Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
The treatment and prevention of travelers' diarrhea are discussed here. The epidemiology, microbiology, clinical manifestations, and diagnosis of travelers' diarrhea are discussed separately. (See "Travelers' diarrhea: Epidemiology, microbiology, clinical manifestations, and diagnosis" .)
Clinical approach — Management of travelers’ diarrhea depends on the severity of illness. Fluid replacement is an essential component of treatment for all cases of travelers’ diarrhea. Most cases are self-limited and resolve on their own within three to five days of treatment with fluid replacement only. Antimotility agents can provide symptomatic relief but should not be used when bloody diarrhea is present. Antimicrobial therapy shortens the disease duration, but the benefit of antibiotics must be weighed against potential risks, including adverse effects and selection for resistant bacteria. These issues are discussed in the sections that follow.
When to seek care — Travelers from resource-rich settings who develop diarrhea while traveling to resource-limited settings generally can treat themselves rather than seek medical advice while traveling. However, medical evaluation may be warranted in patients who develop high fever, abdominal pain, bloody diarrhea, or vomiting. Otherwise, for most patients while traveling or after returning home, medical consultation is generally not warranted unless symptoms persist for 10 to 14 days.
Fluid replacement — The primary and most important treatment of travelers' (or any other) diarrhea is fluid replacement, since the most significant complication of diarrhea is volume depletion [ 11,12 ]. The approach to fluid replacement depends on the severity of the diarrhea and volume depletion. Travelers can use the amount of urine passed as a general guide to their level of volume depletion. If they are urinating regularly, even if the color is dark yellow, the diarrhea and volume depletion are likely mild. If there is a paucity of urine and that small amount is dark yellow, the diarrhea and volume depletion are likely more severe.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Pharm J (Ott)
- v.152(4); Jul-Aug 2019
Travelers’ diarrhea: Clinical practice guidelines for pharmacists
Introduction.
Travelers’ diarrhea (TD) is the most common travel-related illness, affecting up to 70% of travelers to certain destinations. 1 Its etiology is predominantly bacterial, representing approximately 80% to 90% of illnesses, 1 including diarrheagenic Escherichia coli, Salmonella, Shigella and Campylobacter species, but it can also be caused by parasites, such as Giardia and Cryptosporidium , and viruses, such as norovirus. 1 , 2 Opportunity costs, changes to trip itineraries and seeking medical care abroad are just some of the consequences that can result from a bout of TD. Emerging data have affected the recommendations for the prevention and treatment of TD, resulting in the publication of a set of guidelines for the condition in a 2017 supplement to the Journal of Travel Medicine . 3 As highly accessible experts in pharmacotherapy, pharmacists are well positioned to address travel-related concerns, particularly regarding TD, at both the prescription counter and over-the-counter (OTC) aisle. Pharmacists can draw from the guidelines to ensure patients are counselled on safe and appropriate antibiotic therapy during international travel and can direct patients to important nonprescription products supported by the guidelines and provide advice on their safe and effective use. This article summarizes the key recommendations from the 2017 guidelines of interest to practising community pharmacists. Readers requiring additional information are encouraged to consult the full guideline publication. 3
Development of the guidelines
The International Society of Travel Medicine (ISTM) used a panel of experts with relevant experience in the disease’s management to formulate the Guidelines for the Prevention and Treatment of Travelers’ Diarrhea: A Graded Expert Panel Report. Despite ISTM not having a designated process and resources to develop clinical practice guidelines, the panel members attempted to follow the Institute of Medicine guideline standards and Grades of Recommendations, Assessment, Development and Evaluation (GRADE) framework. 3 Each recommendation in the guideline underwent the same procedures: “Recommendation formulation [with a threshold of 80% agreement among panel members], grading the quality of evidence in terms of the confidence in the estimates of the efficacy and harms of the intervention and grading the strength of the recommendation based on the balance of harms and benefits and knowledge of the values and preferences of the travelers.” 3 Prior to publication, the manuscript was peer-reviewed by experts in infectious diseases and travel medicine who were not involved in the development of the guidelines. Readers seeking additional details on guideline development are referred to the Journal of Travel Medicine . 3
TD definitions
TD has previously been classified quantitatively, based on the number of loose bowel movements experienced in a day (e.g., mild = 1-2 stools/24 hours, moderate = 3-5 stools/24 hours and severe = 6-9 stools/24 hours). 4 , 5 Classification is now qualitative, based on the functional impact TD has on the patient and his or her ability to participate in activities planned during travel ( Table 1 ).
Classifications of travelers’ diarrhea
Patients should be counselled on these definitions in order to properly recognize when to begin self-treatment and which treatments should be used (discussed below). It is important to emphasize the “functional impact” when educating, so that travelers can recognize the form of illness they are experiencing. For example, 1 episode with severe fever, cramping and bloody stools may be more impairing than 4 unformed stools without any other symptoms. Furthermore, as severe dysentery TD is typically accompanied by a fever, and traveling patients will likely not be carrying a thermometer, pharmacists should discuss its symptomatology so that patients can recognize this severe form of illness. Pharmacists should advise patients to seek medical assessment for TD lasting longer than 14 days, as persistent diarrhea may be associated with a higher frequency of certain bacteria, protozoal pathogens or other noninfectious conditions that may require targeted diagnosis and treatment.
TD prophylaxis
Antimicrobial resistance is a serious global health issue, necessitating the judicious use of antibiotics. For most travelers, antibiotics should not routinely be used for TD prophylaxis. However, antimicrobial prophylaxis can be considered for patients at a high risk for complications secondary to TD, such as those who have a clinically significant history of potential additional morbidity following an enteric infection (e.g., inflammatory bowel disease, reactive arthritis) or a chronic illness that predisposes them to TD (e.g., achlorhydria, gastrectomy) or its complications (e.g., immunocompromised, diabetes, renal dysfunction). 3 Other individuals who may be considered for TD prophylaxis include travelers who cannot afford to become sick with TD due to occupation or itinerary reasons (e.g., athlete in competition, musician, politician). 3 Because of the rapid efficacy of TD self-treatment and increasing rates of antimicrobial resistance, individual risk-benefit assessments and appropriate counselling must be performed before considering prophylaxis.
TD prophylaxis can be employed without antibiotics through the use of bismuth subsalicylate. Doses of 2.1 g/day or 4.2 g/day in 4 divided doses (with meals and bedtime) in either the liquid or tablet form have been studied and demonstrated a consistent protective effect against TD, upwards of 60%. 6 - 8 Despite robust evidence, its adverse effects, most commonly including black tongue and stools and least commonly being tinnitus, can be undesirable for traveling patients. 6 In addition, its contraindications in pediatric, pregnant, aspirin-allergic and aspirin-taking patients limit its use in the prevention of TD, and its frequent dosing may also affect adherence.
If antibiotic prophylaxis is warranted in a traveling patient, rifaximin is advised, 3 based on strong evidence of effectiveness, minimal antimicrobial resistance (excluding Campylobacter spp.) and favourable safety profile, as it is not systemically absorbed. Because of its resistance to Campylobacter spp., its effectiveness may not be as assured in South and Southeast Asia, where Campylobacter infection is more common. While 600 mg orally once daily is the standard prophylaxis dose for rifaximin, readers should be aware that it is currently available only in Canada as 550 mg tablets. The Committee to Advise on Tropical Medicine and Travel guidelines do not consider this difference in dose to be clinically significant 9 and therefore recommend that a regimen of 550 mg once daily can be used by Canadian travelers. The trials supporting rifaximin’s strong prophylactic protection against TD used a range of dosing regimens, from 200 mg to 1100 mg divided 1 to 3 times daily. 10 - 14 However, because of the risk of missing doses and the observed rebound infection following discontinuation of the drug, some clinicians advocate for a twice-daily regimen (200 mg or 550 mg) based on expert opinion. It should also be noted that effectiveness and safety have not been demonstrated beyond 2 weeks in multiple trials and thus may represent the best solution for short-term protection when needed. 15
Although they have long been prescribed for prophylaxis, fluoroquinolones are no longer recommended for prophylaxis of TD because of the emerging resistance of enteric pathogens. The use of fluoroquinolones exposes patients to potential harm to the peripheral and central nervous system, tendons, muscles and joints, as well as the possibility of Clostridium difficile –associated diarrhea. Therefore, based on its high-risk and low-benefit profile, the guidelines do not recommend the use of fluoroquinolones in TD prophylaxis. In addition, recommendations regarding azithromycin’s prophylactic use have not been determined in the 2017 guidelines. 3
Pharmacists are reminded to encourage patients to also practise food and water precautions to minimize their risk of exposure to TD-causing organisms. Frequent handwashing, especially prior to meals, with warm soap and water or the use of an alcohol-based hand sanitizer with ≥60% alcohol is recommended. 16 It is safest to eat food that is fully cooked and served hot, as raw or undercooked meals containing meat and fish are likely to be contaminated. 16 When selecting foods to eat abroad where hygiene and sanitation are inadequate or unknown, travelers should also be advised to avoid unpasteurized fruit juices, milks or cheeses, produce washed in local water sources and raw fruits that are unpeeled (e.g., strawberries), as opposed to fruits that are peeled by the traveler (e.g., bananas and mangoes). 16 Commercially bottled water with a preserved seal should be recommended for drinking, preparing food and beverages, making ice and brushing teeth. 16
Therapy for mild TD
Most cases of TD can be classified as mild: otherwise tolerable, nondistressing and does not interfere with planned activities. Because of increasing antimicrobial resistance and concerns regarding multidrug-resistant organisms, antibiotic conservation is advised. Therefore, antibiotic treatment is not recommended in patients with mild TD. Instead, supportive measures such as oral rehydration therapy and nonantibiotic, antimotility drugs such as loperamide can be used. Loperamide’s use in mild TD has been shown to decrease the duration of diarrhea and the frequency of passing unformed stools. 17 - 19 Although previously discouraged for TD treatment because of its antimotility effects and concerns about potential retention of pathogens in the gut, a number of observational studies support the safe and effective use of loperamide in the treatment of mild TD. 20 , 21
Loperamide and bismuth subsalicylate are the 2 OTC products with the most supportive evidence, with stronger evidence favoring loperamide over bismuth subsalicylate. 17 Other agents, such as activated charcoal or dimenhydrinate, are not recommended. Although loperamide is the recommended first-line agent, patients should be informed that if the diarrhea worsens or is accompanied by moderate-severe or invasive symptoms (1 or more of fever, moderate to severe abdominal pain or bloody diarrhea), then antibiotics should be used ( Table 2 ). To ensure ready access to antibiotic treatment if required while traveling, prescriptions should be dispensed to most travelers in advance of their departure. Filling medications at a Canadian pharmacy also prevents the exhaustion of the destination country’s medication supply and prevents the possible ingestion of international substandard or falsified medications. 22
Summary of treatment recommendations based on Canadian product availability
po, orally.
Therapy for moderate TD
TD can affect both a traveler’s well-being and finances, as illness may require the rebooking of flights, cancellation of major excursions and missing activities on the traveler’s itinerary. Patients with moderate illness may be treated with antibiotics, with or without adjunctive loperamide. Timely and effective self-treatment with antibiotics in moderate TD reduces the duration of illness to approximately 36 hours, with further reduction to less than 12 hours from combination therapy with loperamide. 9 , 23 - 25 Potential risks from antibiotic therapy, including the potential for acquisition of extended-spectrum beta-lactamase–producing Enterobacteriaceae (ESBL-PE) and C. difficile infection, must be weighed for each individual traveler against the benefits: (1) potentially favourable safety profiles from single-dose regimens and (2) theoretical mitigation of risk of developing long-term TD sequelae such as postinfectious irritable bowel syndrome. 20 , 26 - 30 However, more studies evaluating the nature and impact of these theoretical risks and benefits are needed.
Several class- and regimen-specific factors should be considered when choosing an antibiotic. Despite observational data of globally increasing resistance rates, 31 fluoroquinolones may still be used in the treatment of moderate TD. However, their use should be avoided in Southeast and South Asia, as widespread resistance, particularly against Campylobacter spp., has resulted in documented clinical failure. 32 These resistance rates and safety concerns regarding their potential for intestinal microbiota imbalance and musculoskeletal consequences have resulted in a nonunanimous recommendation by the guideline’s expert panel. Canadian readers should note that while ofloxacin is a fluoroquinolone listed for TD treatment in the guidelines, it is not currently marketed in an oral formulation in Canada. As an alternative to fluoroquinolones, azithromycin may also be considered for moderate TD, as studies indicate there is no significant difference in efficacy between azithromycin and fluoroquinolones. 9 However, it should be noted that as the TD classification changes from moderate to severe, the 2017 guidelines prefer azithromycin as the primary treatment option (discussed below). 3 Apart from concerns in Nepal, azithromycin has limited global resistance, and despite requiring increased concentrations to inhibit enterotoxigenic and enteroaggregative E. coli (ETEC and EAEC, respectively), this has not yet resulted in documented clinical failure. It also has a much more tolerable safety profile compared with fluoroquinolones, with the exception of nausea and vomiting, particularly when the single dose of 1000 mg is ingested. However, both azithromycin and fluoroquinolones potentially expose certain patients to the risk of QT prolongation and must be carefully considered for patients at risk of this, including those with a QTc interval >500 ms, advanced age, female sex and concomitant QTc-prolonging medications, such as some antidepressants and antipsychotics. 33
Finally, the guidelines also recommend rifaximin as another alternative for moderate TD. However, as the only rifaximin products currently licensed in Canada are 550 mg tablets, and the splitting of tablets is not recommended by the manufacturer, 34 product availability prevents Canadian patients from accessing the recommended treatment dose of 200 mg 3 times daily unless they purchase it abroad. As a poorly absorbed antibiotic, it has an excellent safety profile and limited global resistance rates; however, its use is cautioned for travel to regions with a high risk of invasive pathogens, such as Campylobacter, Shigella and Salmonella , because of its poor clinical success against these species. 35 , 36 A recent trial evaluating single high-dose rifaximin (1650 mg) in combination with loperamide was found to be comparable to single-dose levofloxacin (500 mg) and azithromycin (500 mg), with clinical cures of about 14 hours. 37
As mentioned previously, loperamide may be used either in combination therapy with antibiotics or as monotherapy for moderate TD. Its quick onset when used with antibiotics provides symptomatic relief in addition to curative treatment. Concerns about adverse effects, including disruption of the diversity of intestinal flora and ESBL-PE colonization, surrounding combination therapy remain unsubstantiated. Despite the apprehension of increasing a TD patient’s exposure to pathogens when motility is slowed, loperamide’s studied effectiveness has led to its safe recommendation as a solo therapy in nonsevere TD. 3 Other than constipation, which may occur from patients taking doses at too frequent intervals (patients should be advised that it has an onset of action of up to 1-2 hours), it is a well-tolerated agent. Combination therapy with loperamide has consistently demonstrated an advantage in time to clinical cure compared with antibiotics alone.
BOX 1 Key points regarding travelers’ diarrhea for pharmacists
The release of the 2017 guidelines for the prevention and treatment of travelers’ diarrhea has resulted in significant changes in the management of travelers’ diarrhea, many of which affect community pharmacy practice. The key points of interest to pharmacists are summarized here:
- • Classification of TD
- ○ TD severity should be based on a patient’s self-determination:
- □ Mild : Tolerable, nondistressing and does not interfere with planned activities
- □ Moderate : Distressing or interfering with planned activities
- □ Severe : Incapacitating or completing stopping all planned activities, including dysentery and nondysentery presentations
- □ Persistent : Diarrhea lasting ≥2 weeks
- • TD prophylaxis
- ○ Prophylaxis is not routinely used but can be considered for patients at high risk of health-related complications secondary to TD such as:
- □ prior clinically significant history of potential additional morbidity following an enteric infection (e.g., inflammatory bowel disease, reactive arthritis) and
- □ chronic illness that predisposes patient to TD (e.g., achlorhydria, gastrectomy) or its complications (e.g., immunocompromised, diabetes, renal dysfunction).
- ○ Prophylaxis may be considered for travelers who cannot afford to become sick with TD because of their occupation or itinerary reasons (e.g., athlete in competition, musician, politician).
- □ Bismuth subsalicylate may be considered for most travelers as prophylaxis.
- □ If antibiotic prophylaxis is indicated, rifaximin is the recommended agent.
- • Mild TD
- ○ Patients can use loperamide for the treatment of mild TD to decrease the duration of diarrhea and frequency of passing unformed stool.
- • Moderate TD
- ○ Functional impairment and itinerary changes are the main factors to consider when using self-determining to use antibiotics for moderate TD.
- □ Antibiotic treatment options available in Canada are azithromycin and fluoroquinolones (when traveling outside of Southeast Asia).
- □ Because of emerging global resistance and efficacy, pharmacists may notice a shift in prescribing practices, in which azithromycin is used as the first-line treatment for both moderate and severe TD.
- ○ Loperamide can be used either alone or as an adjunct to antibiotics.
- • Severe TD
- ○ Travelers should be educated on how to self-diagnose dysentery (presence of blood in the stool, possibly accompanied by fever and/or abdominal pain) to determine appropriate treatment measures.
- ○ Antibiotics should be used for severe travelers’ diarrhea, both dysentery and nondysentery, with azithromycin being the antibiotic of choice.
- □ Loperamide may also be used as an adjunct to azithromycin, in the absence of dysentery.
Therapy for severe TD
Severe TD includes both nondysenteric watery diarrhea affecting a traveler’s quality of life and dysentery. Both presentations are important to consider and discern as this guides the antibiotic management options. The main distinction between the 2 types of severe diarrhea is the presence of blood in the stool (possibly accompanied by fever and/or abdominal pain), as this depicts the hallmark clinical presentation of dysentery.
BOX 2 Resources for additional information regarding travelers’ diarrhea and other travel-related concerns
- • International Society of Travel Medicine ( www.istm.org/ )
- ○ ISTM offers a Certificate in Travel Health (CTH) to health care practitioners who have developed competency in providing travel medicine services. Pharmacists interested in expanding their knowledge and providing more comprehensive travel medicine services are encouraged to write the CTH examination.
- • Committee to Advise on Tropical Medicine and Travel ( www.canada.ca/en/public-health/services/travel-health/about-catmat.html )
- • Centre for Disease Control and Prevention Health Information for International Travel, otherwise known as the CDC Yellow Book ( wwwnc.cdc.gov/travel/page/yellowbook-home )
- • Travel Health Pro ( travelhealthpro.org.uk/ )
- • American College of Gastroenterology (ACG) Clinical Guideline: Diagnosis, Treatment and Prevention of Acute Diarrheal Infections in Adults 4
- ○ Readers should note that information presented in this guideline related to definitions of TD and management options based on the number of loose stools has been redefined in more recent guidelines; however, the document still provides valuable guidance on symptom management.
- • Pharmacy5in5 TD Infographic ( https://uwaterloo.ca/pharmacy/sites/ca.pharmacy/files/uploads/files/tdinfographic.pdf )
- ○ Pharmacy5in5 is a free online learning platform designed by pharmacists for pharmacists and pharmacy technicians. Pharmacists interested in testing their TD knowledge are encouraged to complete the module on TD.
For both nondysenteric and dysenteric TD, azithromycin is the preferred agent because of its low global resistance against invasive pathogens and tolerable safety profile. 38 - 41 A single-dose antibiotic regimen can be tried initially and continued daily for up to 3 days if symptoms are not resolved within 24 hours. Therefore, pharmacists should ensure patients are provided sufficient antibiotics to allow for both a single dose and a complete 3-day regimen. Fluoroquinolones may be used to treat severe, nondysenteric TD, provided the traveler is not going to Southeast or South Asia (due to Campylobacter resistance) and a proper risk-benefit assessment has been completed regarding its safety profile. Rifaximin may also be used to treat severe, nondysenteric TD, provided the traveler is not going to a region that has a high risk of invasive pathogens, due to the drug’s lack of efficacy against them. However, as mentioned, this product is not available in a suitable strength in Canada and would need to be acquired by patients abroad, limiting its applicability to Canadian travelers. As with moderate diarrhea, combination therapy consisting of antibiotics with loperamide improves time to clinical cure compared with antibiotics alone. However, the combination should not be employed when dysentery is present.
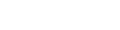
Additional consensus statements of interest to pharmacists
Despite their appeal, prebiotics and probiotics are not currently recommended to prevent or treat TD. More research is needed to determine their use in TD, as questions remain regarding formulation, dosing, strain or combination for the right condition or individual, knowledge of the host microbiome and mechanisms of action. 3 In addition, there is an emerging concern involving the association between travel, the use of antibiotics in TD and the colonization of multidrug-resistant organisms. Carriage is mostly transient but can be persistent 1 year posttravel in approximately 10% of travelers and transmitted to household contacts. 3 Pharmacists should discuss with patients this multidimensional risk regarding travel, TD and the use of antibiotics abroad. Female patients presenting with a urinary tract infection with recent travel should have a urine culture to ensure appropriate antibiotic choice.
Changes to the definitions of illness severity to be largely based on its functional impact on patients (and treatment recommendations based on these symptoms) make it increasingly important for pharmacists to have shared decision-making discussions with patients, considering their individual risk of TD or its complications, their itinerary and goals of their travel and their ability to cope with symptoms abroad. As patients will often need to make symptom assessment and treatment decisions without pharmacist assistance abroad, these discussions at the time of dispensing are especially important to ensure optimal outcomes. ■
Key points for pharmacists related to the prevention and treatment of TD are summarized in Box 1 and the provided infographic, with additional resources that may be of interest provided in Box 2.

