhoea and vomiting. (For example, if they have passed five or more diarrhoeal stools and/or vomited two or more times in the previous 24 hours.)
In most cases, specific treatment of traveller's diarrhoea is not needed. The most important thing is to make sure that you drink plenty of fluids to avoid lack of fluid in your body (dehydration).
Fluid replacement
As a rough guide, drink at least 200 mls after each watery stool (bout of diarrhoea).
This extra fluid is in addition to what you would normally drink. For example, an adult will normally drink about two litres a day but more in hot countries. The above '200 mls after each watery stool' is in addition to this usual amount that you would drink.
If you are sick (vomit), wait 5-10 minutes and then start drinking again but more slowly. For example, a sip every 2-3 minutes but making sure that your total intake is as described above.
You will need to drink even more if you are dehydrated. A doctor will advise on how much to drink if you are dehydrated.
Note : if you suspect that you are becoming dehydrated, you should seek medical advice.
For most adults, fluids drunk to keep hydrated should mainly be water. However, this needs to be safe drinking water - for example, bottled, or boiled and treated water. It is best not to have drinks that contain a lot of sugar, such as fizzy drinks, as they can sometimes make diarrhoea worse. Alcohol should also be avoided.
Rehydration drinks
Rehydration drinks may also be used. They are made from sachets that you can buy from pharmacies and may be a sensible thing to pack in your first aid kit when you travel. You add the contents of the sachet to water.
Home-made salt/sugar mixtures are used in developing countries if rehydration drinks are not available; however, they have to be made carefully, as too much salt can be dangerous. Rehydration drinks are cheap and readily available in the UK, and are the best treatment. Note that safe drinking water should be used to reconstitute oral rehydration salt sachets.
Antidiarrhoeal medication
Antidiarrhoeal medicines are not usually necessary or wise to take when you have traveller's diarrhoea. However you may want to use them if absolutely necessary - for example, if you will be unable to make regular trips to the toilet due to travelling.You can buy antidiarrhoeal medicines from pharmacies before you travel. The safest and most effective is loperamide.
The adult dose of this is two capsules at first. This is followed by one capsule after each time you pass some diarrhoea up to a maximum of eight capsules in 24 hours. It works by slowing down your gut's activity.
You should not take loperamide for longer than two days. You should also not use antidiarrhoeal medicines if you have a high temperature (fever) or bloody diarrhoea.
Eat as normally as possible
It used to be advised to 'starve' for a while if you had diarrhoea. However, now it is advised to eat small, light meals if you can. Be guided by your appetite. You may not feel like food and most adults can do without food for a few days. Eat as soon as you are able but don't stop drinking. If you do feel like eating, avoid fatty, spicy or heavy food. Plain foods such as bread and rice are good foods to try eating.
Antibiotic medicines
Most people with traveller's diarrhoea do not need treatment with antibiotic medicines. However, sometimes antibiotic treatment is advised. This may be because a specific germ (microbe) has been identified after testing of your stool (faeces) sample.
Fluids to prevent dehydration
You should encourage your child to drink plenty of fluids. The aim is to prevent lack of fluid in the body (dehydration). The fluid lost in their sick (vomit) and/or diarrhoea needs to be replaced. Your child should continue with their normal diet and usual drinks. In addition, they should also be encouraged to drink extra fluids. However, avoid fruit juices or fizzy drinks, as these can make diarrhoea worse.
Babies under 6 months old are at increased risk of dehydration. You should seek medical advice if they develop acute diarrhoea. Breast feeds or bottle feeds should be encouraged as normal. You may find that your baby's demand for feeds increases. You may also be advised to give extra fluids (either water or rehydration drinks) in between feeds.
If you are travelling to a destination at high risk for traveller's diarrhoea, you might want to consider buying oral rehydration sachets for children before you travel. These can provide a perfect balance of water, salts and sugar for them and can be used for fluid replacement. Remember that, as mentioned above, safe water is needed to reconstitute the sachets.
If your child vomits, wait 5-10 minutes and then start giving drinks again but more slowly (for example, a spoonful every 2-3 minutes). Use of a syringe can help in younger children who may not be able to take sips.
Note : if you suspect that your child is dehydrated, or is becoming dehydrated, you should seek medical advice urgently.
Fluids to treat dehydration
If your child is mildly dehydrated, this may be treated by giving them rehydration drinks. A doctor will advise about how much to give. This can depend on the age and the weight of your child. If you are breastfeeding, you should continue with this during this time. It is important that your child be rehydrated before they have any solid food.
Sometimes a child may need to be admitted to hospital for treatment if they are dehydrated. Treatment in hospital usually involves giving rehydration solution via a special tube called a 'nasogastric tube'. This tube passes through your child's nose, down their throat and directly into their stomach. An alternative treatment is with fluids given directly into a vein (intravenous fluids).
Eat as normally as possible once any dehydration has been treated
Correcting any dehydration is the first priority. However, if your child is not dehydrated (most cases), or once any dehydration has been corrected, then encourage your child to have their normal diet. Do not 'starve' a child with infectious diarrhoea. This used to be advised but is now known to be wrong. So:
Breastfed babies should continue to be breastfed if they will take it. This will usually be in addition to extra rehydration drinks (described above).
Bottle-fed babies should be fed with their normal full-strength feeds if they will take it. Again, this will usually be in addition to extra rehydration drinks (described above). Do not water down the formula, or make it up with less water than usual. This can make a baby very ill.
Older children - offer them some food every now and then. However, if he or she does not want to eat, that is fine. Drinks are the most important consideration and food can wait until the appetite returns.
Loperamide is not recommended for children with diarrhoea. There are concerns that it may cause a blockage of the gut (intestinal obstruction) in children with diarrhoea.
Most children with traveller's diarrhoea do not need treatment with antibiotics. However, for the same reasons as discussed for adults above, antibiotic treatment may sometimes be advised in certain cases.
Most people have mild illness and complications of traveller's diarrhoea are rare. However, if complications do occur, they can include the following:
Salt (electrolyte) imbalance and dehydration .
This is the most common complication. It occurs if the salts and water that are lost in your stools (faeces), or when you are sick (vomit), are not replaced by you drinking adequate fluids. If you can manage to drink plenty of fluids then dehydration is unlikely to occur, or is only likely to be mild and will soon recover as you drink.
Severe dehydration can lead to a drop in your blood pressure. This can cause reduced blood flow to your vital organs. If dehydration is not treated, your kidneys may be damaged . Some people who become severely dehydrated need a 'drip' of fluid directly into a vein. This requires admission to hospital. People who are elderly or pregnant are more at risk of dehydration.
Reactive complications
Rarely, other parts of your body can 'react' to an infection that occurs in your gut. This can cause symptoms such as joint inflammation (arthritis), skin inflammation and eye inflammation (either conjunctivitis or uveitis). Reactive complications are uncommon if you have a virus causing traveller's diarrhoea.
Spread of infection
The infection can spread to other parts of your body such as your bones, joints, or the meninges that surround your brain and spinal cord. This is rare. If it does occur, it is more likely if diarrhoea is caused by salmonella infection.
Irritable bowel syndrome is sometimes triggered by a bout of traveller's diarrhoea.
Lactose intolerance
Lactose intolerance can sometimes occur for a period of time after traveller's diarrhoea. It is known as 'secondary' or 'acquired' lactose intolerance. Your gut (intestinal) lining can be damaged by the episode of diarrhoea. This leads to lack of a substance (enzyme) called lactase that is needed to help your body digest the milk sugar lactose.
Lactose intolerance leads to bloating, tummy (abdominal) pain, wind and watery stools after drinking milk. The condition gets better when the infection is over and the intestinal lining heals. It is more common in children.
Haemolytic uraemic syndrome
Usually associated with traveller's diarrhoea caused by a certain type of E. coli infection, haemolytic uraemic syndrome is a serious condition where there is anaemia, a low platelet count in the blood and kidney damage. It is more common in children. If recognised and treated, most people recover well.
Guillain-Barré syndrome
This condition may rarely be triggered by campylobacter infection, one of the causes of traveller's diarrhoea. It affects the nerves throughout your body and limbs, causing weakness and sensory problems. See the separate leaflet called Guillain-Barré syndrome for more details.
Reduced effectiveness of some medicines
During an episode of traveller's diarrhoea, certain medicines that you may be taking for other conditions or reasons may not be as effective. This is because the diarrhoea and/or being sick (vomiting) mean that reduced amounts of the medicines are taken up (absorbed) into your body.
Examples of such medicines are those for epilepsy, diabetes and contraception . Speak with your doctor or practice nurse before you travel if you are unsure of what to do if you are taking other medicines and develop diarrhoea.
As mentioned above, symptoms are usually short-lived and the illness is usually mild with most people making a full recovery within in few days. However, a few people with traveller's diarrhoea develop persistent (chronic) diarrhoea that can last for one month or more. It is also possible to have a second 'bout' of traveller's diarrhoea during the same trip. Having it once does not seem to protect you against future infection.
Avoid uncooked meat, shellfish or eggs. Avoid peeled fruit and vegetables (including salads).
Be careful about what you drink. Don't drink tap water, even as ice cubes.
Wash your hands regularly, especially before preparing food or eating.
Be careful where you swim. Contaminated water can cause traveller's diarrhoea.
Regular hand washing
You should ensure that you always wash your hands and dry them thoroughly; teach children to wash and dry theirs:
After going to the toilet (and after changing nappies or helping an older child to go to the toilet).
Before preparing or touching food or drinks.
Before eating.
Some antibacterial hand gel may be a good thing to take with you when you travel in case soap and hot water are not available.
Be careful about what you eat and drink
When travelling to areas with poor sanitation, you should avoid food or drinking water that may contain germs (microbes) or their poisons (toxins). Avoid:
Fruit juices sold by street vendors.
Ice cream (unless it has been made from safe water).
Shellfish (for example, mussels, oysters, clams) and uncooked seafood.
Raw or undercooked meat.
Fruit that has already been peeled or has a damaged skin.
Food that contains raw or uncooked eggs, such as mayonnaise or sauces.
Unpasteurised milk.
Drinking bottled water and fizzy drinks that are in sealed bottles or cans, tea, coffee and alcohol is thought to be safe. However, avoid ice cubes and non-bottled water in alcoholic drinks. Food should be cooked through thoroughly and be piping hot when served.
You should also be careful when eating food from markets, street vendors or buffets if you are uncertain about whether it has been kept hot or kept refrigerated. Fresh bread is usually safe, as is canned food or food in sealed packs.
Be careful where you swim
Swimming in contaminated water can also lead to traveller's diarrhoea. Try to avoid swallowing any water as you swim; teach children to do the same.
Obtain travel health advice before you travel
Always make sure that you visit your GP surgery or private travel clinic for health advice in plenty of time before your journey. Alternatively, the Fit for Travel website (see under Further Reading and References, below) provides travel health information for the public and gives specific information for different countries and high-risk destinations. This includes information about any vaccinations required, advice about food, water and personal hygiene precautions, etc.
There are no vaccines that prevent traveller's diarrhoea as a whole. However, there are some other vaccines that you may need for your travel, such as hepatitis A, typhoid, etc. You may also need to take malaria tablets depending on where you are travelling.