Author Contributions: H. Fernandes initiated the article and wrote and reviewed the final draft. S. Houle, A. Johal and M. Riddle wrote and reviewed the final draft.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.

- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
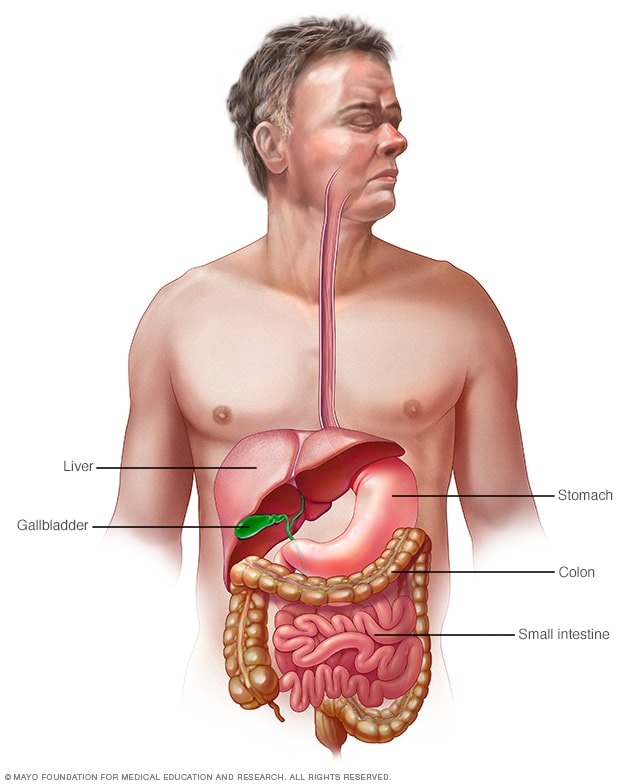
Gastrointestinal tract
Your digestive tract stretches from your mouth to your anus. It includes the organs necessary to digest food, absorb nutrients and process waste.
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant.
When you visit a place where the climate or sanitary practices are different from yours at home, you have an increased risk of developing traveler's diarrhea.
To reduce your risk of traveler's diarrhea, be careful about what you eat and drink while traveling. If you do develop traveler's diarrhea, chances are it will go away without treatment. However, it's a good idea to have doctor-approved medicines with you when you travel to high-risk areas. This way, you'll be prepared in case diarrhea gets severe or won't go away.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
Traveler's diarrhea may begin suddenly during your trip or shortly after you return home. Most people improve within 1 to 2 days without treatment and recover completely within a week. However, you can have multiple episodes of traveler's diarrhea during one trip.
The most common symptoms of traveler's diarrhea are:
- Suddenly passing three or more looser watery stools a day.
- An urgent need to pass stool.
- Stomach cramps.
Sometimes, people experience moderate to severe dehydration, ongoing vomiting, a high fever, bloody stools, or severe pain in the belly or rectum. If you or your child experiences any of these symptoms or if the diarrhea lasts longer than a few days, it's time to see a health care professional.
When to see a doctor
Traveler's diarrhea usually goes away on its own within several days. Symptoms may last longer and be more severe if it's caused by certain bacteria or parasites. In such cases, you may need prescription medicines to help you get better.
If you're an adult, see your doctor if:
- Your diarrhea lasts beyond two days.
- You become dehydrated.
- You have severe stomach or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
While traveling internationally, a local embassy or consulate may be able to help you find a well-regarded medical professional who speaks your language.
Be especially cautious with children because traveler's diarrhea can cause severe dehydration in a short time. Call a doctor if your child is sick and has any of the following symptoms:
- Ongoing vomiting.
- A fever of 102 F (39 C) or more.
- Bloody stools or severe diarrhea.
- Dry mouth or crying without tears.
- Signs of being unusually sleepy, drowsy or unresponsive.
- Decreased volume of urine, including fewer wet diapers in infants.
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become used to the bacteria and have developed immunity to them.
Risk factors
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of:
- Central America.
- South America.
- South Asia and Southeast Asia.
Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses some risk. However, your risk of traveler's diarrhea is generally low in Northern and Western Europe, Japan, Canada, Singapore, Australia, New Zealand, and the United States.
Your chances of getting traveler's diarrhea are mostly determined by your destination. But certain groups of people have a greater risk of developing the condition. These include:
- Young adults. The condition is slightly more common in young adult tourists. Though the reasons why aren't clear, it's possible that young adults lack acquired immunity. They may also be more adventurous than older people in their travels and dietary choices, or they may be less careful about avoiding contaminated foods.
- People with weakened immune systems. A weakened immune system due to an underlying illness or immune-suppressing medicines such as corticosteroids increases risk of infections.
- People with diabetes, inflammatory bowel disease, or severe kidney, liver or heart disease. These conditions can leave you more prone to infection or increase your risk of a more-severe infection.
- People who take acid blockers or antacids. Acid in the stomach tends to destroy organisms, so a reduction in stomach acid may leave more opportunity for bacterial survival.
- People who travel during certain seasons. The risk of traveler's diarrhea varies by season in certain parts of the world. For example, risk is highest in South Asia during the hot months just before the monsoons.
Complications
Because you lose vital fluids, salts and minerals during a bout with traveler's diarrhea, you may become dehydrated, especially during the summer months. Dehydration is especially dangerous for children, older adults and people with weakened immune systems.
Dehydration caused by diarrhea can cause serious complications, including organ damage, shock or coma. Symptoms of dehydration include a very dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness.
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Don't consume unpasteurized milk and dairy products, including ice cream.
- Don't eat raw or undercooked meat, fish and shellfish.
- Don't eat moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Don't drink unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Don't use locally made ice cubes or drink mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You also can chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They also can cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medicine for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medicines, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears, called tinnitus.
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Traveller's diarrhoea
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Traveller's diarrhoea is a common problem among travellers to destinations with deficiencies in water, sanitation, and hygiene (WASH) infrastructure, typically caused by the consumption of contaminated food or water. Predominantly caused by bacteria.
Prevention strategies include careful selection of food and beverages, though these are not fail-safe. Prophylactic antibiotics are not recommended for most travellers.
Management is self-diagnosis while still travelling, followed by hydration, medicine for symptom relief, and possibly, antibiotics. Antibiotic therapy is generally reserved for moderate to severe infections.
In healthy patients, resolution is typically within 3-5 days even without antibiotic treatment.
Traveller's diarrhoea (TD) is defined as ≥3 unformed stools in 24 hours accompanied by at least one of the following: fever, nausea, vomiting, cramps, tenesmus, or bloody stools (dysentery) during a trip abroad, typically to a destination with deficiencies in water, sanitation, and hygiene (WASH) infrastructure. It is usually a benign, self-limited illness lasting 3-5 days.
History and exam
Key diagnostic factors.
- presence of risk factors
- diarrhoea (with or without tenesmus), cramping, nausea, and vomiting
- dysentery (blood and fever)
- persistent diarrhoea >14 days
Other diagnostic factors
- diarrhoea without illness
Risk factors
- travel to a high-risk destination
- age <30 years
- proton-pump inhibitor use
- travellers with prior residence in higher-risk destination visiting friends and relatives
- travel during hot and wet seasons
- deployed military populations
- lack of caution in food and water selection
Diagnostic investigations
1st investigations to order.
- stool culture and sensitivity
- multi-pathogen molecular diagnostic (polymerase chain reaction)
- protozoal stool antigens
Investigations to consider
- stool ova and parasite examination
- Clostridioides difficile stool toxin
- colonoscopy, endoscopy, and biopsy
- haematology, blood chemistries, serology
Treatment algorithm
Pre-travel prophylaxis, non-pregnant adults: mild diarrhoea, non-pregnant adults: moderate diarrhoea, non-pregnant adults: severe diarrhoea, contributors, daniel t. leung, md, msc.
Associate Professor
Division of Infectious Diseases
University of Utah School of Medicine
Salt Lake City
Disclosures
DTL receives authorship royalties from UpToDate, Inc, for a chapter on travel medicine. DTL is an author of upcoming chapters on traveller's diarrhoea for the US CDC Yellow Book. DTL is the president-elect of the American Committee on Clinical Tropical Medicine and Travelers' Health - Clinical Group within the American Society of Tropical Medicine and Hygiene. DTL is an author of some of the references cited in this topic.
Jakrapun Pupaibool, MD, MS
JP declares that he has no competing interests.
Acknowledgements
Dr Daniel T. Leung and Dr Jakrapun Pupaibool would like to gratefully acknowledge Dr Mark Riddle and Professor Gregory Juckett, the previous contributor to this topic.
MR has given talks on the management of traveller's diarrhoea for the International Society of Travel Medicine (ISTM), the CDC Foundation, the American College of Gastroenterology (ACG), and the American College of Preventive Medicine. MR has led the development of guidelines for traveller's diarrhea for the ISTM, the ACG, and the Department of Defense. This work has been unpaid but support for travel has been accepted. MR is employed with Pfizer Inc., and is working on their Lyme disease vaccine programme. While this is not in conflict with traveller’s diarrhoea, Pfizer also makes azithromycin, which is an antibiotic recommended for the treatment of traveller’s diarrhoea. MR does not work in the area of Pfizer that develops, markets, or distributes azithromycin. MR is an author of several references cited in this topic. GJ declares that he has no competing interests.
Peer reviewers
Andrea summer, md.
Assistant Professor of Pediatrics
Medical University of South Carolina
AS declares that she has no competing interests.
Phil Fischer, MD
Professor of Pediatrics
Department of Pediatric and Adolescent Medicine
Mayo Clinic
PF is an author of a reference cited in this topic.
Differentials
- Food poisoning
- Irritable bowel syndrome
- Secondary disaccharidase (or other dietary) deficiency
- CDC Yellow Book 2024: travelers' diarrhea
- 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea
Patient leaflets
Diarrhoea in adults
Use of this content is subject to our disclaimer
Help us improve BMJ Best Practice
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
- Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Traveller's diarrhoea
Peer reviewed by Dr Colin Tidy, MRCGP Last updated by Dr Toni Hazell Last updated 10 Feb 2023
Meets Patient’s editorial guidelines
In this series: Amoebiasis Giardia
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. It is caused by consuming food and water, contaminated by germs (microbes) including bacteria, viruses and parasites. Other symptoms can include high temperature (fever), being sick (vomiting) and tummy (abdominal) pain. In most cases it causes a mild illness and symptoms clear within 3 to 4 days. Specific treatment is not usually needed but it is important to drink plenty of fluids to avoid lack of fluid in the body (dehydration). Always make sure that you get any advice that you need in plenty of time before your journey - some GPs offer travel advice but if yours doesn't then you may need to go to a private travel clinic.
In this article :
What is traveller's diarrhoea, what causes traveller's diarrhoea, are all travellers at risk, what are the symptoms of traveller's diarrhoea, how is traveller's diarrhoea diagnosed, when should i seek medical advice for traveller's diarrhoea, how is traveller's diarrhoea in adults treated, how is traveller's diarrhoea in children treated, side-effects of traveller's diarrhoea, how long does traveller's diarrhoea last, how can i avoid traveller's diarrhoea.
Continue reading below
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. Diarrhoea is defined as: 'loose or watery stools (faeces), usually at least three times in 24 hours.'
Traveller's diarrhoea is caused by eating food, or drinking water, containing certain germs (microbes) or their poisons (toxins). The types of germs which may be the cause include:
Bacteria: these are the most common microbes that cause traveller's diarrhoea. Common types of bacteria involved are:
Escherichia coli
Campylobacter
Viruses: these are the next most common, particularly norovirus and rotavirus.
Parasites: these are less common causes. Giardia, cryptosporidium and Entamoeba histolytica are examples of parasites that may cause traveller's diarrhoea.
Often the exact cause of traveller's diarrhoea is not found and studies have shown that in many people no specific microbe is identified despite testing (for example, of a stool (faeces) specimen).
See the separate leaflets called E. Coli (VTEC O157) , Campylobacter, Salmonella, Cryptosporidium , Amoebiasis (dysentery information), Shigella and Giardia for more specific details on each of the microbes mentioned above.
Note : this leaflet is about traveller's diarrhoea in general and how to help prevent it.
Traveller's diarrhoea most commonly affects people who are travelling from a developed country, such as the UK, to a developing country where sanitation and hygiene measures may not meet the same standards. It can affect as many as 2 to 6 in 10 travellers.
There is a different risk depending on whether you travel to high-risk areas or not:
High-risk areas : South and Southeast Asia, Central America, West and North Africa, South America, East Africa.
Medium-risk areas : Russia, China, Caribbean, South Africa.
Low-risk areas : North America, Western Europe, Australia and New Zealand.
Sometimes outbreaks of diarrhoea can occur in travellers staying in one hotel or, for example, those staying on a cruise ship. People travelling in more remote areas (for example, trekkers and campers) may also have limited access to medical care if they do become unwell.
By definition, diarrhoea is the main symptom. This can be watery and can sometimes contain blood. Other symptoms may include:
Crampy tummy (abdominal) pains.
Feeling sick (nausea).
Being sick (vomiting).
A high temperature (fever).
Symptoms are usually mild in most people and last for 3 to 4 days but they may last longer. Symptoms may be more severe in the very young, the elderly, and those with other health problems. Those whose immune systems are not working as well as normal are particularly likely to be more unwell. For example, people with untreated HIV infection, those on chemotherapy, those on long-term steroid treatment or those who are taking drugs which suppress their immune system, for example after a transplant or to treat an autoimmune condition
Despite the fact that symptoms are usually fairly mild, they can often mean that your travel itinerary is interrupted or may need to be altered.
Traveller's diarrhoea is usually diagnosed by the typical symptoms. As mentioned above, most people have mild symptoms and do not need to seek medical advice. However, in some cases medical advice is needed (see below).
If you do see a doctor, they may suggest that a sample of your stool (faeces) be tested. This will be sent to the laboratory to look for any microbes that may be causing your symptoms. Sometimes blood tests or other tests may be needed if you have more severe symptoms or develop any complications.
As mentioned above, most people with traveller's diarrhoea have relatively mild symptoms and can manage these themselves by resting and making sure that they drink plenty of fluids. However, you should seek medical advice in any of the following cases, or if any other symptoms occur that you are concerned about:
If you have a high temperature (fever).
If you have blood in your stools (faeces).
If it is difficult to get enough fluid because of severe symptoms: frequent or very watery stools or repeatedly being sick (vomiting).
If the diarrhoea lasts for more than 5-7 days.
If you are elderly or have an underlying health problem such as diabetes, inflammatory bowel disease, or kidney disease.
If you have a weakened immune system because of, for example, chemotherapy treatment, long-term steroid treatment, or HIV infection.
If you are pregnant.
If an affected child is under the age of 6 months.
If you develop any of the symptoms listed below that suggest you might have lack of fluid in your body (dehydration). If it is your child who is affected, there is a separate list for children.
Symptoms of dehydration in adults
Dizziness or light-headedness.
Muscle cramps.
Sunken eyes.
Passing less urine.
A dry mouth and tongue.
Becoming irritable.
Symptoms of severe dehydration in adults
Profound loss of energy or enthusiasm (apathy).
A fast heart rate
Producing very little urine.
Coma, which may occur.
Note : severe dehydration is a medical emergency and immediate medical attention is needed.
Symptoms of dehydration in children
Passing little urine.
A dry mouth.
A dry tongue and lips.
Fewer tears when crying.
Being irritable.
Having a lack of energy (being lethargic).
Symptoms of severe dehydration in children
Drowsiness.
Pale or mottled skin.
Cold hands or feet.
Very few wet nappies.
Fast (but often shallow) breathing.
Dehydration is more likely to occur in:
Babies under the age of 1 year (and particularly those under 6 months old). This is because babies don't need to lose much fluid to lose a significant proportion of their total body fluid.
Babies under the age of 1 year who were a low birth weight and who have not caught up with their weight.
A breastfed baby who has stopped being breastfed during their illness.
Any baby or child who does not drink much when they have a gut infection (gastroenteritis).
Any baby or child with severe diarrhoea and vomiting. (For example, if they have passed five or more diarrhoeal stools and/or vomited two or more times in the previous 24 hours.)
In most cases, specific treatment of traveller's diarrhoea is not needed. The most important thing is to make sure that you drink plenty of fluids to avoid lack of fluid in your body (dehydration).
Fluid replacement
As a rough guide, drink at least 200 mls after each watery stool (bout of diarrhoea).
This extra fluid is in addition to what you would normally drink. For example, an adult will normally drink about two litres a day but more in hot countries. The above '200 mls after each watery stool' is in addition to this usual amount that you would drink.
If you are sick (vomit), wait 5-10 minutes and then start drinking again but more slowly. For example, a sip every 2-3 minutes but making sure that your total intake is as described above.
You will need to drink even more if you are dehydrated. A doctor will advise on how much to drink if you are dehydrated.
Note : if you suspect that you are becoming dehydrated, you should seek medical advice.
For most adults, fluids drunk to keep hydrated should mainly be water. However, this needs to be safe drinking water - for example, bottled, or boiled and treated water. It is best not to have drinks that contain a lot of sugar, such as fizzy drinks, as they can sometimes make diarrhoea worse. Alcohol should also be avoided.
Rehydration drinks
Rehydration drinks may also be used. They are made from sachets that you can buy from pharmacies and may be a sensible thing to pack in your first aid kit when you travel. You add the contents of the sachet to water.
Home-made salt/sugar mixtures are used in developing countries if rehydration drinks are not available; however, they have to be made carefully, as too much salt can be dangerous. Rehydration drinks are cheap and readily available in the UK, and are the best treatment. Note that safe drinking water should be used to reconstitute oral rehydration salt sachets.
Antidiarrhoeal medication
Antidiarrhoeal medicines are not usually necessary or wise to take when you have traveller's diarrhoea. However you may want to use them if absolutely necessary - for example, if you will be unable to make regular trips to the toilet due to travelling.You can buy antidiarrhoeal medicines from pharmacies before you travel. The safest and most effective is loperamide.
The adult dose of this is two capsules at first. This is followed by one capsule after each time you pass some diarrhoea up to a maximum of eight capsules in 24 hours. It works by slowing down your gut's activity.
You should not take loperamide for longer than two days. You should also not use antidiarrhoeal medicines if you have a high temperature (fever) or bloody diarrhoea.
Eat as normally as possible
It used to be advised to 'starve' for a while if you had diarrhoea. However, now it is advised to eat small, light meals if you can. Be guided by your appetite. You may not feel like food and most adults can do without food for a few days. Eat as soon as you are able but don't stop drinking. If you do feel like eating, avoid fatty, spicy or heavy food. Plain foods such as bread and rice are good foods to try eating.
Antibiotic medicines
Most people with traveller's diarrhoea do not need treatment with antibiotic medicines. However, sometimes antibiotic treatment is advised. This may be because a specific germ (microbe) has been identified after testing of your stool (faeces) sample.
Fluids to prevent dehydration
You should encourage your child to drink plenty of fluids. The aim is to prevent lack of fluid in the body (dehydration). The fluid lost in their sick (vomit) and/or diarrhoea needs to be replaced. Your child should continue with their normal diet and usual drinks. In addition, they should also be encouraged to drink extra fluids. However, avoid fruit juices or fizzy drinks, as these can make diarrhoea worse.
Babies under 6 months old are at increased risk of dehydration. You should seek medical advice if they develop acute diarrhoea. Breast feeds or bottle feeds should be encouraged as normal. You may find that your baby's demand for feeds increases. You may also be advised to give extra fluids (either water or rehydration drinks) in between feeds.
If you are travelling to a destination at high risk for traveller's diarrhoea, you might want to consider buying oral rehydration sachets for children before you travel. These can provide a perfect balance of water, salts and sugar for them and can be used for fluid replacement. Remember that, as mentioned above, safe water is needed to reconstitute the sachets.
If your child vomits, wait 5-10 minutes and then start giving drinks again but more slowly (for example, a spoonful every 2-3 minutes). Use of a syringe can help in younger children who may not be able to take sips.
Note : if you suspect that your child is dehydrated, or is becoming dehydrated, you should seek medical advice urgently.
Fluids to treat dehydration
If your child is mildly dehydrated, this may be treated by giving them rehydration drinks. A doctor will advise about how much to give. This can depend on the age and the weight of your child. If you are breastfeeding, you should continue with this during this time. It is important that your child be rehydrated before they have any solid food.
Sometimes a child may need to be admitted to hospital for treatment if they are dehydrated. Treatment in hospital usually involves giving rehydration solution via a special tube called a 'nasogastric tube'. This tube passes through your child's nose, down their throat and directly into their stomach. An alternative treatment is with fluids given directly into a vein (intravenous fluids).
Eat as normally as possible once any dehydration has been treated
Correcting any dehydration is the first priority. However, if your child is not dehydrated (most cases), or once any dehydration has been corrected, then encourage your child to have their normal diet. Do not 'starve' a child with infectious diarrhoea. This used to be advised but is now known to be wrong. So:
Breastfed babies should continue to be breastfed if they will take it. This will usually be in addition to extra rehydration drinks (described above).
Bottle-fed babies should be fed with their normal full-strength feeds if they will take it. Again, this will usually be in addition to extra rehydration drinks (described above). Do not water down the formula, or make it up with less water than usual. This can make a baby very ill.
Older children - offer them some food every now and then. However, if he or she does not want to eat, that is fine. Drinks are the most important consideration and food can wait until the appetite returns.
Loperamide is not recommended for children with diarrhoea. There are concerns that it may cause a blockage of the gut (intestinal obstruction) in children with diarrhoea.
Most children with traveller's diarrhoea do not need treatment with antibiotics. However, for the same reasons as discussed for adults above, antibiotic treatment may sometimes be advised in certain cases.
Most people have mild illness and complications of traveller's diarrhoea are rare. However, if complications do occur, they can include the following:
Salt (electrolyte) imbalance and dehydration .
This is the most common complication. It occurs if the salts and water that are lost in your stools (faeces), or when you are sick (vomit), are not replaced by you drinking adequate fluids. If you can manage to drink plenty of fluids then dehydration is unlikely to occur, or is only likely to be mild and will soon recover as you drink.
Severe dehydration can lead to a drop in your blood pressure. This can cause reduced blood flow to your vital organs. If dehydration is not treated, your kidneys may be damaged . Some people who become severely dehydrated need a 'drip' of fluid directly into a vein. This requires admission to hospital. People who are elderly or pregnant are more at risk of dehydration.
Reactive complications
Rarely, other parts of your body can 'react' to an infection that occurs in your gut. This can cause symptoms such as joint inflammation (arthritis), skin inflammation and eye inflammation (either conjunctivitis or uveitis). Reactive complications are uncommon if you have a virus causing traveller's diarrhoea.