Antibiotics
Taking antibiotic medicines to prevent traveller's diarrhoea (antibiotic prophylaxis) is not generally recommended. This is because for most people, traveller's diarrhoea is mild and self-limiting. Also, antibiotics do not protect against nonbacterial causes of traveller's diarrhoea, such as viruses and parasites. Antibiotics may have side-effects and their unnecessary use may lead to problems with resistance to medicines.
Probiotics have some effect on traveller's diarrhoea and can shorten an attack by about one day. It is not known yet which type of probiotic or which dose, so there are no recommendations about using probiotics to prevent traveller's diarrhoea.
Further reading and references
- Bourgeois AL, Wierzba TF, Walker RI ; Status of vaccine research and development for enterotoxigenic Escherichia coli. Vaccine. 2016 Mar 15. pii: S0264-410X(16)00287-5. doi: 10.1016/j.vaccine.2016.02.076.
- Travellers' diarrhoea ; Fitfortravel
- Riddle MS, Connor BA, Beeching NJ, et al ; Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. J Travel Med. 2017 Apr 1;24(suppl_1):S57-S74. doi: 10.1093/jtm/tax026.
- Giddings SL, Stevens AM, Leung DT ; Traveler's Diarrhea. Med Clin North Am. 2016 Mar;100(2):317-30. doi: 10.1016/j.mcna.2015.08.017.
- Diarrhoea - prevention and advice for travellers ; NICE CKS, February 2019 (UK access only)
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Feb 2028
10 feb 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Traveler's Diarrhea
What is traveler's diarrhea, what causes traveler's diarrhea.
It’s caused by drinking water or eating food that has bacteria, viruses, or parasites. Most traveler's diarrhea is from bacteria. Diarrhea from viruses and parasites is less common. Food and water can be infected by people:
- Not washing hands after using the bathroom
- Storing food unsafely
- Handling and preparing food unsafely
- Not cleaning surfaces and utensils safely
Who is at risk for traveler's diarrhea?
You are at risk for this condition if you travel to a country that has poor public sanitation and hygiene. Poor hygiene in local restaurants is also a risk factor. Places that have the highest risk are often in developing countries in:
- Central and South America
- The Middle East
If you travel to a developing country, you are more likely to get this illness if you eat food or have drinks:
- Bought on the street, such as from a food cart
- In someone’s home
- At lodging that provides all meals (all-inclusive)
You’re also at increased risk if you:
- Take some kinds of ulcer medicine
- Have had some kinds of gastrointestinal surgery
What are the symptoms of traveler's diarrhea?
The main symptom is loose stool that occurs suddenly. The stool may be watery. Other symptoms may include:
- Belly (abdominal) pain or cramps
- Blood in the stool
- Trouble waiting to have a bowel movement (urgency)
- Feeling tired
In most cases, symptoms last less than a week.
How is traveler's diarrhea diagnosed?
How is traveler's diarrhea treated, what are possible complications of traveler's diarrhea.
The loss of body fluid from diarrhea and vomiting can lead to dehydration. This can be serious. Contact your healthcare provider if you are not urinating as much as usual.
A small number of people can develop post-infectious irritable bowel syndrome. This can cause symptoms such as:
- Long-term diarrhea
- Belly pain and cramping
What can I do to prevent traveler's diarrhea?
You can take steps to prevent traveler's diarrhea.
Only use water that has been boiled or chemically disinfected for:
- Making tea or coffee
- Brushing your teeth
- Washing your face
- Washing your hands (or use alcohol-based gel)
- Washing fruits and vegetables
- Washing food utensils, equipment, or surfaces
- Washing the surfaces of food or drink tins, cans, and bottles
Don't eat foods such as:
- Raw fruits, vegetables, or salad greens
- Unpasteurized milk, cheese, ice cream, or yogurt
- Any fish caught in tropical reefs rather than the open ocean
- Condiments that are left on the table, such as ketchup, mustard, sauces, or dips
Also make sure to:
- Not eat food from unknown sources
- Not put ice in drinks
- Only have drinks that are bottled and sealed
- Use drinking straws instead of drinking directly from glasses or cups
- Only take antibiotic or antidiarrheal medicine if advised by your health care provider (these can make symptoms worse, which can be dangerous)
When should I call my healthcare provider?
Call a healthcare provider if you:
- Have diarrhea that is severe or bloody
- Have belly pain that is getting worse or not going away
- Have a high fever
- Are not getting better within a few days
- Have signs of dehydration, such as urinating less
- Traveler's diarrhea occurs within 10 days of travel to an area with poor public hygiene. It’s the most common illness in travelers.
- It’s caused by drinking water or eating foods that have bacteria, viruses, or parasites.
- It usually goes away without treatment in a few days.
- Dehydration from diarrhea can be serious. You need to replace body fluid that has been lost.
- See a healthcare provider if your symptoms are severe or last for more than a few days.
- You can prevent it by avoiding unsafe water and not eating unsafe foods.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Find a Doctor
Specializing In:
- Gastroenterology
- Indigestion
- Diarrheal Disease
- Clostridium Difficile
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Gastroenterology and Hepatology
Find Additional Treatment Centers at:
Request an Appointment

Collagenous and Lymphocytic Colitis
Diarrhea in Children
Related Topics
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Best Traveler's Diarrhea Treatments for Symptom Relief
Sources of Bacteria, Prevention, and Medication Types
Complications
Frequently asked questions.
Traveler's diarrhea can turn a trip into a nightmare. Food and water contaminated by germs, also known as pathogens , is not uncommon in certain areas of the world that are popular travel destinations. Consuming even small amounts of these germs can cause loose, watery stool, the main sign of diarrhea , Luckily, treatment options are available.
This article explains the symptoms of traveler's diarrhea, how to treat it, and the best ways to prevent getting infected in the first place.
Luis Alvarez / Getty Images
Symptoms of traveler's diarrhea caused by bacteria or a virus usually appear six to 72 hours after eating or drinking something contaminated. With some types of pathogens, it may take a week or longer for stool to be affected.
Changes in your bowel habits it the main symptoms of diarrhea. At its mildest, diarrhea involves passing loose, watery stool three times a day. You may pass unformed stool 10 or more times a day in severe cases.
Other symptoms vary depending on the type of bacterial or virus you've been exposed to but may include:
- Stomach cramps
- Tenesmus , feeling you need to have a bowel movement even when your bowels are empty
- Mucous in stool
More severe cases of traveler's diarrhea may cause bloody stools .
Should You Go to a Doctor for Traveler's Diarrhea?
See a healthcare provider if your symptoms are accompanied by fever or bloody stools, or they last longer than 48 hours.
Traveler's Diarrhea Causes
The most common cause of traveler's diarrhea is probably poor hygiene (lack of cleanliness) in restaurants. You're most at risk when dining out in areas of Asia, the Middle East, Mexico, Africa, and South and Central America.
Pathogens are usually spread via the fecal-oral route . This means someone with the bacteria or virus excretes the germs in their feces. The feces may not be safely disposed of in a sanitary setting, or the infected person may not properly wash their hands before handling food and beverages. This allows germs to be transmitted to something you put into your mouth.
This cycle of contamination is most common in areas of the world that have specific conditions:
- Warmer climates that promote germ growth
- Poor sanitation (such as open sewage areas)
- Unreliable refrigeration
- Little education on safe food handling.
Common Bacterial Pathogens
The most common cause of traveler's diarrhea is bacteria, which are thought to lead to 80% to 90% of cases. These include:
- Escherichia coli or E-coli
- Campylobacter jejuni
Ingesting these bacterium causes gastroenteritis , which means the stomach and small intestines become inflamed. This leads to diarrhea.
Common Viral Pathogens
Viruses can also be transported via the fecal-oral route. The most common types of viruses that cause diarrhea include:
Viral infections of the digestive system are often referred to as stomach flu . The illness has no connection to respiratory influenza, but like the "flu," it usually lasts a short period.
Other Causes of Diarrhea
In addition to germs in your food and water, you could develop diarrhea from toxins, which cause the common symptoms of food poisoning .
Parasites , or protozoal pathogens, can also cause diarrhea. In these instances, you're more likely to develop symptoms one to two weeks after exposure to the pathogen.
Dehydration is one of the most common complications related to any form of diarrhea. Multiple bowel movements that release a lot of fluid can cause you to have too little water in your body.
Severe dehydration can lead to problems such as:
- Fatigue and muscle weakness or pain
- Dizziness or lightheadedness
- Increased heart rate and breathing
- Kidney Failure
Dysentery is a serious condition that can develop from exposure to Shigella or parasites. It usually causes bloody stool, fever, and extreme dehydration. It can be fatal if it's left untreated. In addition to being picked up from contaminated food or water, the bacteria or parasites that cause dysentery can be passed from person to person in close contact, or you can get it by swimming in unclean water.
Treatment for Traveler's Diarrhea
Getting sick while far from home is more than just inconvenient. The sudden onset and severity of symptoms can be frightening. Often, symptoms will last a few days and resolve on their own, but you may need to manage the condition and take medication.
Fluid Replacement
To manage dehydration, you want to concentrate on getting enough liquids even if you feel like you don't want to put anything in your stomach.
Drinking any safe fluids can manage mild cases of traveler's diarrhea. Since tap water may be a source of infection, you need to boil non-bottled water and let it cool before you drink it. You can also drink boiled broth or prepackaged (non-citrus) fruit juice. Sports drinks like Gatorade are good, too, but not essential.
For severe dehydration, an oral rehydration solution may be needed. These are mixes or packaged beverages that contain glucose and electrolytes such as potassium and sodium. Pedialyte is an example of an oral rehydration solution for kids.
Sweating can cause dehydration as well. Try to find a cool place out of the sun to rest while you rehydrate.
Antibiotics
Antibiotics may be used for traveler's diarrhea caused by bacterial infections. A stool test should be done to identify which antibiotic might work best.
Quinolone antibiotics such as Cipro (ciprofloxacin) are most often used when antibiotics are needed.
A single dose of 750 milligrams (mg) for adults is the typical treatment. Children may be given 20 to 30 mg per kilogram of weight per day.
In some areas, bacteria are resistant to quinolones, which means the medication won't help. This is especially a problem in Southeast Asia. Another antibiotic, azithromycin , may also be used in this case, although some strains are resistant to it.
Upset Stomach Medication
Pepto-Bismol can provide short-term relief of symptoms. However, it may not be effective in small doses, and high doses put you at risk for a health condition called salicylate toxicity. Additionally, Pepto-Bismol is not recommended for people younger than 18 years because there's a risk of a condition called Reye's syndrome .
Antidiarrheal Agents
It might seem logical to reach for an anti-diarrheal product such as Imodium (loperamide) or Lomotil (diphenoxylate). However, these products should not be used if your diarrhea is related to dysentery or if you see any signs of blood in your stools.
An antidiarrheal agent should only be taken with an antibiotic. When using an antidiarrheal for traveler's diarrhea, it is especially important to keep yourself well-hydrated. Discontinue the product if your symptoms worsen or you still have diarrhea after two days.
How Long Traveler's Diarrhea Lasts
Most cases of traveler's diarrhea last from one to five days. However, symptoms may linger for several weeks.