Spread of infection
The infection can spread to other parts of your body such as your bones, joints, or the meninges that surround your brain and spinal cord. This is rare. If it does occur, it is more likely if diarrhoea is caused by salmonella infection.
Irritable bowel syndrome is sometimes triggered by a bout of traveller's diarrhoea.
Lactose intolerance
Lactose intolerance can sometimes occur for a period of time after traveller's diarrhoea. It is known as 'secondary' or 'acquired' lactose intolerance. Your gut (intestinal) lining can be damaged by the episode of diarrhoea. This leads to lack of a substance (enzyme) called lactase that is needed to help your body digest the milk sugar lactose.
Lactose intolerance leads to bloating, tummy (abdominal) pain, wind and watery stools after drinking milk. The condition gets better when the infection is over and the intestinal lining heals. It is more common in children.
Haemolytic uraemic syndrome
Usually associated with traveller's diarrhoea caused by a certain type of E. coli infection, haemolytic uraemic syndrome is a serious condition where there is anaemia, a low platelet count in the blood and kidney damage. It is more common in children. If recognised and treated, most people recover well.
Guillain-Barré syndrome
This condition may rarely be triggered by campylobacter infection, one of the causes of traveller's diarrhoea. It affects the nerves throughout your body and limbs, causing weakness and sensory problems. See the separate leaflet called Guillain-Barré syndrome for more details.
Reduced effectiveness of some medicines
During an episode of traveller's diarrhoea, certain medicines that you may be taking for other conditions or reasons may not be as effective. This is because the diarrhoea and/or being sick (vomiting) mean that reduced amounts of the medicines are taken up (absorbed) into your body.
Examples of such medicines are those for epilepsy, diabetes and contraception . Speak with your doctor or practice nurse before you travel if you are unsure of what to do if you are taking other medicines and develop diarrhoea.
As mentioned above, symptoms are usually short-lived and the illness is usually mild with most people making a full recovery within in few days. However, a few people with traveller's diarrhoea develop persistent (chronic) diarrhoea that can last for one month or more. It is also possible to have a second 'bout' of traveller's diarrhoea during the same trip. Having it once does not seem to protect you against future infection.
Avoid uncooked meat, shellfish or eggs. Avoid peeled fruit and vegetables (including salads).
Be careful about what you drink. Don't drink tap water, even as ice cubes.
Wash your hands regularly, especially before preparing food or eating.
Be careful where you swim. Contaminated water can cause traveller's diarrhoea.
Regular hand washing
You should ensure that you always wash your hands and dry them thoroughly; teach children to wash and dry theirs:
After going to the toilet (and after changing nappies or helping an older child to go to the toilet).
Before preparing or touching food or drinks.
Before eating.
Some antibacterial hand gel may be a good thing to take with you when you travel in case soap and hot water are not available.
Be careful about what you eat and drink
When travelling to areas with poor sanitation, you should avoid food or drinking water that may contain germs (microbes) or their poisons (toxins). Avoid:
Fruit juices sold by street vendors.
Ice cream (unless it has been made from safe water).
Shellfish (for example, mussels, oysters, clams) and uncooked seafood.
Raw or undercooked meat.
Fruit that has already been peeled or has a damaged skin.
Food that contains raw or uncooked eggs, such as mayonnaise or sauces.
Unpasteurised milk.
Drinking bottled water and fizzy drinks that are in sealed bottles or cans, tea, coffee and alcohol is thought to be safe. However, avoid ice cubes and non-bottled water in alcoholic drinks. Food should be cooked through thoroughly and be piping hot when served.
You should also be careful when eating food from markets, street vendors or buffets if you are uncertain about whether it has been kept hot or kept refrigerated. Fresh bread is usually safe, as is canned food or food in sealed packs.
Be careful where you swim
Swimming in contaminated water can also lead to traveller's diarrhoea. Try to avoid swallowing any water as you swim; teach children to do the same.
Obtain travel health advice before you travel
Always make sure that you visit your GP surgery or private travel clinic for health advice in plenty of time before your journey. Alternatively, the Fit for Travel website (see under Further Reading and References, below) provides travel health information for the public and gives specific information for different countries and high-risk destinations. This includes information about any vaccinations required, advice about food, water and personal hygiene precautions, etc.
There are no vaccines that prevent traveller's diarrhoea as a whole. However, there are some other vaccines that you may need for your travel, such as hepatitis A, typhoid, etc. You may also need to take malaria tablets depending on where you are travelling.
Antibiotics
Taking antibiotic medicines to prevent traveller's diarrhoea (antibiotic prophylaxis) is not generally recommended. This is because for most people, traveller's diarrhoea is mild and self-limiting. Also, antibiotics do not protect against nonbacterial causes of traveller's diarrhoea, such as viruses and parasites. Antibiotics may have side-effects and their unnecessary use may lead to problems with resistance to medicines.
Probiotics have some effect on traveller's diarrhoea and can shorten an attack by about one day. It is not known yet which type of probiotic or which dose, so there are no recommendations about using probiotics to prevent traveller's diarrhoea.
Further reading and references
- Bourgeois AL, Wierzba TF, Walker RI ; Status of vaccine research and development for enterotoxigenic Escherichia coli. Vaccine. 2016 Mar 15. pii: S0264-410X(16)00287-5. doi: 10.1016/j.vaccine.2016.02.076.
- Travellers' diarrhoea ; Fitfortravel
- Riddle MS, Connor BA, Beeching NJ, et al ; Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. J Travel Med. 2017 Apr 1;24(suppl_1):S57-S74. doi: 10.1093/jtm/tax026.
- Giddings SL, Stevens AM, Leung DT ; Traveler's Diarrhea. Med Clin North Am. 2016 Mar;100(2):317-30. doi: 10.1016/j.mcna.2015.08.017.
- Diarrhoea - prevention and advice for travellers ; NICE CKS, February 2019 (UK access only)
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Feb 2028
10 feb 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
Issues by year
Advertising
Volume 44, Issue 1, January-February 2015
Advising travellers about management of travellers’ diarrhoea
How is td defined.
Classic, severe TD is usually defined as at least three unformed bowel movements occurring within a 24-hour period, often accompanied by cramps, nausea, vomiting, fever and/or blood in the stools. 5–7 Moderate TD is defined as one or two unformed bowel movements and other symptoms occurring every 24 hours or as three or more unformed bowel movements without additional symptoms. Mild TD is defined as one or two unformed bowel movements without any additional symptoms and without interference with daily activities. 8,9 TD generally resolves spontaneously, usually after 3–4 days, 8 but, in the interim, frequently leads to disruption of planned activities.
What are the causes of TD?
Approximately 50–80% of TD is caused by bacterial infections; enterotoxigenic Escherichia coli (ETEC) is the most common cause overall. Other bacterial causes include enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAEC), Shigella , Campylobacter and Salmonella species. The exact breakdown of organisms varies according to destination, season and other factors. Noroviruses cause 10–20% of TD cases. Protozoal parasites should be considered particularly in those with persistent diarrhoea (illness lasting ≥14 days) or when antibacterial therapy fails to shorten illness. 10
How can TD be prevented?
Methods for preventing TD include avoidance, immunisation, non-antibiotic interventions or antibiotic prophylaxis. 11
What avoidance measures are generally recommended and do they work?
Avoidance of TD has traditionally relied on recommendations regarding careful food and drink choices (avoiding untreated/unboiled tap water, including ice and water used for brushing teeth, and raw foods such as salads, uncooked vegetables or fruits that cannot be peeled). This underpins the saying ‘Boil it, cook it, peel it or forget it…. easy to remember, impossible to do’. Additional standard advice is that undercooked or raw meat, fish and shellfish are high-risk foods. However, whether deliberately or inadvertently, most people find it very difficult to adhere to dietary restrictions 12 and over 95% of people disobey the rules of ‘safe’ eating and drinking within a few days of leaving home. Additionally, there is minimal evidence for a correlation between adherence to dietary precautions and a reduced risk of TD, 13 although common sense nevertheless supports care with food selection. 4
Where people eat may be more important than what people eat. Risks are associated, in descending order, with street vendors, restaurants and private homes. Use of antibacterial handwash before eating is also recommended. 14
Which vaccines can be considered?
Immunisation has little practical role in the prevention of TD and the only potentially relevant vaccines are those against rotavirus (infants only) and the oral cholera vaccine.
The cholera vaccine has >90% efficacy for prevention of Vibrio cholera but travellers are rarely at risk of infection with this pathogen. 1 The vaccine contains a recombinant B subunit of the cholera toxin that is antigenically similar to the heat-labile toxin of ETEC; therefore, the cholera vaccine may also reduce ETEC TD. However, it is not licensed for TD prevention in Australia and, although initially thought to offer a 15–20% short-term (3 months) reduction in TD, a recent Cochrane review showed no statistically significant effects on ETEC diarrhoea or all-cause diarrhoea. 15 Overall, there is, therefore, insufficient evidence to support general use of the cholera vaccine for TD protection, but it may still be considered for individuals with increased risk of severe or complicated TD (eg immunosuppressed or underlying inflammatory bowel disease).
Other vaccines directed against organisms spread by the faecal–oral route are the vaccines for typhoid, hepatitis A and polio, but infection with these organisms rarely causes TD. 15
Do non-antibiotic interventions work?
Several probiotic agents have been studied for treatment and prevention of TD, including Lactobacillus and Saccharomyces preparations. However, their effectiveness for TD prevention has been limited, 11,16,17 and a consensus group has recommended against their use. 4 Other over-the-counter agents are also available (eg travelan, which contains bovine colostrum harvested from cows immunised with an ETEC vaccine) but data regarding overall efficacy of reducing all-cause TD are currently lacking.
Should antibiotic prophylaxis against TD be given?
Quinolone antibiotics are highly effective (80–95%) in preventing TD, but antibiotic prophylaxis is rarely indicated. 4 It may result in a false sense of security and hence less caution in dietary choices, it poses risks of side effects, diarrhoea associated with Clostridium difficile , and, more importantly, would lead to a vast amount of antibiotic use, thus predisposing to more rapid development of antibiotic resistance globally. 11 Therefore non-antibiotic options for prevention and a focus instead on empirical self-treatment if needed according to symptoms are the mainstay of management, aligning with the antimicrobial stewardship perspective of minimisation of antimicrobial overuse and reducing promotion of antimicrobial resistance.
In rare circumstances, it may be reasonable to consider short courses of antibiotic prophylaxis in individuals at very high risk of infection (eg severely immunocompromised). 11 Globally, one of the most commonly used agents in this regard is rifaximin, a non-absorbed semisynthetic rifamycin derivative, which has been shown to be effective and is approved for use for TD prevention in some countries, but it is not approved for this indication in Australia. Other options include the antibiotics discussed below for TD self-treatment.
How should self-treatment of TD be managed?
Because of the limitations of TD prevention measures, the pre-travel consultation should be viewed as an opportunity to ‘arm’ travellers with the knowledge and medication needed to appropriately self-treat, should TD occur during their trip.
The first goal of therapy is the prevention and treatment of dehydration, which is of particular concern for young children, pregnant women and the elderly. Commercial packets of oral rehydration salts are readily available in pharmacies and should be purchased before travel. The other element of TD self-treatment is to recommend travellers bring an antimotility agent plus an antibiotic with them. Loperamide is preferred over the diphenoxylate/atropine combination, as the latter agent is generally less effective and associated with a greater potential for adverse effects.
When should loperamide alone versus loperamide plus an antibiotic be taken?
For mild symptoms of watery diarrhoea, self-treatment with oral rehydration plus loperamide is recommended. Loperamide therapy alone has no untoward effects in mild TD 18 but if symptoms worsen, or do not improve after 24 hours, antibiotics should be added. If TD is moderate or severe at onset, then combination therapy with loperamide plus antibiotics should be started immediately, as this optimises the clinical benefit of self-treatment by providing more rapid relief and shortening the symptom duration. 10,19
The recommended dose of loperamide is two tablets (4 mg) stat, then one tablet after each bowel motion to a maximum of eight per 24-hour period until the TD has resolved. Despite warnings regarding the safety of antidiarrhoeal agents with bloody diarrhoea or diarrhoea accompanied by fever, the combination with antibiotics is likely to be safe in the setting of mild febrile dysentery, 18 and a number of studies have shown the combination to be more efficacious than use of either agent alone. 7,18–20 Rapid institution of effective treatment shortens symptoms to 30 hours or less in most people. 12 For example, the duration of diarrhoea was significantly ( P = 0.0002) shorter following treatment with azithromycin plus loperamide (11 h) than with azithromycin alone (34 h). 19
Which antibiotic should be recommended for empirical elf-treatment of TD?
The most commonly used antibiotics for empirical TD therapy are fluoroquinolones (either norfloxacin or ciprofloxacin) or azithromycin ( Table 1 ). Cotrimoxazole has been used but is no longer recommended because of widespread resistance. For TD caused by ETEC, the fluoroquinolones and azithromycin have similar efficacy; however, in Asia (particularly South and South-East Asia), Campylobacter is a common cause of TD and strains occurring in this part of the world show a high degree of resistance to fluoroquinolones. 10,21 Therefore, azithromycin is preferred for travellers to this region. Azithromycin remains generally efficacious despite emerging resistance, and is also the preferred treatment for diarrhoea with complications of dysentery or high fever, and for use in pregnant women or children under the age of 8 years, in whom avoidance of quinolones is preferred. Moreover, the 24-hour dosing of azithromycin may be preferable to the 12-hourly dosing schedule required with fluoroquinolones.
What is the optimal dosing schedule?
The fluoroquinolones and azithromycin have been administered as a single dose or for 3 days ( Table 1 ). Usually a single dose is adequate and there is no apparent clinically important difference in efficacy with either dosing schedule for TD. 10 However, for bacteria such as Campylobacter and Shigella dysenteriae , single-dose therapy may be inadequate. 11 It is reasonable, therefore, to give travellers a 3-day supply of antibiotics and tell them to continue taking the therapy (either 12- or 24-hourly, depending on which antibiotic is prescribed) only if their TD symptoms persist. If the TD has resolved, no further antibiotics need to be taken and any remaining antibiotic doses can be kept in case of a second bout of TD. It is prudent to specifically highlight that this advice differs from the usual instructions to take all tablets even if symptoms have resolved.
What is the optimal empirical TD management in children?
There are few data on empirical treatment of TD in children and limited options for therapy. The mainstay of therapy is oral rehydration solution, particularly for children <6 years of age. Antimotility agents are contraindicated for children because of the increased risk of adverse effects, especially paralytic ileus, toxic megacolon and drowsiness (narcotic effect) with loperamide. 1 The lower age limit recommended for avoiding loperamide varies by location; US guidelines state that loperamide should not be given to infants <2 years of age, the UK <4 years and Australian guidelines state <12 years. 14 However, most Australian practitioners are prepared to use loperamide in children aged 6 years or older, if needed to control symptoms.
A paediatric (powder) formulation of azithromycin is available and is the most commonly recommended agent for children. The usual dose is 10–25 mg/kg for up to 3 days. A practical tip is to ensure that the pharmacy does not reconstitute the powder into a solution, as once dissolved, the solution lasts only for 10 days. Instead, sterile water should be provided along with instructions on how to reconstitute the powder if needed. Fluoroquinolones (ciprofloxacin or norfloxacin 10mg/kg bd) are an alternative option if there are reasons for avoiding azithromycin, with previous concerns regarding potential effects on cartilage not substantiated in recent studies. 14,22
Does starting antibiotics early prevent the chances of developing prolonged symptoms?
Although TD symptoms are short-lived in most cases, 8–15% of affected travellers are symptomatic for more than a week and 2% develop chronic diarrhoea lasting a month or more. 11 Episodes of TD have been shown to be associated with a quintuple risk of developing irritable bowel syndrome (IBS), and post-travel IBS occurs in 3–10% of travellers. However, it is unknown whether IBS can be prevented by starting antimicrobial therapy earlier in the course of enteric infection. 4,18,23
Should tinidazole also be prescribed and, if so, for whom?
Tinidazole can be prescribed as a second antibiotic for empirical self‑treatment as it is effective against the protozoan parasitic enteric pathogen Giardia intestinalis . A dose of 2 g (4 x 500 mg tablets) stat is recommended. However, for most short-term travellers, tinidazole may be unnecessary and the complexity of the additional instructions required may be unwarranted. It is optimally recommended, therefore, for travellers departing on trips of significant duration (>2–3 weeks). If prescribed, the instructions should be to take tinidazole if the TD persists following the 3-day course of antibiotic therapy (fluoroquinolone or azithromycin). This will mean that the TD has lasted for at least 72 hours, thus increasing the likelihood of a parasitic cause.
When should medical care for acute symptoms be recommended?
While most episodes of TD are amenable to self-treatment, if there is a risk of dehydration due to intolerance of oral fluids or comorbidities, as well as in the setting of frank blood in the stool or unremitting fevers (>38.5°C for 48 hours), medical therapy should be sought. 18
How should TD be managed after return?
While a full description of TD management is beyond the scope of this article, for returning travellers with diarrhoea, at least one (preferably three) stool sample(s) should be taken, including specific requests for evaluation of parasites. For patients who are unwell, particularly those with fevers or dysentery, initiation of empirical antibiotic treatment with azithromycin or a quinolone may be needed while awaiting results. For those with prolonged symptoms, tinidazole as empirical therapy for protozoan parasites may be considered. Endoscopic evaluation may also be advisable if no infectious cause is found and symptoms do not resolve.
- Travellers’ diarrhoea continues to affect 20–50% of people undertaking trips to areas with under-developed sanitation and there is minimal evidence for beneficial effects of dietary precautions.
- Evidence for the benefit of cholera vaccine in reducing TD is limited, but it can be considered in people at high risk of infection.
- In 50–80% of TD cases, TD is caused by bacterial infection. Mild diarrhoea can be managed with an antimotility agent (loperamide) alone, but for moderate or severe diarrhoea, early self-treatment with loperamide in conjunction with antibiotics is advised.
- Recommended empirical antibiotics are fluoroquinolones (norfloxacin / ciprofloxacin) or azithromycin for up to 3 days, although in the setting of increasing resistance, the latter is preferred for travellers to South and South-East Asia.
Competing interests: Karin Leader received a consultancy fee from Imuron in relation to the C. difficile vaccine. She is also an ISTM board member and received a consultancy from ISTM to join the GeoSentinel leadership team. She received grants from Sanofi to develop a mobile phone app for splenectomised patients and from GSK to research the use of the HBV vaccine. GSK also paid her to lecture on travel risks at the Asia Pacific Travel Health Conference. She has received support from both GSK and Sanofi to attend travel medicine conferences.
Provenance and peer review: Commissioned, externally peer reviewed
- Diemert DJ. Prevention and self-treatment of travelers’ diarrhea. Prim Care 2002;29:843–55. Search PubMed
- Department of Health and Human Services. Centers for Disease Control and Prevention. Travelers’ Diarrhea. Available at www.cdc.gov/ncidod/dbmd/diseaseinfo/travelersdiarrhea_g.htm [Accessed 25 November 2014]. Search PubMed
- Paredes-Paredes M, Flores-Figueroa J, Dupont HL. Advances in the treatment of travelers’ diarrhea. Curr Gastroenterol Rep 2011;13:402–07. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for prevention of travelers’ diarrhea. J Travel Med 2009;16:149–60. Search PubMed
- Nair D. Travelers’ diarrhea: prevention, treatment, and post-trip evaluation. J Fam Pract 2013;62:356–61. Search PubMed
- De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. The Cochrane Database Syst Rev 2000:CD002242. Search PubMed
- Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler’s diarrhea: a systematic review and meta-analysis. Clin Infect Dis 2008;47:1007–14. Search PubMed
- Steffen R. Epidemiology of traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S536–40. Search PubMed
- Steffen R, Collard F, Tornieporth N, et al. Epidemiology, etiology, and impact of traveler’s diarrhea in Jamaica. JAMA 1999;281:811–17. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med 2009;16:161–71. Search PubMed
- Diemert DJ. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006;19:583–94. Search PubMed
- Travelers’ diarrhea. NIH Consensus Development Conference. JAMA 1985;253:2700–04. Search PubMed
- Shlim DR. Looking for evidence that personal hygiene precautions prevent traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S531–35. Search PubMed
- Plourde PJ. Travellers’ diarrhea in children. Paediatr Child Health 2003;8:99–103. Search PubMed
- Ahmed T, Bhuiyan TR, Zaman K, Sinclair D, Qadri F. Vaccines for preventing enterotoxigenic Escherichia coli (ETEC) diarrhoea. Cochrane Database Syst Rev 2013;7:CD009029. Search PubMed
- Ritchie ML, Romanuk TN. A meta-analysis of probiotic efficacy for gastrointestinal diseases. PloS One 2012;7:e34938. Search PubMed
- Centers for Disease Control Prevention. Yellow Book. Chapter 2. Travelers’ Diarrhea. Available at wwwnc.cdc.gov/travel/yellowbook/2014/chapter-2-the-pre-travel-consultation/travelers-diarrhea [Accessed 25 November 2014]. Search PubMed
- Wingate D, Phillips SF, Lewis SJ, et al. Guidelines for adults on self-medication for the treatment of acute diarrhoea. Aliment Pharmacol Ther 2001;15:773–82. Search PubMed
- Ericsson CD, DuPont HL, Okhuysen PC, Jiang ZD, DuPont MW. Loperamide plus azithromycin more effectively treats travelers’ diarrhea in Mexico than azithromycin alone. J Travel Med 2007;14:312–19. Search PubMed
- Murphy GS, Bodhidatta L, Echeverria P, et al. Ciprofloxacin and loperamide in the treatment of bacillary dysentery. Ann Intern Med 1993;118:582–86. Search PubMed
- Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis 2007;44:338–46. Search PubMed
- Yung A, Leder K, Torresi J, et al. Manual of Travel Medicine. 3rd edn. Melbourne: IP Communciations, 2011. Search PubMed
- Stermer E, Lubezky A, Potasman I, Paster E, Lavy A. Is traveler’s diarrhea a significant risk factor for the development of irritable bowel syndrome? A prospective study. Clin Infect Dis 2006;43:898–901. Search PubMed
- Expert Group for Antibiotic. Antiobiotic: gastrointestinal tract infections: acute gastroenteritis: acute diarrhoea in special groups: travellers’ diarrhoea. In: eTG Complete [Internet] Melbourne. Therapeutic Guidelines Ltd, 2014. Search PubMed
Also in this issue: Environmental
Professional
Printed from Australian Family Physician - https://www.racgp.org.au/afp/2015/january-february/advising-travellers-about-management-of-travellers © The Australian College of General Practitioners www.racgp.org.au
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
After Travel Tips

You may get infected during travel but not have symptoms until you get home. If you recently traveled and feel sick, particularly if you have a fever, talk to your healthcare provider, and tell them about your travel.
Contact your healthcare provider if you feel sick
Contact your healthcare provider if you feel sick after your trip. Sharing the following information may help your healthcare provider identify possible diseases or infections:
- Your vaccination history.
- Where you traveled.
- Your reasons for traveling.
- Your travel activities, including swimming, hiking, etc.
- The timeframe of your vacation.
- Where you stayed, such as hotels, family or friends’ homes, hostels, or tents.
- What you ate and drank.
- Animals you had close contact with or touched.
- If you have any injuries, scratches, or bug bites.
- Health care or medications you received during your trip.
- Close contact with other people, including sexual encounters.
- If you got any tattoos or piercings.
If your healthcare provider has trouble determining why you are feeling sick, you may want to ask to speak with an infectious disease doctor or travel medicine specialist. Find a clinic for a travel medicine specialist.
Long-term Travelers
Long-term travelers, such as expatriate workers, Peace Corps volunteers, or missionaries, have a greater risk of getting infected, sometimes without symptoms, during travel. If you are a long-term traveler, consider having a thorough medical exam or interview with your healthcare provider after you return to the United States.
More Information:
- The Post Travel Evaluation in CDC Yellow Book
- Long-Term Travelers & Expatriates in CDC Yellow Book
- Screening Asymptomatic Returned Travelers in CDC Yellow Book
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Search the site GO Please fill out this field.
- Newsletters
- Digestive Health
What Causes Loose Stool?
:max_bytes(150000):strip_icc():format(webp)/7cZXd_5cLI7mNtZRS31XzPzGTeA8lh_k24WTXKJk-mo-3956d73663764f15bce8e3e4ea4d59fa.jpeg)
- Identification
- When To Seek Care
Loose stools—sometimes called diarrhea—are loose, watery bowel movements that occur frequently. Some of the most common causes of loose stools are infections, medication side effects, and travelers' diarrhea. Chronic conditions like Crohn’s disease, ulcerative colitis UC), irritable bowel syndrome (IBS), and celiac disease also cause loose stools.
Loose stools can be either acute or chronic, depending on the cause. Acute loose stools last two weeks or less, while loose stools that last 2-4 weeks are considered persistent diarrhea. Chronic diarrhea lasts four weeks or more.
Between 1-5% of adults have chronic diarrhea. Depending on the cause of your diarrhea, there are several ways to manage and treat symptoms. You can also take steps to prevent loose stools from occurring.
Design by Health
What Does Loose Stool Look Like?
Healthcare providers often use a chart known as the Bristol Stool Form Scale (BSFS) to evaluate stool consistency. This scale identifies seven types of bowel movements and contains three points that indicate loose stool.
These loose stool points are types 5-7. Type 5 contains soft blobs with clear-cut edges and is often passed easily due to its loose consistency. Type 6 contains fluffy pieces with ragged edges and is a mushy consistency. Type 7 is extremely loose or watery with no solid edges.
According to the Bristol Stool Scale, loose stool is considered diarrhea. When this occurs, you may also feel an urgent need to use the bathroom , cramping, stomach pain, and nausea. In more extreme cases, you may feel lightheaded and dizzy as well as have a fever and vomit.
Causes of Loose Stool
Having loose stool or experiencing diarrhea is a common symptom of many different conditions. Here are some of the more common causes of loose stool.
Three types of infections can cause loose stools: viral, bacterial, and parasitic. The norovirus and rotavirus are the two most common viruses responsible for loose stools, but viral gastroenteritis can also cause diarrhea.
Bacteria can enter your body through contaminated food and water resulting in a bacterial infection that causes loose stools. The bacteria most often responsible for these loose stools include E. coli, salmonella, campylobacter , and shigella.
Similarly, parasites can enter the body through contaminated food and water causing parasitic infections that lead to diarrhea. Parasites that most often affect people include cryptosporidium enteritis, entamoeba histolytica , and giardia lamblia.
Medication Side Effects
Several medications can cause you to pass loose stool—antibiotics being the most common. Some cancer medications and antacids can also lead to diarrhea.
Before starting a new medication, talk to a healthcare provider about its side effects. If loose stool is a possibility, ask your provider for ways to prevent this side effect. Also, remember that long-term use of certain medications or powerful antibiotics can cause gut changes, leading to chronic diarrhea known as Clostridioides difficile ( C. diff ) .
Travelers' Diarrhea
Traveling to developing countries can often lead to loose stools, especially if you eat contaminated food or drink water that contains bacteria or parasites. Viruses can also spread through food and water in some countries.
Typically, the diarrhea you get from traveling is acute, meaning it will not last more than two weeks. However, some parasites can take longer to get rid of.
Food Sensitivities and Allergies
People who have food sensitivities like lactose intolerance or gluten sensitivity may experience loose stools after consuming foods with lactose or gluten. Also, if you are allergic to certain foods, you can have loose stools if you consume those foods.
It's possible to have a fructose intolerance and an intolerance to sugar alcohols like sorbitol, mannitol, and xylitol—commonly found in many processed foods and drinks. If you have an allergy or intolerance, your healthcare provider may advise limiting or even eliminating the foods you are sensitive to for a short period to see if it helps reduce the number of loose stools you have.