To help prevent traveler's diarrhea:
- Wash your hands with soap and water after going to the bathroom and before eating.
- At restaurants, only eat foods that are cooked and served hot.
- Drink beverages from factory-sealed bottles or containers.
- Don't get ice in your drink since it may be made with contaminated water.
There is evidence that Pepto-Bismol may protect against traveler's diarrhea. Studies have shown a protection rate of about 60%. However, not everyone should take Pepto-Bismol, including those who are pregnant or are 18 years of age and younger.
Don't take antibiotics or antidiarrheal medicine like Pepto-Bismol as prophylaxis—that is, to prevent traveler's diarrhea— unless it's been recommended to you by your healthcare provider.
Bacteria and viruses can live in water and food. These pathogens (germs) are most common in areas where the climate is warm, refrigeration is unreliable, and there isn't proper hand washing or bathroom sanitation. Infection with these pathogens (bacterial or viral) can cause traveler's diarrhea.
Traveler's diarrhea will often resolve on its own once the bacteria or virus is out of your system. However, you may need antibiotics. You may also need to manage symptoms by staying hydrated and using over-the-counter medications. You should contact your healthcare provider if symptoms last more than a few days.
When traveling to regions that have warm climates and relaxed hygiene practices, be sure to take steps to avoid eating or drinking anything that could have pathogens. Drink pre-packed or boiled water and ensure food is handled properly.
It's important to make sure that your child gets enough fluids. Diarrhea can lead to dehydration more quickly in kids than in adults. Check with your healthcare provider if your child has signs of dehydration such as dry mouth, few or no tears when crying, irritability, reduced urination, and drowsiness.
If you're pregnant, the most important thing to do is to drink enough fluids so you don't get dehydrated. Your doctor may suggest using azithromycin if you need an antibiotic. Don't use Pepto-Bismol (bismuth subsalicylate) when pregnant because of risks to the growing fetus.
Connor BA. Preparing international travelers: Travelers’ diarrhea . In: Brunette GW, ed. CDC Yellow Book 2020: Health information for international travel . Oxford University Press; 2017.
Leung AKC, Leung AAM, Wong AHC, Hon KL. Travelers’ diarrhea: a clinical review . Recent Pat Inflamm Allergy Drug Discov . 2019;13(1):38-48. doi:10.2174/1872213X13666190514105054
Shaheen NA, Alqahtani AA, Assiri H, Alkhodair R, Hussein MA. Public knowledge of dehydration and fluid intake practices: variation by participants' characteristics . BMC Public Health . 2018;18(1):1346. doi:10.1186/s12889-018-6252-5
Strachan SR, Morris LF. Management of severe dehydration . Pediatr Crit Care Med . 2017;18(3):251-255. doi:10.1177/1751143717693859
Riddle MS, Connor BA, Beeching NJ, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report . J Travel Med . 2017;24(suppl_1):S57-S74. doi:10.1093/jtm/tax026
Johns Hopkins Medicine. Traveler's Diarrhea.
Nemours Foundation. KidsHealth. Staying healthy while you travel.
Morof DF, Carroll ID. Family travel: Pregnant travelers . In: Brunette GW, ed. CDC Yellow Book 2020: Health information for international travel . Oxford University Press; 2017.
Wanke, Christine A. " Travelers' Diarrhea ." UpToDate .
By Barbara Bolen, PhD Barbara Bolen, PhD, is a licensed clinical psychologist and health coach. She has written multiple books focused on living with irritable bowel syndrome.
Issues by year
Advertising
Volume 44, Issue 1, January-February 2015
Advising travellers about management of travellers’ diarrhoea
How is td defined.
Classic, severe TD is usually defined as at least three unformed bowel movements occurring within a 24-hour period, often accompanied by cramps, nausea, vomiting, fever and/or blood in the stools. 5–7 Moderate TD is defined as one or two unformed bowel movements and other symptoms occurring every 24 hours or as three or more unformed bowel movements without additional symptoms. Mild TD is defined as one or two unformed bowel movements without any additional symptoms and without interference with daily activities. 8,9 TD generally resolves spontaneously, usually after 3–4 days, 8 but, in the interim, frequently leads to disruption of planned activities.
What are the causes of TD?
Approximately 50–80% of TD is caused by bacterial infections; enterotoxigenic Escherichia coli (ETEC) is the most common cause overall. Other bacterial causes include enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAEC), Shigella , Campylobacter and Salmonella species. The exact breakdown of organisms varies according to destination, season and other factors. Noroviruses cause 10–20% of TD cases. Protozoal parasites should be considered particularly in those with persistent diarrhoea (illness lasting ≥14 days) or when antibacterial therapy fails to shorten illness. 10
How can TD be prevented?
Methods for preventing TD include avoidance, immunisation, non-antibiotic interventions or antibiotic prophylaxis. 11
What avoidance measures are generally recommended and do they work?
Avoidance of TD has traditionally relied on recommendations regarding careful food and drink choices (avoiding untreated/unboiled tap water, including ice and water used for brushing teeth, and raw foods such as salads, uncooked vegetables or fruits that cannot be peeled). This underpins the saying ‘Boil it, cook it, peel it or forget it…. easy to remember, impossible to do’. Additional standard advice is that undercooked or raw meat, fish and shellfish are high-risk foods. However, whether deliberately or inadvertently, most people find it very difficult to adhere to dietary restrictions 12 and over 95% of people disobey the rules of ‘safe’ eating and drinking within a few days of leaving home. Additionally, there is minimal evidence for a correlation between adherence to dietary precautions and a reduced risk of TD, 13 although common sense nevertheless supports care with food selection. 4
Where people eat may be more important than what people eat. Risks are associated, in descending order, with street vendors, restaurants and private homes. Use of antibacterial handwash before eating is also recommended. 14
Which vaccines can be considered?
Immunisation has little practical role in the prevention of TD and the only potentially relevant vaccines are those against rotavirus (infants only) and the oral cholera vaccine.
The cholera vaccine has >90% efficacy for prevention of Vibrio cholera but travellers are rarely at risk of infection with this pathogen. 1 The vaccine contains a recombinant B subunit of the cholera toxin that is antigenically similar to the heat-labile toxin of ETEC; therefore, the cholera vaccine may also reduce ETEC TD. However, it is not licensed for TD prevention in Australia and, although initially thought to offer a 15–20% short-term (3 months) reduction in TD, a recent Cochrane review showed no statistically significant effects on ETEC diarrhoea or all-cause diarrhoea. 15 Overall, there is, therefore, insufficient evidence to support general use of the cholera vaccine for TD protection, but it may still be considered for individuals with increased risk of severe or complicated TD (eg immunosuppressed or underlying inflammatory bowel disease).
Other vaccines directed against organisms spread by the faecal–oral route are the vaccines for typhoid, hepatitis A and polio, but infection with these organisms rarely causes TD. 15
Do non-antibiotic interventions work?
Several probiotic agents have been studied for treatment and prevention of TD, including Lactobacillus and Saccharomyces preparations. However, their effectiveness for TD prevention has been limited, 11,16,17 and a consensus group has recommended against their use. 4 Other over-the-counter agents are also available (eg travelan, which contains bovine colostrum harvested from cows immunised with an ETEC vaccine) but data regarding overall efficacy of reducing all-cause TD are currently lacking.
Should antibiotic prophylaxis against TD be given?
Quinolone antibiotics are highly effective (80–95%) in preventing TD, but antibiotic prophylaxis is rarely indicated. 4 It may result in a false sense of security and hence less caution in dietary choices, it poses risks of side effects, diarrhoea associated with Clostridium difficile , and, more importantly, would lead to a vast amount of antibiotic use, thus predisposing to more rapid development of antibiotic resistance globally. 11 Therefore non-antibiotic options for prevention and a focus instead on empirical self-treatment if needed according to symptoms are the mainstay of management, aligning with the antimicrobial stewardship perspective of minimisation of antimicrobial overuse and reducing promotion of antimicrobial resistance.
In rare circumstances, it may be reasonable to consider short courses of antibiotic prophylaxis in individuals at very high risk of infection (eg severely immunocompromised). 11 Globally, one of the most commonly used agents in this regard is rifaximin, a non-absorbed semisynthetic rifamycin derivative, which has been shown to be effective and is approved for use for TD prevention in some countries, but it is not approved for this indication in Australia. Other options include the antibiotics discussed below for TD self-treatment.
How should self-treatment of TD be managed?
Because of the limitations of TD prevention measures, the pre-travel consultation should be viewed as an opportunity to ‘arm’ travellers with the knowledge and medication needed to appropriately self-treat, should TD occur during their trip.
The first goal of therapy is the prevention and treatment of dehydration, which is of particular concern for young children, pregnant women and the elderly. Commercial packets of oral rehydration salts are readily available in pharmacies and should be purchased before travel. The other element of TD self-treatment is to recommend travellers bring an antimotility agent plus an antibiotic with them. Loperamide is preferred over the diphenoxylate/atropine combination, as the latter agent is generally less effective and associated with a greater potential for adverse effects.
When should loperamide alone versus loperamide plus an antibiotic be taken?
For mild symptoms of watery diarrhoea, self-treatment with oral rehydration plus loperamide is recommended. Loperamide therapy alone has no untoward effects in mild TD 18 but if symptoms worsen, or do not improve after 24 hours, antibiotics should be added. If TD is moderate or severe at onset, then combination therapy with loperamide plus antibiotics should be started immediately, as this optimises the clinical benefit of self-treatment by providing more rapid relief and shortening the symptom duration. 10,19
The recommended dose of loperamide is two tablets (4 mg) stat, then one tablet after each bowel motion to a maximum of eight per 24-hour period until the TD has resolved. Despite warnings regarding the safety of antidiarrhoeal agents with bloody diarrhoea or diarrhoea accompanied by fever, the combination with antibiotics is likely to be safe in the setting of mild febrile dysentery, 18 and a number of studies have shown the combination to be more efficacious than use of either agent alone. 7,18–20 Rapid institution of effective treatment shortens symptoms to 30 hours or less in most people. 12 For example, the duration of diarrhoea was significantly ( P = 0.0002) shorter following treatment with azithromycin plus loperamide (11 h) than with azithromycin alone (34 h). 19
Which antibiotic should be recommended for empirical elf-treatment of TD?
The most commonly used antibiotics for empirical TD therapy are fluoroquinolones (either norfloxacin or ciprofloxacin) or azithromycin ( Table 1 ). Cotrimoxazole has been used but is no longer recommended because of widespread resistance. For TD caused by ETEC, the fluoroquinolones and azithromycin have similar efficacy; however, in Asia (particularly South and South-East Asia), Campylobacter is a common cause of TD and strains occurring in this part of the world show a high degree of resistance to fluoroquinolones. 10,21 Therefore, azithromycin is preferred for travellers to this region. Azithromycin remains generally efficacious despite emerging resistance, and is also the preferred treatment for diarrhoea with complications of dysentery or high fever, and for use in pregnant women or children under the age of 8 years, in whom avoidance of quinolones is preferred. Moreover, the 24-hour dosing of azithromycin may be preferable to the 12-hourly dosing schedule required with fluoroquinolones.
What is the optimal dosing schedule?
The fluoroquinolones and azithromycin have been administered as a single dose or for 3 days ( Table 1 ). Usually a single dose is adequate and there is no apparent clinically important difference in efficacy with either dosing schedule for TD. 10 However, for bacteria such as Campylobacter and Shigella dysenteriae , single-dose therapy may be inadequate. 11 It is reasonable, therefore, to give travellers a 3-day supply of antibiotics and tell them to continue taking the therapy (either 12- or 24-hourly, depending on which antibiotic is prescribed) only if their TD symptoms persist. If the TD has resolved, no further antibiotics need to be taken and any remaining antibiotic doses can be kept in case of a second bout of TD. It is prudent to specifically highlight that this advice differs from the usual instructions to take all tablets even if symptoms have resolved.
What is the optimal empirical TD management in children?
There are few data on empirical treatment of TD in children and limited options for therapy. The mainstay of therapy is oral rehydration solution, particularly for children <6 years of age. Antimotility agents are contraindicated for children because of the increased risk of adverse effects, especially paralytic ileus, toxic megacolon and drowsiness (narcotic effect) with loperamide. 1 The lower age limit recommended for avoiding loperamide varies by location; US guidelines state that loperamide should not be given to infants <2 years of age, the UK <4 years and Australian guidelines state <12 years. 14 However, most Australian practitioners are prepared to use loperamide in children aged 6 years or older, if needed to control symptoms.
A paediatric (powder) formulation of azithromycin is available and is the most commonly recommended agent for children. The usual dose is 10–25 mg/kg for up to 3 days. A practical tip is to ensure that the pharmacy does not reconstitute the powder into a solution, as once dissolved, the solution lasts only for 10 days. Instead, sterile water should be provided along with instructions on how to reconstitute the powder if needed. Fluoroquinolones (ciprofloxacin or norfloxacin 10mg/kg bd) are an alternative option if there are reasons for avoiding azithromycin, with previous concerns regarding potential effects on cartilage not substantiated in recent studies. 14,22
Does starting antibiotics early prevent the chances of developing prolonged symptoms?
Although TD symptoms are short-lived in most cases, 8–15% of affected travellers are symptomatic for more than a week and 2% develop chronic diarrhoea lasting a month or more. 11 Episodes of TD have been shown to be associated with a quintuple risk of developing irritable bowel syndrome (IBS), and post-travel IBS occurs in 3–10% of travellers. However, it is unknown whether IBS can be prevented by starting antimicrobial therapy earlier in the course of enteric infection. 4,18,23
Should tinidazole also be prescribed and, if so, for whom?
Tinidazole can be prescribed as a second antibiotic for empirical self‑treatment as it is effective against the protozoan parasitic enteric pathogen Giardia intestinalis . A dose of 2 g (4 x 500 mg tablets) stat is recommended. However, for most short-term travellers, tinidazole may be unnecessary and the complexity of the additional instructions required may be unwarranted. It is optimally recommended, therefore, for travellers departing on trips of significant duration (>2–3 weeks). If prescribed, the instructions should be to take tinidazole if the TD persists following the 3-day course of antibiotic therapy (fluoroquinolone or azithromycin). This will mean that the TD has lasted for at least 72 hours, thus increasing the likelihood of a parasitic cause.
When should medical care for acute symptoms be recommended?
While most episodes of TD are amenable to self-treatment, if there is a risk of dehydration due to intolerance of oral fluids or comorbidities, as well as in the setting of frank blood in the stool or unremitting fevers (>38.5°C for 48 hours), medical therapy should be sought. 18
How should TD be managed after return?
While a full description of TD management is beyond the scope of this article, for returning travellers with diarrhoea, at least one (preferably three) stool sample(s) should be taken, including specific requests for evaluation of parasites. For patients who are unwell, particularly those with fevers or dysentery, initiation of empirical antibiotic treatment with azithromycin or a quinolone may be needed while awaiting results. For those with prolonged symptoms, tinidazole as empirical therapy for protozoan parasites may be considered. Endoscopic evaluation may also be advisable if no infectious cause is found and symptoms do not resolve.
- Travellers’ diarrhoea continues to affect 20–50% of people undertaking trips to areas with under-developed sanitation and there is minimal evidence for beneficial effects of dietary precautions.
- Evidence for the benefit of cholera vaccine in reducing TD is limited, but it can be considered in people at high risk of infection.
- In 50–80% of TD cases, TD is caused by bacterial infection. Mild diarrhoea can be managed with an antimotility agent (loperamide) alone, but for moderate or severe diarrhoea, early self-treatment with loperamide in conjunction with antibiotics is advised.
- Recommended empirical antibiotics are fluoroquinolones (norfloxacin / ciprofloxacin) or azithromycin for up to 3 days, although in the setting of increasing resistance, the latter is preferred for travellers to South and South-East Asia.
Competing interests: Karin Leader received a consultancy fee from Imuron in relation to the C. difficile vaccine. She is also an ISTM board member and received a consultancy from ISTM to join the GeoSentinel leadership team. She received grants from Sanofi to develop a mobile phone app for splenectomised patients and from GSK to research the use of the HBV vaccine. GSK also paid her to lecture on travel risks at the Asia Pacific Travel Health Conference. She has received support from both GSK and Sanofi to attend travel medicine conferences.
Provenance and peer review: Commissioned, externally peer reviewed
- Diemert DJ. Prevention and self-treatment of travelers’ diarrhea. Prim Care 2002;29:843–55. Search PubMed
- Department of Health and Human Services. Centers for Disease Control and Prevention. Travelers’ Diarrhea. Available at www.cdc.gov/ncidod/dbmd/diseaseinfo/travelersdiarrhea_g.htm [Accessed 25 November 2014]. Search PubMed
- Paredes-Paredes M, Flores-Figueroa J, Dupont HL. Advances in the treatment of travelers’ diarrhea. Curr Gastroenterol Rep 2011;13:402–07. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for prevention of travelers’ diarrhea. J Travel Med 2009;16:149–60. Search PubMed
- Nair D. Travelers’ diarrhea: prevention, treatment, and post-trip evaluation. J Fam Pract 2013;62:356–61. Search PubMed
- De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. The Cochrane Database Syst Rev 2000:CD002242. Search PubMed
- Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler’s diarrhea: a systematic review and meta-analysis. Clin Infect Dis 2008;47:1007–14. Search PubMed
- Steffen R. Epidemiology of traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S536–40. Search PubMed
- Steffen R, Collard F, Tornieporth N, et al. Epidemiology, etiology, and impact of traveler’s diarrhea in Jamaica. JAMA 1999;281:811–17. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med 2009;16:161–71. Search PubMed
- Diemert DJ. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006;19:583–94. Search PubMed
- Travelers’ diarrhea. NIH Consensus Development Conference. JAMA 1985;253:2700–04. Search PubMed
- Shlim DR. Looking for evidence that personal hygiene precautions prevent traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S531–35. Search PubMed
- Plourde PJ. Travellers’ diarrhea in children. Paediatr Child Health 2003;8:99–103. Search PubMed
- Ahmed T, Bhuiyan TR, Zaman K, Sinclair D, Qadri F. Vaccines for preventing enterotoxigenic Escherichia coli (ETEC) diarrhoea. Cochrane Database Syst Rev 2013;7:CD009029. Search PubMed
- Ritchie ML, Romanuk TN. A meta-analysis of probiotic efficacy for gastrointestinal diseases. PloS One 2012;7:e34938. Search PubMed
- Centers for Disease Control Prevention. Yellow Book. Chapter 2. Travelers’ Diarrhea. Available at wwwnc.cdc.gov/travel/yellowbook/2014/chapter-2-the-pre-travel-consultation/travelers-diarrhea [Accessed 25 November 2014]. Search PubMed
- Wingate D, Phillips SF, Lewis SJ, et al. Guidelines for adults on self-medication for the treatment of acute diarrhoea. Aliment Pharmacol Ther 2001;15:773–82. Search PubMed
- Ericsson CD, DuPont HL, Okhuysen PC, Jiang ZD, DuPont MW. Loperamide plus azithromycin more effectively treats travelers’ diarrhea in Mexico than azithromycin alone. J Travel Med 2007;14:312–19. Search PubMed
- Murphy GS, Bodhidatta L, Echeverria P, et al. Ciprofloxacin and loperamide in the treatment of bacillary dysentery. Ann Intern Med 1993;118:582–86. Search PubMed
- Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis 2007;44:338–46. Search PubMed
- Yung A, Leder K, Torresi J, et al. Manual of Travel Medicine. 3rd edn. Melbourne: IP Communciations, 2011. Search PubMed
- Stermer E, Lubezky A, Potasman I, Paster E, Lavy A. Is traveler’s diarrhea a significant risk factor for the development of irritable bowel syndrome? A prospective study. Clin Infect Dis 2006;43:898–901. Search PubMed
- Expert Group for Antibiotic. Antiobiotic: gastrointestinal tract infections: acute gastroenteritis: acute diarrhoea in special groups: travellers’ diarrhoea. In: eTG Complete [Internet] Melbourne. Therapeutic Guidelines Ltd, 2014. Search PubMed
Also in this issue: Environmental
Professional
Printed from Australian Family Physician - https://www.racgp.org.au/afp/2015/january-february/advising-travellers-about-management-of-travellers © The Australian College of General Practitioners www.racgp.org.au
This website uses cookies to ensure you get the best experience on our website. Learn more

Information on how to stay safe and healthy abroad. About us.
- Disease Prevention Advice
Travellers' Diarrhoea
Introduction.
- Recommendations
Overview of Disease
The illness.
- Additional Preventative Measures
Vaccination
Travellers' diarrhoea is spread mainly through food and water but it can also spread from person to person. It is one of the commonest health problems experienced during travel.
Travellers' diarrhoea usually gets better in 3 to 5 days. Most cases are mild and do not need specific treatment.
- For further information on self-treatment and when to seek medical help, see treatment section below.
Recommendations for Travellers
Preventing travellers' diarrhoea depends mainly upon you practising good hand hygiene and food and water precautions .
- before eating and drinking
- before and after preparing food, particularly raw meat
- after using the toilet or changing nappies
- after visiting food markets
- after touching live animals
- If you cannot wash your hands, use alcohol based sanitiser :
It might be necessary for you to use extra preventive measures in certain situations.
Travellers' diarrhoea is one of the most common health issues experienced during travel.
It can be caused by many different germs like bacteria (E.coli, Salmonella), viruses ( norovirus ) and parasites ( Giardia ). All these germs are spread through eating and drinking contaminated food and water, or using contaminated dishes and cutlery.
Loose poo can also be caused by a change in your diet such as eating oily or spicy foods.
- Travellers’ diarrhoea is when you have 3 or more bouts of loose, watery poo in 24 hours.
- Most cases are mild, but for some people it is severe.
- Travellers' diarrhoea tends to happen in the first week of travel.
- Symptoms last on average 3 to 5 days and usually get better without you needing specific treatment.
Mild travellers’ diarrhoea
Travellers’ diarrhoea is mild if:
- episodes of diarrhoea are not that frequent, they don’t disrupt your activities and any other symptoms are mild
You will usually get better with rest and without specific treatment, but you should make sure you don’t become dehydrated .