Digestive Disorders and Conditions
Certain disorders or digestive conditions can be the underlying cause of loose stools. Common conditions that can cause chronic diarrhea include celiac disease , Crohn's disease, irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), and ulcerative colitis (UC).
Your healthcare provider may run several tests to determine if one of these conditions is the root cause of your chronic diarrhea.
When To See a Healthcare Provider
Although loose stool is not necessarily harmful, it can become problematic if it is ongoing and has the potential to lead to dehydration or malabsorption. Loose stool can signal an underlying medical condition that needs to be addressed. You should consider seeing a healthcare provider for loose stool if you are:
- Passing loose stools for more than two days (for adults) or more than 24 hours (for children)
- Showing signs of dehydration like dry mouth, excessive thirst, and dark urine
- Experiencing severe pain in your stomach or rectum
- Passing six or more loose stools in 24 hours
- Having a fever of 102 degrees Fahrenheit or higher
- Passing stools that contain blood or pus
- Having black or tar-like stools
Treatments for Loose Stool
Treatments for loose stools often depend on the underlying cause. The treatment options may include over-the-counter (OTC) medications, prescription drugs, diet changes, and supplements.
Medications
Acute loose stools can typically be treated with OTC medications. A healthcare provider may suggest Imodium (loperamide) or Pepto-Bismol (bismuth subsalicylate).
If you have a bacterial or parasitic infection, your provider can prescribe antibiotics or other medications to help clear up the infection.
If your loose stools are caused by an underlying condition like UC, Crohn's disease , or IBS, your provider may prescribe certain medications as part of a treatment plan.
Dietary Changes
When a food allergy or food sensitivity is the cause of loose stools, your provider will likely advise limiting or removing the food from your diet for a short period to see if it relieves the symptom.
Changing your dietary pattern can also help you treat loose stools even if you have no sensitivities. To help combat diarrhea, healthcare providers often recommend the BRAT diet (bananas, rice, applesauce, and toast).
You should also drink plenty of fluids to prevent dehydration. Beverages with added electrolytes can help replenish the electrolytes you've lost from passing loose stools.
Supplements
Healthcare providers might recommend supplements for treating loose stools. Researchers are investigating the role that probiotics can play in the treatment of diarrhea. However, the effects and benefits of probiotics are still not fully understood. If you're interested in taking probiotics for diarrhea, talk to your healthcare provider about how much to take and for how long.
Research has also shown that taking zinc supplements for about 10-14 days can help reduce the duration of loose stools and decrease the likelihood of developing persistent diarrhea.
Other supplements that show promise for treating chronic diarrhea include:
- Phosphatidylcholine
- Lactoferrin
- Palmitoylethanolamide (PEA)
In cases of chronic diarrhea, your provider may suggest taking supplemental vitamins and minerals to fill any nutritional gaps you may have due to the malabsorption that loose stools can cause. Taking fiber supplements can also help add bulk to your stool.
Certain types of diarrhea or loose stools are preventable—like traveler's diarrhea and rotavirus. However, you likely cannot completely avoid loose stool. Here are some tips for preventing or reducing your risk of diarrhea :
- Wash your hands thoroughly with warm water and soap for 15-30 seconds after using the restroom or changing diapers, or when handling food
- Make sure to clean, store, and prepare foods properly
- Avoid tap water, unpasteurized milk or juice, raw fruits and vegetables, food from street vendors, and raw or undercooked meat, fish, or shellfish when traveling
- Use bottled or purified water for brushing your teeth, drinking, and making ice cubes when traveling
- Get your infant vaccinated against the rotavirus, ensuring they receive all the doses by the time they are 8 months old
A Quick Review
Loose stools, or diarrhea, are loose, watery bowel movements caused by viruses, food sensitivities, parasites, infections, medications, some digestive disorders, and more. They can be acute or chronic depending on the underlying cause.
You can treat diarrhea with medications, dietary changes, and possibly probiotics. See a healthcare provider if you have diarrhea for more than two days or pass more than six loose stools in a 24-hour period.
MedlinePlus. Diarrhea .
National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms and causes of diarrhea .
American College of Gastroenterology. Diarrheal diseases overview .
American Family Physician. Chronic diarrhea in adults: Evaluation and differential diagnosis .
Chumpitazi BP, Self MM, Czyzewski DI, Cejka S, Swank PR, Shulman RJ. Bristol Stool Form Scale reliability and agreement decreases when determining Rome III stool form designations . Neurogastroenterol Motil . 2016;28(3):443-448. doi:10.1111/nmo.12738
National Institute of Diabetes and Digestive and Kidney Diseases. Treatment for diarrhea .
Kanikowska A, Janisz S, Mańkowska-Wierzbicka D, Gabryel M, Dobrowolska A, Eder P. Management of adult patients with gastrointestinal symptoms from food hypersensitivity: Narrative Review . J Clin Med . 2022;11(24):7326. doi:10.3390/jcm11247326
Nemeth V, Pfleghaar N. Diarrhea . In: StatPearls . StatPearls Publishing; 2024.
Barffour MA, Hinnouho GM, Wessells KR, et al. Effects of therapeutic zinc supplementation for diarrhea and two preventive zinc supplementation regimens on the incidence and duration of diarrhea and acute respiratory tract infections in rural Laotian children: A randomized controlled trial . J Glob Health . 2020;10(1):010424. doi:10.7189/jogh.10.010424
Kiani AK, Bonetti G, Donato K, Bertelli M. Dietary supplements for intestinal inflammation . J Prev Med Hyg . 2022;63(2 Suppl 3):E214-E220. doi:10.15167/2421-4248/jpmh2022.63.2S3.2763
MedlinePlus. Fiber .
Related Articles
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Urinary Catheter Culture Stewardship
- Clinical Safety
- Antibiotic Prescribing and Use
- Healthcare-Associated Infections (HAIs)
Urinary Tract Infection Basics
- Do you have pain or burning when you urinate? You might have a urinary tract infection (UTI).
- Antibiotics treat UTIs. Your healthcare provider can determine if you have a UTI and what antibiotic you need.
The urinary tract includes the bladder, urethra and kidneys (see figure). UTIs are common infections that happen when bacteria, often from the skin or rectum, enter the urethra and infect the urinary tract.
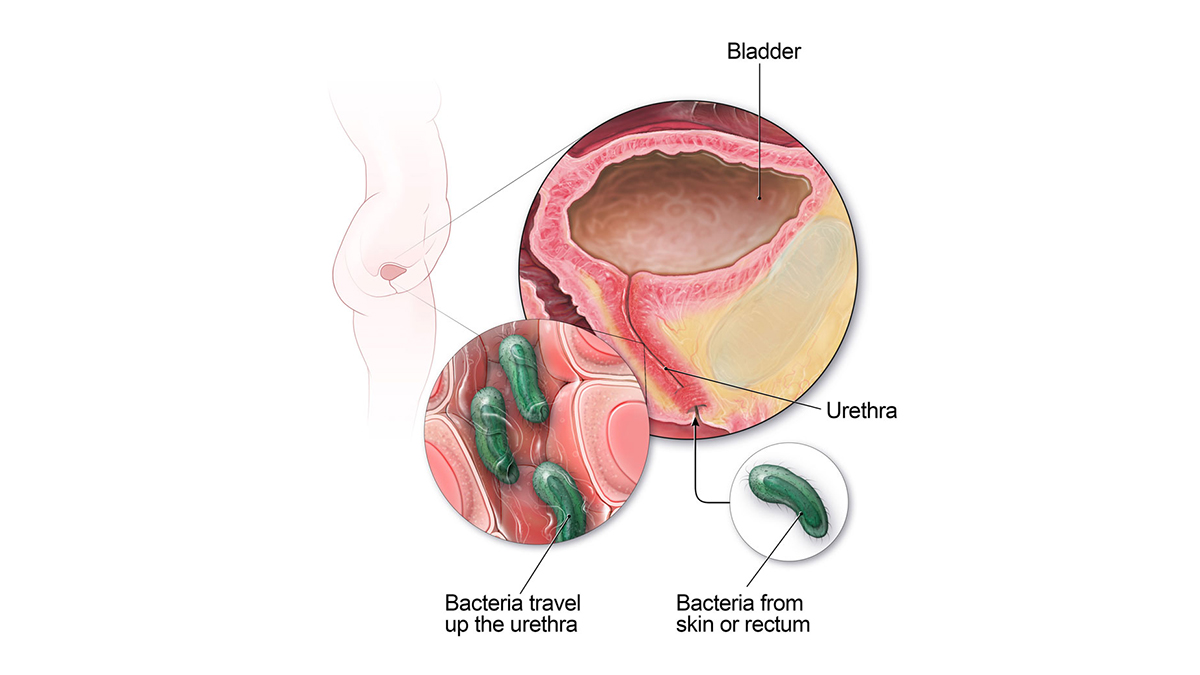
Types and strains
- Bladder infection (most common, also known as cystitis).
- Kidney infection (less common but more serious, also known as pyelonephritis).
Signs and symptoms
Symptoms of a bladder infection can include:
- Pain or burning while urinating
- Frequent urination
- Feeling the need to urinate despite having an empty bladder
- Bloody urine
- Pressure or cramping in the groin or lower abdomen
Symptoms of a kidney infection can include:
- Lower back pain or pain in the side of your back
- Nausea or vomiting
Younger children may not be able to tell you about UTI symptoms they are having. While fever is the most common sign of UTI in infants and toddlers, most children with fever do not have a UTI.
Risk factors
UTIs are more common in females because their urethras are shorter and closer to the rectum. This makes it easier for bacteria to enter the urinary tract.
Other risk factors:
- A previous UTI.
- Recent sexual activity.
- Changes in the bacteria that live inside the vagina or vaginal flora. For example, menopause or the use of spermicides can cause these bacterial changes.
- Age (older adults and young children are more likely to get UTIs).
- Structural problems in the urinary tract, such as enlarged prostate.
- Poor hygiene, for example, in children who are potty-training.
- Urinate after sexual activity.
- Stay well hydrated.
- Take showers instead of baths.
- Minimize douching, sprays or powders in the genital area.
- Teach girls when potty training to wipe front to back.
When to seek medical care
- If you or your child have symptoms of a UTI or for any symptom that is severe or concerning.
Talk to your healthcare provider right away
Your healthcare provider will determine if you have a UTI by:
- Asking about symptoms.
- Doing a physical exam.
- Ordering urine tests, if needed.
- Starting an antibiotic to treat a UTI, if needed.
- Taking antibiotics, prescribed by a healthcare provider, at home can treat most UTIs. Your healthcare provider might also recommend medicine to help lessen the pain or discomfort. Some cases may require treatment in a hospital.
Any time you take antibiotics, they can cause side effects.
- Side effects can include rash, dizziness, nausea, diarrhea and yeast infections.
- More serious side effects can include antimicrobial-resistant infections or C. diff infection, which causes diarrhea that can lead to severe colon damage and death.
Call your healthcare provider if you develop any side effects while taking your antibiotic.
How to feel better
- Drink plenty of water or other fluids.
- Take antibiotics exactly as your healthcare provider tells you.
- Do not share your antibiotics with others.
- Do not save antibiotics for later. Talk to your healthcare provider about safely discarding leftover antibiotics.
Talk with your healthcare provider if you have any questions about your antibiotics.
Similar diseases
- Sexually transmitted diseases
For more on treatment of common illnesses, visit CDC resources:
- Acute Bronchitis
- Ear Infection
- Sinus Infection
- Sore Throat
- Common Cold Fact Sheet
- Skin Infection Fact Sheet
A urinary tract infection, when germs infect the urinary tract, is usually treated with antibiotics. Learn the signs and symptoms.
For Everyone
Health care providers.
- Skip to main content
- Skip to "About this site"
Language selection
Search travel.gc.ca.
Help us to improve our website. Take our survey !
COVID-19: travel health notice for all travellers
Russia travel advice
Latest updates: Editorial change
Last updated: May 23, 2024 08:00 ET
On this page
Safety and security, entry and exit requirements, laws and culture, natural disasters and climate, russia - avoid all travel.
The armed conflict in Ukraine has led to armed incursions and shelling in areas close to the Russian-Ukrainian border. Drone strikes, explosions, and fires have occurred further into Russia’s interior. The impacts of the armed conflict with Ukraine could also include:
- partial military mobilization
- restrictions on financial transactions
- increasingly limited flight options
If you are in Russia, you should leave while commercial means are still available. If you remain in Russia, maintain a low profile. Canadians holding Russian citizenship may be subject to call-up for mandatory military service.
Back to top
Terrorist attack in Krasnogorsk, Moscow Oblast
On March 22, 2024, a terrorist attack occurred at the Crocus City Hall, a concert venue in Krasnogorsk, just outside central Moscow. There are reports of gunfire and explosions. The incident resulted in multiple casualties and fires continue to burn around the site of the attack.
Local authorities have cordoned off the affected area and have cancelled upcoming mass gatherings in Moscow. Further attacks could occur at any time.
If you are in Moscow Oblast:
- avoid the affected area
- follow the instructions of local authorities
- exercise extreme caution in public and avoid large gatherings
- contact the Embassy of Canada to Russia, in Moscow, if you require consular emergency assistance
Armed conflict with Ukraine
On June 24, 2023, there were reports of military tensions in the Rostov region.
Flight availability, already reduced following Russia’s full-scale invasion of Ukraine, continues to be subject to unpredictable and significant limitations. If you are in Russia, you should leave while commercial means are still available.
Some financial transactions, including those with Canadian major credit and ATM cards, are not possible. As a result, you may not be able to use your credit card for purchases within Russia or to withdraw cash at an ATM. Availability of essential services may also be affected.
Communications related to the current situation are scrutinized by local authorities. You may face heavy consequences if you discuss, share or publish information related to the Russian invasion of Ukraine. Foreign journalists and other media workers in Russia may also face considerable risks.
Security conditions are unpredictable and could deteriorate without notice. The ability of our Embassy to provide consular services in Russia may become severely limited.
There have been armed incursions and shelling in areas close to the Russian-Ukrainian border, notably in Bryansk and Belgorod Oblasts. Drone strikes, explosions and fires have also occurred at key infrastructure sites and military installations further into Russia's interior and in cities, including in Moscow and St. Petersburg.
You may encounter an increased security presence with potential disruptions to transport and movement, especially in areas near Russian military installations.
Avoid all travel to Russia. If you decide to remain despite this advisory, be aware that:
- you may have to stay in Russia longer than expected
- you may be affected by shortages of essential products and services
- you may not be able to use your banking cards for payment or to withdraw funds
- you should not depend on the Government of Canada to help you leave the country
Additionally, while you remain in Russia, you should:
- review your personal security plans on a daily basis
- keep a low profile
- refrain from discussing political developments in public or online
- avoid areas where demonstrations and large gatherings are taking place
- make sure you have an adequate supply of cash, essential items and medications
- avoid any area where there are military installations or activity
- monitor trustworthy news sources to stay informed on the evolving situation
- make sure your travel documents are up-to-date, including those of your family
- contact your air company to check on flight availability
- communicate your travel plans to family and friends
- register and update your contact information through the Registration of Canadians Abroad service and encourage other Canadian citizens in Russia to do so
Rostov Oblast
The Russian government has declared a state of emergency and maintains a significant military presence in Rostov Oblast. The situation along the Ukrainian border is unpredictable and could change quickly. Exercise extreme vigilance if you must travel to this region, as armed clashes and violence pose serious threats to your safety. If you are currently in this area, you should strongly consider leaving. The ability of the Embassy of Canada to Russia in Moscow to provide consular assistance in this district is extremely limited.
Republics of Chechnya, Dagestan and Ingushetia, and Stavropol Krai
Terrorist attacks are frequent in the Chechnya, Dagestan and Ingushetia republics and Stavropol region. The security situation is unstable and dangerous. Suicide bombings occur on a regular basis and targeted assassinations have also taken place. Unexploded mines and munitions are widespread. Kidnapping for ransom is also common.
You must obtain special permission from the Ministry of the Interior to enter certain areas and regions.
Republics of Kabardino-Balkaria (including the Mount Elbrus region), Karachai-Cherkessia and North Ossetia
Tensions are high in Russia’s border regions with Georgia and may affect the security situation in Kabardino-Balkaria, Karachai-Cherkessia and North Ossetia republics. Military operations are carried out with little or no notice, and are accompanied by travel restrictions. The border crossings to Azerbaijan and Georgia are subject to frequent, sometimes lengthy closures.
There is a threat of terrorism. Terrorist groups have called for attacks on Russian soil. Incidents resulting in death and injury have occurred most frequently in the North Caucasus region, Moscow and St. Petersburg, but may happen throughout the country. Terrorist attacks could occur at any time.
Targets could include:
- government buildings, including schools
- cultural venues, including concert halls, nightclubs, and event centres
- places of worship
- Russian airlines, airports and other transportation hubs and networks
- public areas such as tourist attractions, restaurants, bars, coffee shops, shopping centres, markets, hotels and other sites frequented by foreigners
Always be aware of your surroundings when in public places.
Russian authorities have increased general security measures in Moscow and other large cities.
Violent crime
Crime against foreigners is a serious problem. Harassment and assaults are prevalent, particularly against foreigners of Asian and African descent. Some victims have died as a result of assaults. Foreigners in the areas to which we advise against all travel are particularly vulnerable. Several journalists and foreign aid personnel working in Russia have been killed or kidnapped. Criminals have targeted and destroyed well-marked aid convoys. Exercise extreme caution in crowds and open markets.
Petty crime
Petty crime, such as pickpocketing and purse snatching, occurs frequently and is often committed by groups of children and teenagers. Criminals use various techniques to distract the victims, including requests for help. In such situations, walk away quickly. Preferred areas for criminals include:
- underground walkways
- public transportation and transportation hubs
- tourist sites
- restaurants and markets
- hotel rooms and residences (even when occupied and locked)
Reduce your risk of being targeted by travelling in groups with reputable tour agencies.
Avoid showing signs of affluence and ensure personal belongings, including passports and other travel documents, are secure at all times. Replacing travel documents and visas is difficult, and could considerably delay your return to Canada.
Criminal strategies
Criminals may also pose as police officers, particularly in St. Petersburg. Real police officers wear a visible personal identification number on their uniforms. Bogus checkpoints may be set up in rural areas to commit robbery.
Demonstrations and elections
Demonstrations take place. Even peaceful demonstrations can turn violent at any time. They can also lead to disruptions to traffic and public transportation.
- Avoid areas where demonstrations and large gatherings are taking place
- Follow the instructions of local authorities
- Monitor local media for the latest information
Due to heightened political tensions, be vigilant and don’t discuss political developments in public.
Useful links
- More about mass gatherings (large-scale events)
- Laws regarding minors involved in demonstrations
Tensions on the Korean Peninsula
Tensions on the neighbouring Korean Peninsula could escalate with little notice and the security situation could deteriorate suddenly. Tensions may increase before, during and after North Korean nuclear and missile tests, military exercises or as the result of incidents or military activities at or near the inter-Korean border. Monitor developments, remain vigilant and follow the instructions of local authorities.
Spiked food and drinks
Never leave food or drinks unattended or in the care of strangers. Be wary of accepting snacks, beverages, gum or cigarettes from new acquaintances. These items may contain drugs that could put you at risk of sexual assault and robbery.
There have been cases of foreigners developing friendships or romantic relationships over the Internet and becoming entangled in financial issues in Russia. Remain vigilant and be aware that we can’t help you recover lost funds or property in such cases.
Only exchange money at major banks. Foreigners have been scammed in the past when exchanging money on the street.
Traffic police may stop motorists to collect fraudulent cash fines on the spot.
Credit card and automated banking machine (ABM) fraud occurs. Be cautious when using debit or credit cards:
- pay careful attention when your cards are being handled by others
- use ATMs located in well-lit public areas or inside a bank or business
- avoid using card readers with an irregular or unusual feature
- cover the keypad with one hand when entering your PIN
- check for any unauthorized transactions on your account statements
Overseas fraud
Organized crime
Organized criminal groups are active throughout Russia, particularly in large cities. Extortion and corruption are common business practices, including among foreign businesses. Criminals demand protection money from their victims under threat of serious violence. Report extortion attempts to Russian authorities.
Surveillance
Authorities may place foreigners under surveillance. Hotel rooms, telephones, fax machines and e-mail messages may be monitored. Personal possessions in hotel rooms may be searched.
Power outages
Power outages and shortages occur often throughout Russia.
2SLGBTQI+ travellers
Discrimination against 2SLGBTQI+ individuals is common.
2SLGBTQI+ travellers, as well as their friends and families, have been targets of harassment and violence, particularly outside of Moscow.
Travel and your sexual orientation, gender identity, gender expression and sex characteristics
Road safety
Road conditions vary and are often poor outside major cities.
Drivers don’t respect traffic laws and often drive and park on pedestrian areas. Accidents are common. Pedestrians should be particularly careful. In the event of an accident, don’t move the vehicle until the police arrive, even if the car is obstructing traffic.
Drive only during the day.
In winter, road travel can be hazardous due to ice and snow.
Public transportation
When travelling by train, store valuables in a safe place and don’t leave the compartment unattended. Lock the door from the inside.
Most major cities have reliable public transportation including buses, subways or streetcars.
Use only registered taxis and don’t share a taxi with strangers. Foreigners have been victims of assault and robbery when using unregistered taxis.
Book taxis in advance either by phone or through taxi company apps. Avoid flagging down taxis on the street, but if you do, negotiate the price before getting into the taxi.
Marine transportation
Boat accidents are common due to the overloading and poor maintenance of some vessels. Safety standards differ from those in Canada. Exercise caution and common sense when using marine transportation. Don’t board vessels that appear overloaded or unseaworthy.
We do not make assessments on the compliance of foreign domestic airlines with international safety standards.
Information about foreign domestic airlines
Every country or territory decides who can enter or exit through its borders. The Government of Canada cannot intervene on your behalf if you do not meet your destination’s entry or exit requirements.
We have obtained the information on this page from the Russian authorities. It can, however, change at any time.
Verify this information with the Foreign Representatives in Canada .
border_crossings_with_finland
Border crossings with Finland
Finnish authorities have closed border crossings along the land border with Russia. As of December 15, 2023, all land border crossings are closed.
Contact information and hours of operation – Finnish Border Guard
Entry requirements vary depending on the type of passport you use for travel.
Before you travel, check with your transportation company about passport requirements. Its rules on passport validity may be more stringent than the country’s entry rules.
Regular Canadian passport
Your passport must be valid for at least 6 months beyond the date you expect to leave Russia.
Passport for official travel
Different entry rules may apply.
Official travel
Passport with “X” gender identifier
While the Government of Canada issues passports with an “X” gender identifier, it cannot guarantee your entry or transit through other countries. You might face entry restrictions in countries that do not recognize the “X” gender identifier. Before you leave, check with the closest foreign representative for your destination.
Other travel documents
Different entry rules may apply when travelling with a temporary passport or an emergency travel document. Before you leave, check with the closest foreign representative for your destination.
- Foreign Representatives in Canada
- Canadian passports
Tourist visa: required for stays in commercial accommodations (exceptions apply) Guest visa: required for stays in private accommodations Business visa: required Student visa: required Transit visa: required (exceptions apply) Exit visa: required
You must be submitted your visa request online to the Embassy of the Russian Federation.
Foreign visitors must leave Russia once the visa validity period has ended. To extend a visa, a foreign national must arrange with the territorial units of the migration service authorities prior to the validity end date to start the extension process.
Embassy of the Russian Federation
Tourist visa
You need a tourist visa if you are staying at a hotel or other commercial establishment. Ensure that the hotel registers your visa when you check in.
It is best if you book your travel through a travel agency, which will submit a tourist visa application on your behalf. Canadian travel agents work with Russian travel agencies or companies, which act as sponsors for tourist visas.
In cases of expired tourist visas or lost or stolen Canadian passports, only the visa-sponsoring travel agency is authorized to apply for a new tourist visa on your behalf. Extensions are not issued. Holders of expired visas face heavy fines or detention upon departure.
Guest visas
You need a guest visa if you intend to stay in private accommodations. The host must obtain an official invitation (priglashenie) from the nearest Russian visa and passport office (UFMS) and send it to you in Canada. You must then take the invitation, the visa application and your passport to a Russian embassy or consulate to apply for the visa.
Foreign diplomatic missions and consulates in Canada
Business visa
To get a business visa, you need to be sponsored by a Russian individual or organization (the host). It may take up to 3 months for the host to obtain approval for sponsorship from the Ministry of the Interior. Any subsequent change (replacement or extension) to the original visa must be made by the sponsor. A business visa is not a work permit.
You must have a valid visa to be allowed to leave Russia. If your visa expires, your sponsor must apply for an exit visa on your behalf. To avoid problems, including deportation, make sure your visa is valid beyond your intended departure date.
Visa exceptions
Contact your cruise company to find out if you need to apply for a Russian visa before your cruise starts. International cruise passengers may enter Russia at specific port cities without a visa for up to 72 hours. Your cruise ship tour guide must have all the authorizations required for your entry by the Russian authorities. While in Russia, make sure that you’re able to contact your cruise ship tour guide at any time, in case of emergency or any issue with local authorities.
Some Russian international airports have transit areas that allow for visa-free travel through Russia. If you plan to transit through Russia, check with your transportation carrier to see if transit visa exceptions apply to you.
Migration card
You must complete a migration card upon your arrival in Russia. These cards are usually distributed on flights and trains entering Russia or at points of entry, but sometimes they are not available, even at major international airports. Even if that’s the case, you are responsible to find a migration card and fill it out. You must keep and carry part B of the migration card throughout your stay. The card is required for hotel registration.
If the police request to see your migration card, you must comply. You must present it, your passport and your registered visa. You must also present the card to border officials upon departure.
If you hold a multiple-entry visa, you must fill out a new migration card every time you enter Russia.
Loss of this card can result in fines, serious delays or imprisonment at the time of departure.
Registration
All foreign visitors must register their arrival within 72 hours of entering the country (excluding weekends and national holidays). If you have made accommodation arrangements with a hotel for your entire trip, the hotel will take care of registering your stay with the authorities.
Visitors staying in private accommodations must register with the territorial office of the Federal Migration Service. Any Russian citizen with a resident registration (propiska) can register a foreigner staying at their home at a local police station or any post office. A small registration fee may apply. The visitor’s host must be present during the process.
Violation of the rules of migration registration may result in a fine. In some cases, visitors may face expulsion from Russia and a ban from re-entering of up to 5 years.
Customs declaration form
Upon arrival in Russia, you must fill out a customs declaration form, then go through the red customs line and have the form stamped by a customs official. Without the stamp, any undeclared currency and valuables—including items that could be considered antique—may be confiscated upon departure.
You must declare amounts of currency exceeding US$10,000 at border crossings. You may also have to provide information on the origin of the money and its intended use. Currency exceeding the amount stated on the declaration form will be confiscated if you have not obtained an official bank receipt authorizing the clearance of these sums. The declaration form must be kept until departure.
Upon departure, you must fill out a second customs declaration form and present the two forms to a customs official. You must declare any amount greater than RUB3,000. If you fail to declare, in writing, the amount of currency in your possession, the undeclared currency and valuables may be confiscated and you may be detained and face criminal charges leading to imprisonment.
Special permits and restricted areas
Travel to and residency in several Russian cities and regions is restricted. You must obtain permission from local authorities prior to entering a restricted city or region. Failure to do so may result in arrest, fines and/or deportation. Attach an itinerary to your visa application to avoid delays. Some areas must be specifically indicated in the visa, and you may have to pay an extra fee to include them.
Passport requirements for individuals holding both Canadian and Russian citizenships
If you have dual citizenship, you must enter and leave Russia on a Russian passport.
If your Russian passport expires prior travelling to Russia, Russian authorities in Canada can extend it for entry into Russia only. If the passport expires during your stay in Russia, you must obtain a new one before leaving. Renewing a Russian passport may take several months.
If you enter Russia with a repatriation certificate issued by Russian authorities abroad, you may not be allowed to leave on a Canadian passport. This certificate is only valid for one-way travel into Russia.
Entry ban on vehicles with Russian license plates
In September 2023, the Baltic States (Latvia, Estonia and Lithuania) and Finland announced a ban on vehicles with Russian license plates entering their respective territories. The ban is enforced at the border as a result of existing European Union sanctions on the Russian Federation. Lithuania will allow an exception for travellers able to prove transit to the Russian exclave of Kaliningrad.
Other countries from the EU or the Schengen area have introduced similar bans. You should confirm with local authorities before travelling to the EU or Schengen area.
Land border with Belarus
Only local residents are allowed to travel by land from Russia to Belarus. This restriction applies to cars, tour buses and trains.
Health entry requirements
If you are planning to remain in Russia for more than 3 months, you must provide a medical certificate of a negative test for HIV infection. The certificate must be valid for 3 months from the date of testing and include:
- passport details (full name, date of birth, passport number and country of residence)
- HIV test information (date of test, test results and signatures of the doctor who performed the test and the person examined)
- the length of your intended stay in Russia
Other tests (such as for tuberculosis and leprosy) may be required for individuals staying in Russia for more than 3 months.
Children and travel
Learn more about travelling with children .
Yellow fever
Learn about potential entry requirements related to yellow fever (vaccines section).
Relevant Travel Health Notices
- Global Measles Notice - 13 March, 2024
- COVID-19 and International Travel - 13 March, 2024
This section contains information on possible health risks and restrictions regularly found or ongoing in the destination. Follow this advice to lower your risk of becoming ill while travelling. Not all risks are listed below.
Consult a health care professional or visit a travel health clinic preferably 6 weeks before you travel to get personalized health advice and recommendations.
Routine vaccines
Be sure that your routine vaccinations , as per your province or territory , are up-to-date before travelling, regardless of your destination.
Some of these vaccinations include measles-mumps-rubella (MMR), diphtheria, tetanus, pertussis, polio, varicella (chickenpox), influenza and others.
Pre-travel vaccines and medications
You may be at risk for preventable diseases while travelling in this destination. Talk to a travel health professional about which medications or vaccines may be right for you, based on your destination and itinerary.
Yellow fever is a disease caused by a flavivirus from the bite of an infected mosquito.
Travellers get vaccinated either because it is required to enter a country or because it is recommended for their protection.
- There is no risk of yellow fever in this country.
Country Entry Requirement*
- Proof of vaccination is not required to enter this country.
Recommendation
- Vaccination is not recommended.
* It is important to note that country entry requirements may not reflect your risk of yellow fever at your destination. It is recommended that you contact the nearest diplomatic or consular office of the destination(s) you will be visiting to verify any additional entry requirements.
About Yellow Fever
Yellow Fever Vaccination Centres in Canada
There is a risk of hepatitis A in this destination. It is a disease of the liver. People can get hepatitis A if they ingest contaminated food or water, eat foods prepared by an infectious person, or if they have close physical contact (such as oral-anal sex) with an infectious person, although casual contact among people does not spread the virus.
Practise safe food and water precautions and wash your hands often. Vaccination is recommended for all travellers to areas where hepatitis A is present.
Tick-borne encephalitis (TBE) is a risk in some areas of this destination. It is a viral disease that affects the central nervous system (brain and spinal cord). It is spread to humans by the bite of infected ticks or occasionally when unpasteurized milk products are consumed.
Travellers to areas where TBE is found may be at higher risk during April to November, and the risk is highest for people who hike or camp in forested areas.
Protect yourself from tick bites . The vaccine is not available in Canada. It may be available in the destination you are travelling to.
Measles is a highly contagious viral disease. It can spread quickly from person to person by direct contact and through droplets in the air.
Anyone who is not protected against measles is at risk of being infected with it when travelling internationally.
Regardless of where you are going, talk to a health care professional before travelling to make sure you are fully protected against measles.
Japanese encephalitis is a viral infection that can cause swelling of the brain. It is spread to humans through the bite of an infected mosquito. Risk is very low for most travellers. Travellers at relatively higher risk may want to consider vaccination for JE prior to travelling.
Travellers are at higher risk if they will be:
- travelling long term (e.g. more than 30 days)
- making multiple trips to endemic areas
- staying for extended periods in rural areas
- visiting an area suffering a JE outbreak
- engaging in activities involving high contact with mosquitos (e.g., entomologists)
Hepatitis B is a risk in every destination. It is a viral liver disease that is easily transmitted from one person to another through exposure to blood and body fluids containing the hepatitis B virus. Travellers who may be exposed to blood or other bodily fluids (e.g., through sexual contact, medical treatment, sharing needles, tattooing, acupuncture or occupational exposure) are at higher risk of getting hepatitis B.
Hepatitis B vaccination is recommended for all travellers. Prevent hepatitis B infection by practicing safe sex, only using new and sterile drug equipment, and only getting tattoos and piercings in settings that follow public health regulations and standards.
Coronavirus disease (COVID-19) is an infectious viral disease. It can spread from person to person by direct contact and through droplets in the air.
It is recommended that all eligible travellers complete a COVID-19 vaccine series along with any additional recommended doses in Canada before travelling. Evidence shows that vaccines are very effective at preventing severe illness, hospitalization and death from COVID-19. While vaccination provides better protection against serious illness, you may still be at risk of infection from the virus that causes COVID-19. Anyone who has not completed a vaccine series is at increased risk of being infected with the virus that causes COVID-19 and is at greater risk for severe disease when travelling internationally.
Before travelling, verify your destination’s COVID-19 vaccination entry/exit requirements. Regardless of where you are going, talk to a health care professional before travelling to make sure you are adequately protected against COVID-19.
The best way to protect yourself from seasonal influenza (flu) is to get vaccinated every year. Get the flu shot at least 2 weeks before travelling.
The flu occurs worldwide.
- In the Northern Hemisphere, the flu season usually runs from November to April.
- In the Southern Hemisphere, the flu season usually runs between April and October.
- In the tropics, there is flu activity year round.
The flu vaccine available in one hemisphere may only offer partial protection against the flu in the other hemisphere.
The flu virus spreads from person to person when they cough or sneeze or by touching objects and surfaces that have been contaminated with the virus. Clean your hands often and wear a mask if you have a fever or respiratory symptoms.
In this destination, rabies is carried by dogs and some wildlife, including bats. Rabies is a deadly disease that spreads to humans primarily through bites or scratches from an infected animal. While travelling, take precautions , including keeping your distance from animals (including free-roaming dogs), and closely supervising children.
If you are bitten or scratched by an animal while travelling, immediately wash the wound with soap and clean water and see a health care professional. Rabies treatment is often available in this destination.
Before travel, discuss rabies vaccination with a health care professional. It may be recommended for travellers who are at high risk of exposure (e.g., occupational risk such as veterinarians and wildlife workers, children, adventure travellers and spelunkers, and others in close contact with animals).
Safe food and water precautions
Many illnesses can be caused by eating food or drinking beverages contaminated by bacteria, parasites, toxins, or viruses, or by swimming or bathing in contaminated water.
- Learn more about food and water precautions to take to avoid getting sick by visiting our eat and drink safely abroad page. Remember: Boil it, cook it, peel it, or leave it!
- Avoid getting water into your eyes, mouth or nose when swimming or participating in activities in freshwater (streams, canals, lakes), particularly after flooding or heavy rain. Water may look clean but could still be polluted or contaminated.
- Avoid inhaling or swallowing water while bathing, showering, or swimming in pools or hot tubs.
Travellers' diarrhea is the most common illness affecting travellers. It is spread from eating or drinking contaminated food or water.
Risk of developing travellers' diarrhea increases when travelling in regions with poor standards of hygiene and sanitation. Practise safe food and water precautions.
The most important treatment for travellers' diarrhea is rehydration (drinking lots of fluids). Carry oral rehydration salts when travelling.
Insect bite prevention
Many diseases are spread by the bites of infected insects such as mosquitoes, ticks, fleas or flies. When travelling to areas where infected insects may be present:
- Use insect repellent (bug spray) on exposed skin
- Cover up with light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- Minimize exposure to insects
- Use mosquito netting when sleeping outdoors or in buildings that are not fully enclosed
To learn more about how you can reduce your risk of infection and disease caused by bites, both at home and abroad, visit our insect bite prevention page.
Find out what types of insects are present where you’re travelling, when they’re most active, and the symptoms of the diseases they spread.
Crimean-Congo haemorrhagic fever is a viral disease that can cause fever, pain and bleeding under the skin. In some cases, it can be fatal. It spreads to humans through contact with infected animal blood or tissues, or from the bite of an infected tick. Risk is generally low for most travellers. Protect yourself from tick bites and avoid animals, particularly livestock. There is no vaccine available for Crimean-Congo haemorrhagic fever.
Animal precautions
Some infections, such as rabies and influenza, can be shared between humans and animals. Certain types of activities may increase your chance of contact with animals, such as travelling in rural or forested areas, camping, hiking, and visiting wet markets (places where live animals are slaughtered and sold) or caves.
Travellers are cautioned to avoid contact with animals, including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats, and to avoid eating undercooked wild game.
Closely supervise children, as they are more likely to come in contact with animals.
Human cases of avian influenza have been reported in this destination. Avian influenza is a viral infection that can spread quickly and easily among birds and in rare cases it can infect mammals, including people. The risk is low for most travellers.
Avoid contact with birds, including wild, farm, and backyard birds (alive or dead) and surfaces that may have bird droppings on them. Ensure all poultry dishes, including eggs and wild game, are properly cooked.
Travellers with a higher risk of exposure include those:
- visiting live bird/animal markets or poultry farms
- working with poultry (such as chickens, turkeys, domestic ducks)
- hunting, de-feathering, field dressing and butchering wild birds and wild mammals
- working with wild birds for activities such as research, conservation, or rehabilitation
- working with wild mammals, especially those that eat wild birds (e.g., foxes)
All eligible people are encouraged to get the seasonal influenza shot, which will protect them against human influenza viruses. While the seasonal influenza shot does not prevent infection with avian influenza, it can reduce the chance of getting sick with human and avian influenza viruses at the same time.
Person-to-person infections
Stay home if you’re sick and practise proper cough and sneeze etiquette , which includes coughing or sneezing into a tissue or the bend of your arm, not your hand. Reduce your risk of colds, the flu and other illnesses by:
- washing your hands often
- avoiding or limiting the amount of time spent in closed spaces, crowded places, or at large-scale events (concerts, sporting events, rallies)
- avoiding close physical contact with people who may be showing symptoms of illness
Sexually transmitted infections (STIs) , HIV , and mpox are spread through blood and bodily fluids; use condoms, practise safe sex, and limit your number of sexual partners. Check with your local public health authority pre-travel to determine your eligibility for mpox vaccine.
Tuberculosis is an infection caused by bacteria and usually affects the lungs.
For most travellers the risk of tuberculosis is low.
Travellers who may be at high risk while travelling in regions with risk of tuberculosis should discuss pre- and post-travel options with a health care professional.
High-risk travellers include those visiting or working in prisons, refugee camps, homeless shelters, or hospitals, or travellers visiting friends and relatives.
Medical services and facilities
Good health care is only available in major cities. Quality of care varies greatly throughout the country. A few quality facilities exist in larger cities and usually require cash payment upon admission. Medical evacuation, which can be very expensive, may be necessary in the event of serious illness or injury.
Make sure you get travel insurance that includes coverage for medical evacuation and hospital stays.
Travel health and safety
Keep in Mind...
The decision to travel is the sole responsibility of the traveller. The traveller is also responsible for his or her own personal safety.
Be prepared. Do not expect medical services to be the same as in Canada. Pack a travel health kit , especially if you will be travelling away from major city centres.
You must abide by local laws.
Learn about what you should do and how we can help if you are arrested or detained abroad .
Identification
Authorities frequently perform random identity checks in public places.
You must carry the following identification documents at all times:
- a valid passport with 2 blank pages for stamps
- a valid Russian visa
- an migration card
- a stamped registration notification
You may be fined or detained for failing to provide proper documentation to Russian authorities.
Only the special police of the Federal Migration Bureau have the authority to arrest, detain and impose fines on improperly documented foreigners. If you are stopped in the street and requested to pay a fine, ask to see the officer’s name and identification and to contact the Embassy of Canada to Russia in Moscow.
Penalties for possession, use or trafficking of illegal drugs are severe. Convicted offenders can expect jail sentences and heavy fines.
Drugs, alcohol and travel
Minors participating in demonstrations
It is illegal for minors (those under 18) to participate in unauthorized protests. Adults who involve minors in such protests could face up to 15 days in jail and fines of up to RUB1 million.
Although the laws of Russia do not prohibit homosexual activity, Russian federal law prohibits public actions that are described as promoting homosexuality and “non-traditional sexual relations.”
Public actions that contravene or appear to contravene this law may lead to arrest, a fine and deportation. Examples of such actions include dissemination of information (for example, through public statements) and public displays of affection. Same sex marriage is not recognized in Russia. Homosexuality isn’t socially accepted.
Dual citizenship
Dual citizenship is not legally recognized in Russia.
If local authorities consider you a citizen of Russia, they may refuse to grant you access to Canadian consular services. This will prevent us from providing you with those services.
If you are also a Russian citizen and reside in Russia or hold permanent residency status in another country, you must declare this citizenship or residency status to your local migration office.
You may also be subject to certain legal obligations, including military service. You may be detained, imprisoned, or fined larges sums if you try to avoid military service. Seek advice from the nearest Russian embassy or consulate before travelling to Russia, or consult official sources from the Government of the Russian Federation.
- Official information - Government of the Russian Federation ( may not be currently available depending on your location)
- Military mobilization - Government of the Russian Federation (may not be currently available depending on your location)
- Requirement and consequences of non-compliance with the declaration of foreign citizenship - Federal Migration Service of the Russian Federation (in Russian, may not be currently available depending on your location)
- General information for travellers with dual citizenship
International Child Abduction
The Hague Convention on the Civil Aspects of International Child Abduction is an international treaty. It can help parents with the return of children who have been removed to or retained in certain countries in violation of custody rights. It does not apply between Canada and Russia.
If your child was wrongfully taken to, or is being held in Russia by an abducting parent:
- act as quickly as you can
- consult a lawyer in Canada and in Russia to explore all the legal options for the return of your child
- report the situation to the nearest Canadian government office abroad or to the Vulnerable Children’s Consular Unit at Global Affairs Canada by calling the Emergency Watch and Response Centre
If your child was removed from a country other than Canada, consult a lawyer to determine if The Hague Convention applies.
Be aware that Canadian consular officials cannot interfere in private legal matters or in another country’s judicial affairs.
- International Child Abduction: A Guidebook for Left-Behind Parents
- Travelling with children
- Canadian embassies and consulates by destination
- Emergency Watch and Response Centre
Religious activity
Religious activity is heavily regulated in Russia. If you plan to engage in religious activity, such as missionary work, make sure you are not inadvertently violating local laws.
You should carry an international driving permit.
International Driving Permit
You may drive with a Canadian driver’s licence if you carry it and a Russian translation. You must obtain a local permit if staying longer than 6 months.
The legal blood alcohol content limit is significantly lower than in Canada. Those found guilty of drinking and driving can expect heavy fines, suspension of their driving permit and immediate detention. Repeat offenders may face prison sentences.
The traffic police can impose fines on drivers for traffic violations. They can conduct identity checks on pedestrians, but they are not authorized to impose fines. The same is true of police in the underground metro systems.
Russia has very strict rules on the importation of medication. Certain prescription and over-the-counter drugs that are common in Canada may be prohibited, and large quantities of any medicine will be scrutinized.
If you are travelling with medication, even over-the-counter medication, you must have a doctor’s note translated to Russian confirming that you need the medication. Contact the Embassy of the Russian Federation for up-to-date information.
Imports and exports
The importation and use of electronic equipment are strictly controlled. Foreigners have faced charges of espionage for possessing improperly certified GPS devices, such as those used for geological mapping.
You must obtain a certificate from the Ministry of Culture to export items that appear old (prior to 1945) or may have cultural value. Customs officials may conduct thorough baggage searches and can arrest you if you don’t have the necessary certificate.
Contact the nearest Russian embassy or consulate, or consult the Federal Customs Service prior to departure for up-to-date information on customs requirements.
The currency of Russia is the Russian ruble (RUB).
It is illegal to pay for goods and services in foreign currency. You can exchange U.S. dollars at any exchange counter. Carry new, crisp bills; well-worn or used U.S. banknotes may not be accepted. ATMs are common in main cities. ATMs will accept cards with 4-digit pin numbers, but you may experience problems with cards with 5- or 6-digit pin codes. In major cities, you can usually exchange Euros and U.S. dollars at various banks.
Forest fires
Forest fires are common between July and September, particularly in Siberia. The air quality in areas near active fires may deteriorate due to heavy smoke.
In case of a major fire:
- stay away from the affected area, particularly if you suffer from respiratory ailments
- follow the instructions of local emergency services
- monitor local media for up-to-date information on the situation
Seismic activity
Parts of Russia, such as Chechnya, the Kamchatka Peninsula and the Kuril Islands, are prone to seismic or volcanic activity.
Spring flooding throughout Siberia and parts of western Russia.
Local services
In case of emergency, dial 112 or:
- police: 102
- medical assistance: 103
- firefighters: 101
Consular assistance
Armenia (Consular and Trade Commissioner services)
For calls originating inside Russia the “7” should be replaced by an “8”.
For emergency consular assistance, call the Embassy of Canada in Moscow and follow the instructions. At any time, you may also contact the Emergency Watch and Response Centre in Ottawa.
The decision to travel is your choice and you are responsible for your personal safety abroad. We take the safety and security of Canadians abroad very seriously and provide credible and timely information in our Travel Advice to enable you to make well-informed decisions regarding your travel abroad.
The content on this page is provided for information only. While we make every effort to give you correct information, it is provided on an "as is" basis without warranty of any kind, expressed or implied. The Government of Canada does not assume responsibility and will not be liable for any damages in connection to the information provided.
If you need consular assistance while abroad, we will make every effort to help you. However, there may be constraints that will limit the ability of the Government of Canada to provide services.
Learn more about consular services .
Risk Levels
take normal security precautions.
Take similar precautions to those you would take in Canada.
Exercise a high degree of caution
There are certain safety and security concerns or the situation could change quickly. Be very cautious at all times, monitor local media and follow the instructions of local authorities.
IMPORTANT: The two levels below are official Government of Canada Travel Advisories and are issued when the safety and security of Canadians travelling or living in the country or region may be at risk.
Avoid non-essential travel
Your safety and security could be at risk. You should think about your need to travel to this country, territory or region based on family or business requirements, knowledge of or familiarity with the region, and other factors. If you are already there, think about whether you really need to be there. If you do not need to be there, you should think about leaving.
Avoid all travel
You should not travel to this country, territory or region. Your personal safety and security are at great risk. If you are already there, you should think about leaving if it is safe to do so.
- Share full article