Preventing dehydration
When you have diarrhoea, you can lose a lot of water from your body and become dehydrated. Young children can dehydrate quickly.
- These can be bought in pharmacies and supermarkets.
- All rehydrating drinks must be prepared using safe water .
Anti-diarrhoeal Medicine
If diarrhoea is disrupting your plans but is not severe, you can take medicines such as Loperamide (Imodium®) or diphenoxylate plus atropine (Lomotil®). These can help, particularly with tummy pains.
Please note:
- these medicines are not recommended for use in children under 12 years of age
- Imodium® does not work straight away – it might take 1 to 2 hours to help
- taking too much of these medicines might make you constipated
If you develop the following symptoms you should not take anti-diarrhoeal medications and should instead seek medical advice:
- blood or slime (mucous) in your diarrhoea
- a high fever
- severe pain in your stomach
Severe Travellers’ diarrhoea
You should seek medical attention if:
- you cannot continue your normal activities and you have had more than 6 episodes of diarrhoea stools in a 24 hour period, OR
- you have passed blood or mucous (slime) in your diarrhoea, OR
- you keep vomiting, have a fever or severe tummy pain
You might need intravenous fluids to prevent you becoming dehydrated, or antibiotics if an infection is suspected.
Additional Preventive Measures
Tablets to prevent diarrhoea are not routinely recommended as their side effects may be worse than the diarrhoea.
Antibiotics are not routinely recommended to prevent travellers’ diarrhoea:
- widespread use of antibiotics causes resistance to develop in germs, meaning that antibiotics no longer work. This is an increasing problem around the world.
Preventative antibiotics might be offered to some people with severe medical problems that could be made worse by diarrhoea or dehydration. If you feel you may require antibiotics for travel, you should discuss this with your GP or a travel health practitioner.
- All antibiotics have side effects, and can interact with other medicines that you may be taking. You should always read the patient information leaflet that comes with the medicine.
Non-antibiotic medicines
- Bismuth subsalicylate (Pepto-Bismol®, Pepti-calm®)
- Can help to prevent travellers' diarrhoea.
- Available in tablet (Pepto-bismol®) or liquid (Pepto-bismol® or Boots Pepti-calm®).
- Can be bought in pharmacies.
- Can cause blackening of your poo and tongue.
- It may interact with other medicines and is not suitable for everyone.
- You should check with the pharmacist if it is safe for you to take.
- Always follow the dose instructions on the medicine packet.
Pre/Probiotics
Pre- and probiotics are not recommended for either prevention or treatment of travellers' diarrhoea. There is not yet any convincing evidence that they are effective.
No licensed vaccines are available in the UK against travellers' diarrhoea.
back to top
- General Travel Health Advice
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Travelers diarrhea.
Noel Dunn ; Chika N. Okafor .
Affiliations
Last Update: July 4, 2023 .
- Continuing Education Activity
Traveler's diarrhea is a common ailment in individuals traveling to resource-limited destinations overseas. It is estimated to affect nearly 40 to 60 percent of travelers and is the most common travel-associated condition. Bacterial, viral, and parasitic infections can cause symptoms, though bacterial sources represent the most frequent etiology. Although traveler's diarrhea is typically a benign, self-resolving condition, it can lead to dehydration and, in severe cases, significant complications. This activity reviews the evaluation and management of traveler's diarrhea and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
- Identify the causes of traveler's diarrhea.
- Identify strategies to prevent traveler's diarrhea.
- Explain the management of traveler's diarrhea.
- Explain the importance of improving coordination amongst the interprofessional team to enhance care for patients affected by traveler's diarrhea.
- Introduction
Travelers’ diarrhea is a common ailment in persons traveling to resource-limited destinations overseas. Estimates indicate that it affects nearly 40% to 60% of travelers depending on the place they travel, and it is the most common travel-associated condition. Bacterial, viral, and parasitic infections can cause symptoms, though bacterial sources represent the most frequent etiology. While travelers’ diarrhea is typically a benign self-resolving condition, it can lead to dehydration and, in severe cases, significant complications. [1] [2] [3]
The most common bacterial cause is enterotoxigenic Escherichia coli (ETEC), with estimates that the bacteria is responsible for nearly 30% of cases. Other common bacterial causes of travelers’ diarrhea include Campylobacter jejuni , Shigella , and Salmonella species. Norovirus is the most common viral cause while rotavirus is another source of infection. Giardia intestinalis is the most common parasitic source while Cryptosporidium and Entamoeba histolytica can also cause travelers’ diarrhea. The most common cause of travelers’ diarrhea varies by region, though the source is rarely identified in less severe cases. [4] [5] [6]
Traveler's diarrhea can occur in both short and long term travelers; in general, there is no immunity against future attacks. Traveler's diarrhea appears to be most common in warmer climates, in areas of poor sanitation and lack of refrigeration. In addition, the lack of safe water and taking short cuts to preparing foods are also major risk factors. In areas where food handling education is provided, rates of traveler's diarrhea are low.
- Epidemiology
Estimates place the incidence of travelers’ diarrhea at 30% to 60% of travelers to resource-limited destinations. Incidence and causal agent vary by destination, with the highest incidence reported in sub-Saharan Africa. Other locations with high incidence include Latin America, the Middle East, and South Asia. Risk factors are typically related to poor hygiene in resource-limited areas. These include poor hygienic practices in food handling and preparation; lack of refrigeration due to inadequate electrical supply; and poor food storage practices. Additional modifiable risk factors include proton pump inhibitor (PPI) use, recent antibiotic use, and unsafe sexual practices. Risk factors for severe complications are pregnancy, young or old age, travelers with underlying chronic gastrointestinal diseases, or people who are immunocompromised. [7] [8]
- Pathophysiology
Travelers’ diarrhea is most commonly spread by fecal-oral transmission of the causative organism, typically through consumption of contaminated food or water. The incubation period varies by causal agent, with viruses and bacteria ranging from 6 to 24 hours and intestinal parasites requiring 1 to 3 weeks before the onset of symptoms. The pathophysiology for travelers’ diarrhea differs by a causative agent but can be split into non-inflammatory or inflammatory pathways. Non-inflammatory agents cause a decrease in the absorptive abilities of the intestinal mucosa, thereby increasing the output of the gastrointestinal (GI) tract. Inflammatory agents on the other hand cause destruction of the intestinal mucosa either through cytotoxin release or direct invasion of the mucosa. The loss of mucosa surface again results in a decrease of absorption with a resultant increase in bowel movements. [9]
- History and Physical
The onset of symptoms will typically occur 1 to 2 weeks after arrival in a resource-limited destination, though travelers can develop symptoms throughout their stay or shortly after arrival. Travelers’ diarrhea is considered as three or more loose stools in 24 hours or a two-fold increase from baseline bowel habits. Diarrhea often occurs precipitously and is accompanied by abdominal cramping, fever, nausea, or vomiting. Patients should be asked about any blood in their stool, fevers, or any associated symptoms. A thorough travel history should be obtained including timeline and itinerary, diet and water consumption at their destination, illnesses in other travelers, and possible sexual exposures.
In most self-limited cases physical examination will show mild diffuse abdominal tender to palpation. Providers should assess for dehydration through skin turgor and capillary refill. In more severe cases patients may have severe abdominal pain, high fever, and evidence of hypovolemia (tachycardia, hypotension).
Laboratory investigation is typically not required in most cases. In patients with concerning features, such as with high fever, hematochezia, or tenesmus, stool studies can be obtained. Typical stool studies include stool culture, fecal leukocytes, and lactoferrin. The stool should be assessed for ova and parasites in patients with longer duration of symptoms. New multiplex polymerase chain reaction (PCR) screens are becoming available and provide quick analysis of multiple stool pathogens. These screens, however, are expensive, are not widely available, and may not change the clinical management of patients. [4]
Radiological studies are not required in most cases. Kidneys, ureters, and bladder x-ray can be obtained to assess for acute intra-abdominal pathology or look for evidence of perforation in severe cases. An abdominal CT can also be used to assess for intraabdominal pathology in severe cases.
- Treatment / Management
Travelers should be counseled on risk reduction before travel, including avoiding tap water & ice, frequent hand washing, avoiding leafy vegetables or fruit that isn’t peeled, and avoiding street food. Bismuth subsalicylate (two tabs 4 times a day) can be used for prophylaxis and can reduce the incidence of travelers’ diarrhea by almost half, though it should be avoided in children and pregnant women due salicylate side effects. In short high-stakes travel, it may be reasonable to start antibiotics as prophylaxis but is generally avoided in longer-term travel. Rifaximin is a commonly used chemoprophylaxis due to its minimal absorption and minimal side effects. [10] [11] [12]
The foundation of diarrhea management is fluid repletion. In mild cases, travelers should focus on increasing water intake. Water is usually sufficient though sports drinks and other electrolyte fluids can be used. Pedialyte can be used for pediatric patients. Milk and juices should be avoided as this can worsen diarrhea. In more severe cases, oral rehydration salt can be used to ensure rehydration with adequate electrolyte repletion. In cases of severe dehydration, IV fluids may ultimately be required.
Treatment is supportive in mild-moderate cases. In patients without signs of inflammatory diarrhea, loperamide can be used for symptomatic relief. The typical dose for adults is 4 mg initially with 2 mg after each subsequent loose stool, not to exceed 16 mg total in a day.
Also, travelers can be given antibiotics to take as needed at the onset of symptoms. Ciprofloxacin is commonly used for treatment, though there are concerns with resistance with Campylobacter species. For this reason, fluoroquinolones are not often prescribed for travelers to Asia and azithromycin preferable. Also, azithromycin is often prescribed for pregnant travelers and children. A common regimen is 500 mg daily for three days, though evidence suggests that a single dose of 1000 mg may be slightly more effective. Parents can be given azithromycin powder with instructions to mix with water when needed. Rifaximin is a minimally absorbed antibiotic that is also available and is safe for older children and pregnant travelers.
- Differential Diagnosis
- Pseudomembranous colitis
- Ischemic colitis
- Radiation-induced colitis
- Food poisoning
New Guidelines for Traveler's Diarrhea
- Travelers should be advised against the use of prophylactic antibiotics
- In high-risk groups, one may consider antibiotic prophylaxis
- Bismuth subsalicylate can be considered in any traveler.
- The antibiotic of choice is rifaximin
- Fluoroquinolones should not be used as prophylaxis
The outcomes in most patients with traveler's diarrhea are good. However, in severe cases, dehydration can occur requiring admission.
- Complications
- Dehydration
- Malabsorption
- Hemolytic uremic syndrome
- Reactive arthritides
- Postoperative and Rehabilitation Care
The majority of patients are managed as outpatients and need to do the following:
- Maintain hydration
- Hand washing
- Only take antimotility agents if prescribed by the healthcare provider
- Maintain good personal hygiene
- If diarrhea persists for more than 10 days, should follow up with the primary provider
- Deterrence and Patient Education
- Wash hands regularly
- Avoid shellfish from waters that are contaminated
- Wash all foods before consumption
- Drink bottled water when traveling
- Avoid consumption of raw poultry or eggs
- When traveling, consume dry foods and carbonated beverages
- Avoid water and ice from the street
- Avoid drinking water from lakes and rivers
- Pearls and Other Issues
There is a strong correlation with travelers’ diarrhea and the subsequent development of irritable bowel syndrome (IBS), with some studies suggesting up to 50% incidence.