Do I Need That Antibiotic?
If it’s not medically necessary, you may want to consider the risk of antimicrobial resistance.
Credit... Eric Helgas for The New York Times
Supported by
By Anna Gibbs
- Published May 14, 2024 Updated May 17, 2024
Q: I was prescribed a yearlong course of antibiotics to prevent recurrent urinary tract infections. Should I be worried about antimicrobial resistance?
Whenever you take antibiotics, no matter the dose or duration, there is a risk of developing resistance, said Dr. Sarah Kabbani, a public health physician at the Centers for Disease Control and Prevention.
Antibiotics work by killing bacteria in your body. But some bacteria will survive and thrive, which can make future infections more difficult to treat. This result, called antimicrobial resistance, is responsible for more than 35,000 deaths in the United States each year .
While antibiotics are necessary for serious, life-threatening infections, they’re sometimes prescribed for less urgent situations. Here’s how to tell if an antibiotic is right for you.
What to Consider
The most important question to discuss with your doctor before taking an antibiotic is: Do I really need it?
It’s very possible that you don’t, said Dr. Bradley Langford, a pharmacist specializing in antimicrobial resistance at Public Health Ontario in Toronto. According to the C.D.C., at least 28 percent of antibiotics prescribed in outpatient settings like doctors’ offices and emergency departments are unnecessary.
In recent years, U.S. health experts have recommended being more conservative in prescribing antibiotics for common situations, like for treating acne or preventing infections from dental procedures .
If a provider does recommend an antibiotic, research suggests that the shorter the course, the lower the resistance risk , and in many cases, shorter courses are just as effective as longer ones.
Still, some providers continue to prescribe longer courses than are necessary , Dr. Kabbani said, so whatever your situation, ask if you’re on the shortest course possible.
Also consider the type of antibiotic. Broad-spectrum antibiotics, which target many types of bacteria, are more likely to cause resistance than those that target fewer types.
And lower dosages don’t automatically mean less chance of resistance, Dr. Langford said. What’s more important is whether you’re taking antibiotics at all, and for how long.
Common Situations For Antibiotic Use
Most of us know that we shouldn’t take antibiotics for viral infections, like colds, coughs and flus. But guidelines for other situations may be less straightforward.
Surgical and Dental Procedures
Prophylactic antibiotics are often prescribed before surgeries to reduce the risk of infection. In those cases, antibiotics are worth taking, Dr. Kabbani said.
But taking antibiotics before a dental procedure is often not necessary , she said; the drugs should be reserved for those at higher risk of complications, according to the American Dental Association.
Recurrent Urinary Tract Infections
If you have chronic U.T.I.s, defined as more than two in six months or more than three in a year, short courses of prophylactic antibiotics — typically lasting from three months to a year — can reduce their recurrence in adults. But the drugs still carry risks for resistance and unwanted side effects (like rashes, diarrhea or yeast infections).
Doctors are increasingly recommending that if you have recurrent U.T.I.s, it’s best to start with alternative prevention methods, such as drinking more fluids , Dr. Langford said. Cranberry products, like juices or supplements, may help too. Or, if you regularly get U.T.I.s after sexual intercourse, you might take a single dose of an antibiotic just after intercourse.
There’s “very limited evidence” for taking prophylactic antibiotics for recurrent U.T.I.s indefinitely, Dr. Kabbani said. But if you are prescribed them for an extended course, make sure you know how long it should last; usually, it’s no more than a year, Dr. Langford said.
If your doctor detects bacteria in your urine but you don’t have symptoms, avoid antibiotics, research suggests, as they may increase your risk for developing symptomatic U.T.I.s in the future .
Skin Conditions
People with skin conditions like rosacea or acne are commonly prescribed antibiotics. In fact, dermatologists prescribe more antibiotics than providers in any other medical specialty , said Dr. John Barbieri, a dermatologist at Brigham and Women’s Hospital in Boston.
For severe rosacea, antibiotics are often the best treatment, Dr. Barbieri said. Though medicated creams or gels or gentle skin care routines can help with milder cases.
For acne, alternative and effective treatments are available, like benzoyl peroxide washes, topical retinoids and products with salicylic acid.
Topical antibiotics like clindamycin may help mild cases of acne, with fewer side effects than oral antibiotics, but they can still cause antimicrobial resistance . So take them in combination with other topical treatments, like benzoyl peroxide, experts say, to reduce your exposure.
If your acne is severe, oral antibiotics like doxycycline or sarecycline won’t “cure” it, but they can improve an outbreak quickly, Dr. Barbieri said, so they may be helpful for temporarily managing your acne while pursuing other, longer-term treatments.
If you can’t use an alternative treatment because of its side effects or because of another health condition, it’s “reasonable” to use oral antibiotics for longer periods, Dr. Barbieri said.
That decision will ultimately depend on your unique situation, Dr. Langford said, so it’s important to discuss every possible option with your provider. For some, “the benefit of antibiotics will outweigh the risk,” he added. But many people won’t need them at all.
Ask Well: Answers to Your Health Questions
Are Ingrown Hairs Preventable?: The dreaded bumps can occur anywhere you shave, wax or pluck. Here’s how to avoid them .
Do I Need That Antibiotic?: If it’s not medically necessary, you may want to consider the risk of antimicrobial resistance .
Why Are Feet So Stinky?: Experts say a mix of bacteria and sweat is likely to blame. But small changes can go a long way in reducing odors .
Why Is It So Hard to Shower When I’m Depressed?: Issues with hygiene are common symptoms of depression. Here’s why .
Why Don’t We Have Drugs to Stop Lyme Disease?: Anti-tick medications exist for dogs, but certain concerns have hindered their development for humans . That’s changing.
Do you have a question for our health and science editors? Ask us here .
Advertisement
‘We have nothing’: As Israel attacks Rafah, Palestinians live in tents, search for food