- Enhancing Healthcare Team Outcomes
The key to traveler's diarrhea is preventing it. Today, nurses, the primary care provider and the pharmacists are in the prime position to educate the patient on the importance of hydration and good hygiene. The traveler should be educated on drinking bottled water and washing all fresh fruit and vegetables prior to consumption. Plus, travelers should be warned not to drink from lakes and streams. Carrying small packets of alcohol desansitizer to wash hands can be very helpful when hand washing is not possible.
The pharmacist should educate the traveler on managing the symptoms of diarrhea with over-the-counter medications or loperamide. Travelers should be discouraged from taking prophylactic antibiotics when traveling, as this leads to more harm than good. Finally, the traveler should be educated on the symptoms of dehydration and when to seek medical care. The primary care clinicians should monitor patients until there is a complete resolution of symptoms. Any patient that fails to improve within a few days should be referred to a specialist for further workup. With open communication between the team members, the morbidity of traveler's diarrhea can be reduced. [1] [8] (level V)
The prognosis for most patients with traveler's diarrhea is excellent. However, thousands of patients go to the emergency departments each year looking for a magical cure. Hydration is the key and admission is only required for severe dehydration and orthostatic hypotension. The elderly and children under the age of 4 are at the highest risk for developing complications, which often occur because of self-prescribing of over-the-counter medications. [13] [14] (Level V)
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Noel Dunn declares no relevant financial relationships with ineligible companies.
Disclosure: Chika Okafor declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Dunn N, Okafor CN. Travelers Diarrhea. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Travelers Diarrhea (Nursing). [StatPearls. 2024] Travelers Diarrhea (Nursing). Dunn N, Okafor CN, Knizel JE. StatPearls. 2024 Jan
- Review Travelers' Diarrhea: A Clinical Review. [Recent Pat Inflamm Allergy Dru...] Review Travelers' Diarrhea: A Clinical Review. Leung AKC, Leung AAM, Wong AHC, Hon KL. Recent Pat Inflamm Allergy Drug Discov. 2019; 13(1):38-48.
- Review Travelers' diarrhea. [Curr Opin Infect Dis. 2010] Review Travelers' diarrhea. Hill DR, Beeching NJ. Curr Opin Infect Dis. 2010 Oct; 23(5):481-7.
- Review [Travelers' diarrhea]. [Dtsch Med Wochenschr. 2013] Review [Travelers' diarrhea]. Burchard GD, Hentschke M, Weinke T, Nothdurft HD. Dtsch Med Wochenschr. 2013 Aug; 138(33):1673-83; quiz 1684-6. Epub 2013 Aug 2.
- Review Beyond immunization: travelers' infectious diseases. 1--Diarrhea. [J Egypt Soc Parasitol. 2015] Review Beyond immunization: travelers' infectious diseases. 1--Diarrhea. El-Bahnasawy M, Morsy TA. J Egypt Soc Parasitol. 2015 Apr; 45(1):29-42.
Recent Activity
- Travelers Diarrhea - StatPearls Travelers Diarrhea - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Skip to content
- Accessibility help
Diarrhoea - prevention and advice for travellers
Last revised in September 2023
Travellers' diarrhoea is a clinical syndrome associated with contaminated food or water, that occurs during or shortly after travel
- Scenario: Diarrhoea - prevention and advice for travellers
Background information
- Risk factors
- Complications
Diarrhoea - prevention and advice for travellers: Summary
- Travellers' diarrhoea is defined as passing three or more unformed stools in a 24-hour period with at least one additional symptom, such as abdominal pain or cramps, nausea, vomiting, fever, or blood in the stools.
- Enteric bacteria are the most commonly documented (for example, Escherichia coli, Campylobacter spp., Salmonella spp., and Shigella spp .).
- Viruses and parasites can also cause travellers' diarrhoea.
- Low for people travelling to western European countries, the USA and Canada, Japan, Australia, and New Zealand.
- Intermediate for people travelling to southern European countries, Israel, South Africa, and some Caribbean and Pacific Islands.
- High for people travelling to Africa, Latin America, the Middle East, and most parts of Asia.
- Food hygiene and safe drinking water.
- Self-management and when to seek medical advice if diarrhoea develops during travel.
- The importance of personal hygiene, food hygiene, and safe drinking water should be emphasized.
- Advice regarding the risk of waterborne infection and avoiding contaminated recreational water should be offered.
- Antibiotic prophylaxis or 'stand-by' antibiotic treatment can be considered for certain high-risk travellers. Specialist advice should be sought.
- Most episodes are short-lived and self-limiting, lasting a few days.
- The person could consider purchasing sachets of oral rehydration salt before travelling.
- During an episode of diarrhoea, it is important to prevent dehydration — particularly for young children, pregnant women, elderly people, and those with pre-existing illnesses.
- Both loperamide and bismuth subsalicylate (for example, Pepto-Bismol ® ) may be considered in adults for the relief of mild-to-moderate diarrhoea. They should be used for a maximum of 2 days.
- When to seek medical assistance.
The content on the NICE Clinical Knowledge Summaries site (CKS) is the copyright of Clarity Informatics Limited (trading as Agilio Software Primary Care) . By using CKS, you agree to the licence set out in the CKS End User Licence Agreement .

JOHNNIE YATES, M.D.
Am Fam Physician. 2005;71(11):2095-2100
Patient Information: Seen related handout on traveler’s diarrhea , written by the author of this article.
Acute diarrhea affects millions of persons who travel to developing countries each year. Food and water contaminated with fecal matter are the main sources of infection. Bacteria such as enterotoxigenic Escherichia coli , enteroaggregative E. coli , Campylobacter, Salmonella, and Shigella are common causes of traveler’s diarrhea. Parasites and viruses are less common etiologies. Travel destination is the most significant risk factor for traveler’s diarrhea. The efficacy of pretravel counseling and dietary precautions in reducing the incidence of diarrhea is unproven. Empiric treatment of traveler’s diarrhea with antibiotics and loperamide is effective and often limits symptoms to one day. Rifaximin, a recently approved antibiotic, can be used for the treatment of traveler’s diarrhea in regions where noninvasive E. coli is the predominant pathogen. In areas where invasive organisms such as Campylobacter and Shigella are common, fluoroquinolones remain the drug of choice. Azithromycin is recommended in areas with quinolone-resistant Campylobacter and for the treatment of children and pregnant women.
Acute diarrhea is the most common illness among travelers. Up to 55 percent of persons who travel from developed countries to developing countries are affected. 1 , 2 A study 3 of Americans visiting developing countries found that 46 percent acquired diarrhea. The classic definition of traveler’s diarrhea is three or more unformed stools in 24 hours with at least one of the following symptoms: fever, nausea, vomiting, abdominal cramps, tenesmus, or bloody stools. Milder forms can present with fewer than three stools (e.g., an abrupt bout of watery diarrhea with abdominal cramps). Most cases occur within the first two weeks of travel and last about four days without treatment. 1 , 3 Although traveler’s diarrhea rarely is life threatening, it can result in significant morbidity; one in five travelers with diarrhea is bedridden for a day and more than one third have to alter their activities. 1 , 3
Destination is the most significant risk factor for developing traveler’s diarrhea. 1 – 4 Regions with the highest risk are Africa, South Asia, Latin America, and the Middle East. Travelers who are immunocompromised and those with lowered gastric acidity (e.g., patients taking histamineH 2 blockers or proton pump inhibitors) are more susceptible to traveler’s diarrhea. Recently, a genetic susceptibility has been demonstrated. 5 Younger age and adventurous travel increase the risk of developing traveler’s diarrhea, 3 , 6 but persons staying at luxury resorts or on cruise ships also are at risk. 7 , 8
Food and water contaminated with fecal matter are the main reservoirs for the pathogens that cause traveler’s diarrhea. Unsafe foods and beverages include salads, unpeeled fruits, raw or poorly cooked meats and seafood, unpasteurized dairy products, and tap water. Eating in restaurants increases the probability of contracting traveler’s diarrhea 6 and food from street vendors is particularly risky. 9 , 10 Cold sauces, salsas, and foods that are cooked and then reheated also are risky. 6 , 11
In contrast to the largely viral etiology of gastroenteritis in the United States, diarrhea acquired in developing countries is caused mainly by bacteria 1 , 4 , 6 , 12 ( Table 1 ) . Enterotoxigenic Escherichia coli is the pathogen most frequently isolated, but other types of E. coli such as enteroaggregative E. coli have been recognized as common causes of traveler’s diarrhea. 13 Invasive pathogens such as Campylobacter, Shigella, and non-typhoid Salmonella are relatively common depending on the region, while Aeromonas and non-cholera Vibrio species are encountered less frequently.
Protozoal parasites such as Giardia lamblia , Entamoeba histolytica , and Cyclospora cayetanensis are uncommon causes of traveler’s diarrhea, but increase in importance when diarrhea lasts for more than two weeks. 14 Parasites are diagnosed more frequently in returning travelers because of longer incubation periods (often one to two weeks) and because bacterial pathogens may have been treated with antibiotics. Rotavirus and noroviruses are infrequent causes of traveler’s diarrhea, although noroviruses have been responsible for outbreaks on cruise ships.
The prevalence of specific organisms varies with travel destination. 1 , 4 , 12 , 13 , 15 Available data suggest that E. coli is the predominant cause of traveler’s diarrhea in Latin America, the Caribbean, and Africa, while invasive pathogens are relatively uncommon. Enterotoxigenic E. coli and enteroaggregative E. coli may be responsible for up to 71 percent of cases of traveler’s diarrhea in Mexico. 13 In contrast, Campylobacter is a leading cause of traveler’s diarrhea in Thailand 15 – 17 and also is common in Nepal. 6 Regional variation also exists with parasitic causes of traveler’s diarrhea ( Table 2 ) . 12 , 13 For example, Cyclospora is endemic in Nepal, Peru, and Haiti.
Food poisoning is part of the differential diagnosis of traveler’s diarrhea. Gastroenteritis from preformed toxins (e.g., Staphylococcus aureus , Bacillus cereus ) is characterized by a short incubation period (one to six hours), and symptoms typically resolve within 24 hours. 18 Seafood ingestion syndromes such as diarrhetic shellfish poisoning, ciguatera poisoning, and scombroid poisoning also can cause diarrhea in travelers. These syndromes can be distinguished from traveler’s diarrhea by symptoms such as perioral numbness and reversal of temperature sensation (ciguatera poisoning) or flushing and warmth (scombroid poisoning). 19
Although travelers often are advised to “Boil it, cook it, peel it, or forget it,” data on the effectiveness of dietary precautions in preventing traveler’s diarrhea are inconclusive. 3 , 6 , 20 Many travelers find it difficult to adhere to dietary recommendations. 21 In a study 3 of American travelers, nearly one half developed diarrhea despite pretravel advice on avoidance measures; even persons who strictly followed dietary recommendations developed diarrhea. Avoiding high-risk foods and adventuresome eating behaviors may reduce the inoculum of ingested pathogens or prevent the development of other enteric diseases such as typhoid and hepatitis A and E.
Boiling is the best way to purify water. Iodination or chlorination is acceptable but does not kill Cryptosporidium or Cyclospora, and increased contact time is required to kill Giardia in cold or turbid water. 22 Filters with iodine resins generally are effective in purifying water, although it is uncertain whether the contact time with the resin is sufficient to kill viruses. Bottled water generally is safe if the cap and seal are intact.
DRUG PROPHYLAXIS
Antibiotic prophylaxis is not recommended by the Centers for Disease Control and Prevention (CDC) even for high-risk travelers because it can lead to drug-resistant organisms and may give travelers a false sense of security. Although antibiotic prophylaxis does not prevent viral or parasitic infection, some health care professionals believe that it may be an option for travelers who are at high risk of developing traveler’s diarrhea and related complications (e.g., immunocompromised persons). Prophylaxis with fluoroquinolones is up to 90 percent effective. 23 Rifaximin (Xifaxan) may prove to be the preferred antibiotic because it is not absorbed and is well tolerated, although data on its effectiveness for prophylaxis have not yet been published.
Bismuth subsalicylate (Pepto-Bismol) provides a rate of protection of about 60 percent against traveler’s diarrhea. 24 However, it is not recommended for persons taking anticoagulants or other salicylates. Because bismuth subsalicylate interferes with the absorption of doxycycline (Vibramycin), it should not be taken by travelers using doxycycline for malaria prophylaxis. Travelers should be warned about possible reversible side effects of bismuth subsalicylate, such as a black tongue, dark stools, and tinnitus.
Probiotics are a more natural approach to prophylaxis of traveler’s diarrhea. Probiotics colonize the gastrointestinal tract and theoretically prevent pathogenic organisms from infecting the gut. Studies 25 , 26 of Lactobacillus GG (Culturelle) have suggested protection rates of up to 47 percent. More studies are needed to confirm the efficacy of probiotic prophylaxis. Agents for the prophylaxis of traveler’s diarrhea are summarized in Table 3 .
Empiric Treatment
Counseling travelers about food precautions does not eliminate the risk of traveler’s diarrhea, and nonantibiotic prophylaxis requires frequent dosing to achieve only a modest reduction in risk. In addition, the traveler with diarrhea may have difficulty accessing medical care, the quality of care may be poor, and the quality of medications purchased abroad may be substandard. 27 However, because antibiotics reduce the duration and severity of traveler’s diarrhea and generally are well tolerated, 28 providing the traveler with the means for empiric self-treatment can effectively reduce morbidity from traveler’s diarrhea.
Waiting 24 hours to confirm the diagnosis of traveler’s diarrhea results in unnecessary discomfort and time away from activities. Therapy can be initiated after the first episode of “distressing” diarrhea (i.e., diarrhea that is uncomfortable or interferes with activities). 29 , 30 If symptoms resolve within 24 hours, no further treatment is necessary. 31 , 32 If diarrhea persists after one day, treatment should be continued for one or two more days. An algorithm for the treatment of traveler’s diarrhea is presented in Figure 1 . 33 , 34
Antibiotic selection is based on the likelihood that an invasive organism is present and on antibiotic resistance patterns. These factors are determined largely by travel destination. Although blood in the stool suggests invasive disease, fever is not a sensitive indicator of dysentery. Fluoroquinolones have been the drug of choice for traveler’s diarrhea in most parts of the world because of their efficacy against most enteropathogens. Rifaximin recently became available for the treatment of noninvasive diarrhea caused by E. coli . For persons traveling to destinations where noninvasive E. coli is the predominant pathogen (e.g., Mexico), rifaximin is a good choice. 35 , 36
In regions where invasive pathogens are responsible for a significant proportion of traveler’s diarrhea, quinolones should be used. Azithromycin (Zithromax) is recommended in places where quinoloneresistant Campylobacter is prevalent (e.g., Thailand). 15 , 16 Antibiotics used for the treatment of traveler’s diarrhea are listed in Table 4 . 16 , 32 , 37 Trimethoprim-sulfamethoxazole (Bactrim, Septra) and doxycycline are no longer recommended because of the development of widespread resistance. 12
Therapy that involves an antibiotic with loperamide (Imodium) often limits symptoms to one day. 38 , 39 Loperamide has antimotility and antisecretory effects and is taken as two 2–mg tablets after the first loose stool, followed by one tablet after each subsequent loose stool (maximum of 8 mg in 24 hours for two days). The use of loperamide in dysentery has been controversial because of concerns about prolonging illness, but it is now considered safe when combined with an antibiotic. 29 , 34 , 38 A conservative approach would be to use loperamide for dysentery only if combined with an antibiotic and if the traveler has a long trip or will have no toilet access.
Oral rehydration solutions generally are unnecessary in adults younger than 65 years. 40 However, all travelers with diarrhea should be encouraged to drink plenty of fluids and to replace lost electrolytes using foods such as salt crackers or broth.
Traveler’s Diarrhea in Infants, Children, and Pregnant Women
Traveler’s diarrhea is more common in young children than in adults, and they have a higher risk of dehydration and severe illness. 41 Parents should seek immediate medical attention if their child shows signs of moderate to severe dehydration, bloody diarrhea, a temperature higher than 39°C (102°F), or persistent vomiting. Few data exist on the treatment of diarrhea in children. The use of oral rehydration solutions is essential, and parents should include prepackaged packets (to be mixed with safe water) in their travel kits. These packets are available in camping stores in the United States or in pharmacies in other countries.
Because infants and toddlers normally can have three or more loose stools, an alternate definition of diarrhea in this age group is a twofold increase in the frequency of unformed stool. 37 Nursing infants should continue to breastfeed on demand, and infants and older children should be offered their usual food.
Fluoroquinolones are not approved by the U.S. Food and Drug Administration (FDA) for use in children, and rifaximin is approved only for children 12 years and older. Therefore, azithromycin is the drug of choice for most children with traveler’s diarrhea. 37 Another option is nalidixic acid (Neggram) in a dosage of 55 mg per kg per day divided into four doses, not to exceed 1 g in 24 hours. 37 Loperamide is approved for children older than two years, but should not be used in children with dysentery. Bismuth subsalicylate should be avoided for prophylaxis in children because of the possible risk of Reye’s syndrome.
Pregnant women may be at higher risk of traveler’s diarrhea than nonpregnant women because of lowered gastric acidity and increased gastrointestinal transit time. 42 Quinolones (FDA pregnancy category C) generally are not advised during pregnancy, but azithromycin (FDA pregnancy category B) is safe. Oral rehydration should be emphasized. Although rifaximin is not absorbed, the safety of this medication in pregnant women has not been established. Loperamide (FDA pregnancy category B) may be used, but bismuth subsalicylate (FDA pregnancy category D) should be avoided. Being careful with food and water is particularly important during pregnancy because infections such as listeriosis can cause miscarriage, and hepatitis E can result in maternal mortality.
Complications
Dehydration is the main complication of traveler’s diarrhea, especially in children and older adults. Because E. coli O157:H7 is a rare cause of traveler’s diarrhea, there is little risk of hemolyticuremic syndrome. Other complications include Guillain-Barré syndrome after Campylobacter enteritis, Reiter’s syndrome (especially in persons who are HLA-B27 positive), Clostridium difficile colitis after antibiotic use, and postinfectious irritable bowel. These conditions may appear after the traveler has returned home.
If diarrhea persists despite antibiotic treatment, medical attention should be sought. Parasitic causes should be suspected in travelers who return with prolonged diarrhea or who do not respond to antibiotics. For those traveling to remote areas for extended periods, it is reasonable to discuss empiric treatment of protozoal infections (e.g., metronidazole [Flagyl] 250 mg three times a day for five days or tinidazole [Fasigyn] in a single 2–g dose for Giardia). 43
Resources such as the Travelers’ Health section of the CDC Web site ( http://www.cdc.gov/travel/diarrhea.htm ) or commercial sites such as Travel Health Online ( http://www.tripprep.com ) can keep physicians up to date on the epidemiology and resistance patterns of traveler’s diarrhea. Better preventive and prophylactic strategies will be needed until newer antibiotics become available and the sanitation and hygiene in developing countries improve.
von Sonnenburg F, Tornieporth N, Waiyaki P, Lowe B, Peruski LF , DuPont HL, et al. Risk and aetiology of diarrhoea at various tourist destinations.. Lancet. 2000;356:133-4.
Castelli F, Pezzoli C, Tomasoni L. Epidemiology of travelers’ diarrhea.. J Travel Med. 2001;8(suppl 2):S26-S30.
Hill DR. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to developing countries.. Am J Trop Med Hyg. 2000;62:585-9.
Steffen R, Sack RB. Epidemiology. In: Ericsson CD, DuPont HL, Steffen R, eds. Travelers’ diarrhea. Hamilton, Ont.: BC Decker, 2003:112–23.
Jiang ZD, Okhuysen PC, Guo DC, He R, King TM, DuPont HL, et al. Genetic susceptibility to enteroaggregative Escherichia coli diarrhea: polymorphism in the interleukin–8 promotor region.. J Infect Dis. 2003;188:506-11.
Hoge CW, Shlim DR, Echeverria P, Rajah R, Herrmann JE, Cross JH. Epidemiology of diarrhea among expatriate residents living in a highly endemic environment. JAMA. 1996;275:533-8.
Hardie RM, Wall PG, Gott P, Bardhan M, Bartlett LR. Infectious diarrhea in tourists staying in a resort hotel.. Emerg Infect Dis. 1999;5:168-71.
Daniels NA, Neimann J, Karpati A, Parashar UD, Greene KD, Wells JG, et al. Traveler’s diarrhea at sea: three outbreaks of waterborne enterotoxigenic Escherichia coli on cruise ships.. J Infect Dis. 2000;181:1491-5.
Ansdell VE, Ericsson CD. Prevention and empiric treatment of traveler’s diarrhea.. Med Clin North Am. 1999;83:945-73
Mensah P, Yeboah-Manu D, Owusu-Darko K, Ablordey A. Street foods in Accra, Ghana: how safe are they?. Bull World Health Organ. 2002;80:546-54.
Adachi JA, Mathewson JJ, Jiang ZD, Ericsson CD, DuPont HL. Enteric pathogens in Mexican sauces of popular restaurants in Guadalajara, Mexico, and Houston, Texas.. Ann Intern Med. 2002;136:884-7.
Jiang ZD, Lowe B, Verenkar MP, Ashley D, Steffen R, Tornieporth N, et al. Prevalence of enteric pathogens among international travelers with diarrhea acquired in Kenya (Mombasa), India (Goa), or Jamaica (Montego Bay).. J Infect Dis. 2002;185:497-502.
Adachi JA, Jiang ZD, Mathewson JJ, Verenkar MP, Thompson S, Martinez-Sandoval F, et al. Enteroaggregative Escherichia coli as a major etiologic agent in traveler’s diarrhea in 3 regions of the world.. Clin Infect Dis. 2001;32:1706-9.
Taylor DN, Houston R, Shlim DR, Bhaibulaya M, Ungar BL, Echeverria P. Etiology of diarrhea among travelers and foreign residents in Nepal.. JAMA. 1988;260:1245-8.
Kuschner RA, Trofa AF, Thomas RJ, Hoge CW, Pitarangsi C, Amato S, et al. Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent.. Clin Infect Dis. 1995;21:536-41.
Hoge CW, Gambel JM, Srijan A, Pitarangsi C, Echeverria P. Trends in antibiotic resistance among diarrheal pathogens isolated in Thailand over 15 years.. Clin Infect Dis. 1998;26:341-5.
Sanders JW, Isenbarger DW, Walz SE, Pang LW, Scott DA, Tamminga C, et al. An observational clinic-based study of diarrheal illness in deployed United States military personnel in Thailand: presentation and outcome of Campylobacter infection.. Am J Trop Med Hyg. 2002;67:533-8.
Tauxe RV, Swerdlow DL, Hughes JM. Foodborne disease. In: Mandell GL, Douglas RG, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and practice of infectious diseases. 5th ed. Philadelphia: Churchill Livingstone, 2000:1150–65.
Barbier HM, Diaz JH. Prevention and treatment of toxic seafoodborne diseases in travelers.. J Travel Med. 2003;10:29-37.
Kozicki M, Steffen R, Schar M. ‘Boil it, cook it, peel it or forget it’: does this rule prevent travellers’ diarrhoea?. Int J Epidemiol. 1985;14:169-72.
Mattila L, Siitonen A, Kyronseppa H, Simula II, Peltola H. Risk behavior for travelers’ diarrhea among Finnish travelers.. J Travel Med. 1995;2:77-84.
Backer H. Water disinfection for international and wilderness travelers.. Clin Infect Dis. 2002;34:355-64.
RendiWagner P, Kollaritsch H. Drug prophylaxis for travelers’ diarrhea.. Clin Infect Dis. 2002;34:628-33.
Steffen R, Heusser R, DuPont HL. Prevention of travelers’ diarrhea by nonantibiotic drugs.. Rev Infect Dis. 1986;8(suppl 2):S151-9.
Oksanen PJ, Salminen S, Saxelin M, Hamalainen P, Ihantola-Vormisto A, Muurasniemi-Isoviita L, et al. Prevention of travellers’ diarrhoea by Lactobacillus GG.. Ann Med. 1990;22:53-6.
Hilton E, Kolakowski P, Singer C, Smith M. Efficacy of Lactobacillus GG as a diarrheal preventive in travelers.. J Travel Med. 1997;4:41-3.
World Health Organization. Substandard and counterfeit medicines. Fact sheet no. 275, November 2003. Accessed online April 6, 2005, at: http://www.who.int/mediacentre/factsheets/2003/fs275 .
De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea.. Cochrane Database Syst Rev. 2005;;1:CD002242.
Shlim DR. Self diagnosis and treatment of traveler’s diarrhea. In: Keystone JS, Kozarsky PE, Freedman DO, Nothdurft HD, Connor BA, eds. Travel medicine. St. Louis: Mosby, 2003:201–4.
Ericsson CD. Travelers’ diarrhea: epidemiology, prevention, and self-treatment.. Infect Dis Clin North Am. 1998;12:285-303.
Salam I, Katelaris P, Leigh-Smith S, Farthing MJ. Randomised trial of singledose ciprofloxacin for travellers’ diarrhoea.. Lancet. 1994;344:1537-9.
Adachi JA, Ericsson CD, Jiang ZD, DuPont MW, Martinez-Sandoval F, Knirsch C, et al. Azithromycin found to be comparable to levofloxacin for the treatment of US travelers with acute diarrhea acquired in Mexico.. Clin Infect Dis. 2003;37:1165-71.
DuPont HL, Mattila L. Antimicrobial treatment: an algorithmic approach. In: Ericsson CD, DuPont HL, Steffen R, eds. Travelers’ diarrhea. Hamilton, Ont.: BC Decker, 2003:227–37.
Adachi JA, OstroskyZeichner L, DuPont HL, Ericsson CD. Empirical antimicrobial therapy for traveler’s diarrhea.. Clin Infect Dis. 2000;31:1079-83.
DuPont HL, Jiang ZD, Ericsson CD, Adachi JA, Mathewson JJ, DuPont MW, et al. Rifaximin versus ciprofloxacin for the treatment of traveler’s diarrhea: a randomized, double-blind clinical trial.. Clin Infect Dis. 2001;33:1807-15.
Steffen R, Sack DA, Riopel L, Jiang ZD, Sturchler M, Ericsson CD, et al. Therapy of travelers’ diarrhea with rifaximin on various continents.. Am J Gastroenterol. 2003;98:1073-8.
Stauffer WM, Konop RJ, Kamat D. Traveling with infants and young children. Part III: travelers’ diarrhea.. J Travel Med. 2002;9:141-50.
Murphy GS, Bodhidatta L, Echeverria P, Tansuphaswadikul S, Hoge CW, Imlarp S, et al. Ciprofloxacin and loperamide in the treatment of bacillary dysentery.. Ann Intern Med. 1993;118:582-6.
Taylor DN, Sanchez JL, Candler W, Thornton S, McQueen C, Echeverria P. Treatment of travelers’ diarrhea: ciprofloxacin plus loperamide compared with ciprofloxacin alone. A placebo-controlled randomized trial.. Ann Intern Med. 1991;114:731-4.
Caeiro JP, DuPont HL, Albrecht H, Ericsson CD. Oral rehydration therapy plus loperamide versus loperamide alone in the treatment of traveler’s diarrhea.. Clin Infect Dis. 1999;28:1286-9.
Pitzinger B, Steffen R, Tschopp A. Incidence and clinical features of traveler’s diarrhea in infants and children.. Pediatr Infect Dis J. 1991;10:719-23.
Samuel BU, Barry M. The pregnant traveler.. Infect Dis Clin North Am. 1998;12:325-54.
Drugs for parasitic infections. Med Lett Drugs Ther. 2004;46:1-12.
Continue Reading
More in afp.
Copyright © 2005 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
IMAGES
VIDEO
COMMENTS
Travelers' Diarrhea. Travelers' diarrhea is the most common travel-related illness. It can occur anywhere, but the highest-risk destinations are in Asia (except for Japan and South Korea) as well as the Middle East, Africa, Mexico, and Central and South America. In otherwise healthy adults, diarrhea is rarely serious or life-threatening, but it ...
Lifestyle and home remedies. If you do get traveler's diarrhea, avoid caffeine, alcohol and dairy products, which may worsen symptoms or increase fluid loss. But keep drinking fluids. Drink canned fruit juices, weak tea, clear soup, decaffeinated soda or sports drinks to replace lost fluids and minerals.
Episodes of travelers' diarrhea are nearly always benign and self-limited, but symptoms may disrupt planned activities and result in health care visits for some travelers . There is a growing recognition that travelers' diarrhea and its self-treatment abroad are associated with the acquisition of organisms harboring antibiotic resistance [ 5-10 ].
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant. When you visit a place where the climate or sanitary practices are ...
Traveler's diarrhea affects travelers and others who consume contaminated food or water. It's a brief but unpleasant gastrointestinal infection that typically causes loose stools and abdominal cramps. Most of the time, it's caused by bacteria, but sometimes viruses or parasites are to blame. International travelers are most at risk when ...
Traveller's diarrhoea. Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. It is caused by consuming food and water, contaminated by germs (microbes) including bacteria, viruses and parasites. Other symptoms can include high temperature (fever), being sick (vomiting) and tummy (abdominal) pain.
410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Diarrhea is the term for bowel movements that are loose or watery. Traveler's diarrhea occurs within 10 days of travel to an area with poor public hygiene. It's the most common illness in travelers.
Fever. Nausea and vomiting. Bloating. Urgent need to have a bowel movement. Malaise (weakness or discomfort) Explosive and painful gas. Stomach c ramps. Loss of appetite. Traveler's diarrhea ...
Traveler's diarrhea can turn a trip into a nightmare. Food and water contaminated by germs, also known as pathogens, is not uncommon in certain areas of the world that are popular travel destinations.Consuming even small amounts of these germs can cause loose, watery stool, the main sign of diarrhea, Luckily, treatment options are available.
In 50-80% of TD cases, TD is caused by bacterial infection. Mild diarrhoea can be managed with an antimotility agent (loperamide) alone, but for moderate or severe diarrhoea, early self-treatment with loperamide in conjunction with antibiotics is advised. Recommended empirical antibiotics are fluoroquinolones (norfloxacin / ciprofloxacin) or ...
The Illness. Travellers' diarrhoea is when you have 3 or more bouts of loose, watery poo in 24 hours. Most cases are mild, but for some people it is severe. Travellers' diarrhoea tends to happen in the first week of travel. Symptoms last on average 3 to 5 days and usually get better without you needing specific treatment.
For example, without treatment bacterial or viral diarrhea may last for a few days, while protozoal diarrhea can persist for weeks or months. ... (2019). Travelers' diarrhea: Update on the ...
Travelers' diarrhea is a common ailment in persons traveling to resource-limited destinations overseas. Estimates indicate that it affects nearly 40% to 60% of travelers depending on the place they travel, and it is the most common travel-associated condition. Bacterial, viral, and parasitic infections can cause symptoms, though bacterial sources represent the most frequent etiology.
Diarrhoea - prevention and advice for travellers: Summary. Travellers' diarrhoea is defined as passing three or more unformed stools in a 24-hour period with at least one additional symptom, such as abdominal pain or cramps, nausea, vomiting, fever, or blood in the stools.
Travelers diarrhea. Epidemiology, prevention, and self-treatment. Infect Dis Clin North Am. 1998;12:285-303. Kuschner RA, Trofa AF, Thomas RJ, Hoge CW, Pitarangsi C, Amato S, et al. Use of ...
Most cases occur within the first two weeks of travel and last about four days without treatment. 1, 3 Although traveler's diarrhea rarely is life threatening, it can result in significant ...
In addition to diarrhea, they usually include fever, nausea, vomiting, bloating, abdominal cramping and an urgent need to use the bathroom. Generally, the symptoms go away in a few days without treatment. In more severe and rare cases, travellers' diarrhea can lead to dehydration and death. This is a particular concern for children, the elderly ...
Istra is famous for its New Jerusalem Monastery which was established to serve as a Russian version of the Holy Land. Today the monastery has been completely restored following the damage it suffered at the hands of the Nazis and Bolsheviks, and remains the main reason for visiting Istra. The city can easily be visited as a day trip from Moscow.
Many travellers enjoy visiting Usadba Altufyevo (7.6 miles) and House of the Lukutin merchants (5.2 miles). See all nearby attractions. Hotel Gosti, Lobnya, Moscow Oblast: See traveller reviews, candid photos, and great deals for Hotel Gosti at Tripadvisor.
Contacts Warehouse and Оffice. Industrial Park Sheremetyevo. 141400, Moscow Oblast, Khimki city, Klyazma area, 1g. Phone: +7 (495) 6519231 Fax: +7 (495) 6519232
Lobnya is a town in Moscow Oblast, Russia, located 30 kilometres north west of Moscow. Lobnya has about 84,200 residents. Mapcarta, the open map.