- Show more sharing options
- Copy Link URL Copied!
The tent camps stretch more than 10 miles along Gaza’s coast, filling the beach and spilling into empty lots, fields and streets. Families dig trenches to use as toilets. Fathers search for food and water. Children dig through garbage and wrecked buildings looking for wood or cardboard their mothers can burn for cooking.
Over the past three weeks, Israel’s offensive in Rafah has sent nearly a million Palestinians fleeing the city in the southern Gaza Strip and scattering across a wide area. Most have been displaced multiple times during Israel’s nearly eight-month-long war in Gaza, which is aimed at destroying Hamas but has devastated the territory and caused what the United Nations says is a near famine.
Monday night and Tuesday, Israeli shelling and airstrikes killed at least 37 people outside of Rafah, most of them sheltering in tents, pummeling the same area where strikes triggered a deadly fire days earlier in the camp for displaced Palestinians, according to witnesses, emergency workers and hospital officials.
The situation has been worsened by a dramatic plunge in the amount of food, fuel and other supplies reaching the U.N. and other aid groups to distribute to the population. Palestinians have largely been on their own to resettle and find the basics for survival.

World & Nation
Israeli army says it used small munitions in Rafah airstrike, and fire was caused by secondary blast
The Israeli military says an initial investigation into a strike that sparked a deadly weekend fire in Rafah has found the blaze was caused by a secondary explosion.
May 28, 2024
“The situation is tragic. You have 20 people in the tent, with no clean water, no electricity. We have nothing,” said Mohammad Abu Radwan, a schoolteacher. He shares a tent with his wife, six children and other family members.
“I can’t explain what it feels like living through constant displacement, losing your loved ones,” he said. “All of this destroys us mentally.”
Abu Radwan fled Rafah soon after the Israeli assault on the city began May 6 as bombardment neared the house where he was sheltering. He and three other families paid $1,000 for donkey carts to take them to the outskirts of Khan Yunis, less than 4 miles away, where it took a day living outdoors before they could assemble the materials for a makeshift tent. Next to the tent, they dug a toilet trench, hanging blankets and old clothes around it for privacy.
Families usually have to buy the wood and tarps for their tents, which can run up to $500, not counting ropes, nails and the cost of transporting the material, the humanitarian group Mercy Corps said.
Israeli authorities controlling all entry points into Gaza have been letting greater numbers of private commercial trucks into the territory, the U.N. and aid workers say. More fruits and vegetables can be found in markets, and prices on some have fallen, Palestinians say.

In Gaza, she sits by her belongings, waiting for her home to be bombed
‘I just don’t know where we’ll go.’ It’s a question Palestinians ask over and over in Gaza as Israel ramps up bombardment after Hamas truce collapsed.
Dec. 4, 2023
Still, most homeless Palestinians can’t afford them. Many in Gaza have not received salaries for months, and their savings are being depleted. Even those who have money in the bank often can’t withdraw it because there is so little cash in the territory. Many turn to black-market exchanges that charge up to 20% to give cash for transfers from bank accounts.
Meanwhile, humanitarian convoys with supplies for aid groups to distribute have fallen to nearly the lowest levels of the war, the U.N. says.
Previously, the U.N. was receiving several hundred trucks a day. Since May 6, the daily number has dropped to an average of 53, according to the U.N. Office for the Coordination of Humanitarian Affairs, or OCHA. Some 600 trucks a day are needed to stave off starvation, according to the U.S. Agency for International Development.
In the past three weeks, most of the incoming aid has entered through two crossings from Israel in northern Gaza and via a U.S.-built floating pier taking deliveries by sea. But that pier has suspended operations after damage from rough seas, three U.S. officials told the Associated Press on Tuesday.
The main crossings in the south, Rafah from Egypt and Kerem Shalom from Israel, are either not operating or are largely inaccessible to aid groups because of fighting. Israel says it has been letting hundreds of trucks through Kerem Shalom. But the U.N. has been able to collect only about 200 on the Gaza side over the past three weeks because of Israeli military restrictions, the expanding offensive, Israeli airstrikes and Hamas rocket launches, spokesperson Juliette Touma said Tuesday.

Grief and anger as workers with José Andrés aid kitchen killed in Israeli airstrikes in Gaza
Staffers from World Central Kitchen, chef José Andrés’ humanitarian aid group trying to get food to Palestinians in Gaza, were killed in Israeli airstrikes.
April 2, 2024
Entry of fuel has fallen to about a third of what it was before the Rafah offensive, according to OCHA. That amount has to keep hospitals, bakeries, water pumps and aid trucks working.
The U.S. humanitarian group American Near East Refugee Aid “is having difficulty distributing what we are able to bring in to the people who need it, because there’s so little fuel for trucks,” spokesperson Steve Fake said.
Most of those fleeing Rafah have poured into a humanitarian zone declared by Israel that is centered on Muwasi, a largely barren strip of coastal land. The zone was expanded north and east to reach the edges of Khan Yunis and the central town of Deir al Balah, both of which have also filled with people.
“As we can see, there is nothing ‘humanitarian’ about these areas,” said Suze van Meegen, head of operations in Gaza for the Norwegian Refugee Council, which has staff operating in Muwasi.
Much of the humanitarian zone has no charity kitchens or food market; it has only a few field hospitals and smaller medical tents that can’t handle emergencies but pass out painkillers and antibiotics if they have them, according to Mercy Corps. “It’s just a matter of time before people begin to suffer greatly from food insecurity,” the group said.

U.N. halts all food distribution in Rafah after running out of supplies in the southern Gaza city
The United Nations says it has suspended food distribution in the southern Gaza city of Rafah due to lack of supplies and insecurity.
May 21, 2024
The Muwasi area is mostly coastal dunes, with no water resources or sewage systems. With human waste deposited near the tents and garbage piling up, many people are suffering from diarrhea and diseases such as hepatitis, as well as skin allergies and lice, Mercy Corps said.
One aid worker who fled Rafah said he was lucky he could afford to rent a house in Deir al Balah. “You can’t walk” in the town from all the tents that have arisen, said the man, who was not authorized to speak to the press. Many people he sees in the street are yellow with jaundice, and “the stench is disgusting” from the sewage and garbage.
Israel says its offensive in Rafah is vital to its aim of destroying Hamas in Gaza after the group’s Oct. 7 attack, in which militants killed some 1,200 people and abducted around 250. Israel’s retaliatory campaign in Gaza has killed some 36,000, according to the Health Ministry there.
Aid groups have warned for months that an attack on Rafah would worsen Gaza’s humanitarian disaster. So far, Israel’s operations have been short of an all-out invasion, though fighting has expanded over the past three weeks from the eastern parts of Rafah to the central districts. A strike Sunday hit a tent camp in a western part of Rafah, causing a large fire and killing at least 45 people, according to health officials. Israeli Prime Minister Benjamin Netanyahu acknowledged that a “tragic mistake” had occurred.

Netanyahu acknowledges ‘tragic mistake’ after Rafah strike kills dozens of Palestinians
Israel faces new condemnation over strikes on the southern Gaza city of Rafah that local health officials say killed at least 45 Palestinians.
May 27, 2024
Satellite photos shot Friday by Planet Labs PBC show dense new tent camps running the length of the coast from just north of Rafah to Deir al Balah. The ramshackle shelters are densely packed in mazes of corrugated metal and plastic sheets, blankets and bedsheets draped over wooden sticks for privacy.
Tamer Saeed Abu’l Kheir said he goes out every day at 6 a.m. to find water, usually returning around noon to the tent outside Khan Yunis where he and nearly two dozen relatives live. His three children, all under 10, are always sick, but he has to send them out to collect wood for the cooking fire, he says. He worries they’ll come across unexploded bombs in the wrecked houses.
His aging father has trouble moving so has to relieve himself in a bucket, and Abu’l Kheir has to regularly pay to transport him to the nearest hospital for kidney dialysis.
“Wood costs money, water costs money, everything costs money,” said his wife, Leena Abu’l Kheir. She broke down in sobs. “I’m afraid I’ll wake up one day and I’ve lost my children, my mother, my husband, my family.”
Shurafa, Magdy and Keath write for the Associated Press. Magdy and Keath reported from Cairo. AP correspondents Sarah El Deeb in Beirut, Fatma Khaled in Cairo and Mohammed Jahjouh in Muwasi, Gaza Strip, contributed to this report.
More to Read

Israeli airstrike kills at least 22 people in Rafah, Palestinian medics say
May 26, 2024

Palestinians mark 76 years of dispossession as new catastrophe unfolds in Gaza
May 14, 2024

Misery deepens in Gaza’s Rafah as Israeli troops press operation
May 13, 2024
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.
More From the Los Angeles Times

Spain, Norway and Ireland formally recognize a Palestinian state as EU rift with Israel widens

Kaffiyehs and pickets: UCLA, UC Davis workers strike over treatment at pro-Palestinian protests

Norway hands over papers in diplomatic step recognizing a Palestinian state

Opinion: The issue of human rights is on life support. Here’s how to save it
- Skip to content
- Accessibility help
Diarrhoea - antibiotic associated
Last revised in June 2023
Diarrhoea is a common consequence of treatment with antibiotics, occurring in 225% of people taking antibiotics
- Investigations
- Scenario: Diarrhoea - antibiotic associated
Prescribing information
- Fidaxomicin
Background information
- Risk factors
- Complications
Diarrhoea - antibiotic associated: Summary
- Diarrhoea is a common consequence of treatment with antibiotics, occurring in 2–25% of people taking antibiotics, depending on the antibiotic prescribed.
- Around 20% to 30% of cases of antibiotic-associated diarrhoea are due to Clostridioides difficile . Antibiotics frequently associated with C. difficile infection (CDI) include clindamycin, cephalosporins (especially third and fourth-generation), fluoroquinolones, and broad-spectrum penicillins.
- Factors that increase the risk of CDI include increased age, frailty, previous history of CDI, exposure to other cases, concomitant use of a proton pump inhibitor or other acid-suppressing drugs, and underlying co-morbidity (such as abdominal surgery, chronic renal disease, inflammatory bowel disease, and immunosuppression).
- The complications of CDI can be severe and include pseudomembranous colitis, toxic megacolon, perforation of the colon, sepsis, and death.
- The severity of symptoms should be assessed and the need for hospital admission considered.
- If C. difficile is suspected, assess whether this is a first or further episode (relapse or recurrence).
- If infection with C. difficile is suspected, a stool sample should be taken.
- The antibiotic should be stopped, if this is appropriate.
- Fluid loss and symptoms should be managed as for acute gastroenteritis.
- Suspected and non-severe infection is managed with antibiotics after advice from a microbiologist or infectious diseases specialist.
- Risk of a C. difficile outbreak should be assessed — for example, among other elderly residents in a care or nursing home.
- Any antibiotics not being used to treat CDI should be stopped, if appropriate.
- Fluid loss and symptoms should be managed.
- Antimotility drugs (such as loperamide) should be avoided.
- Advice should be given on hygiene measures to minimize the spread of C. difficile .
- Diarrhoea due to C. difficile infection should resolve in 1–2 weeks. The person will remain infectious whilst they still have symptoms, and they should stay away from work or school until they have been free from diarrhoea for 48 hours.
- Severe and fulminant CDI should be managed in hospital and referral should be considered in individuals at high risk of complications or recurrence, or if they have a recurrent infection after experiencing two previous CDI episodes.
The content on the NICE Clinical Knowledge Summaries site (CKS) is the copyright of Clarity Informatics Limited (trading as Agilio Software Primary Care) . By using CKS, you agree to the licence set out in the CKS End User Licence Agreement .

IMAGES
VIDEO
COMMENTS
Antibiotic prophylaxis or 'stand-by' antibiotic treatment can be considered for certain high-risk travellers. Specialist advice should be sought. Advice should be offered about managing diarrhoea while travelling, including the following: Most episodes are short-lived and self-limiting, lasting a few days.
The recommendations on managing people at low or intermediate risk of travellers' diarrhoea are largely based on expert opinion regarding general advice to offer travellers in a World Health Organisation (WHO) publication International Travel and Health [], the American College of Gastroenterologists guideline Diagnosis, Treatment, and Prevention of Acute Diarrheal Infections in Adults [Riddle ...
Treatment. Travelers' diarrhea (TD) is the most predictable travel-related illness. Attack rates range from 30%-70% of travelers during a 2-week period, depending on the destination and season of travel. Traditionally, TD was thought to be prevented by following simple dietary recommendations (e.g., "boil it, cook it, peel it, or forget ...
The recommendation on suspected travellers' diarrhoea is based on the expert consensus publication on travellers' diarrhoea, which found moderate-quality evidence that antibiotic treatment is not recommended in people with mild symptoms, and moderate-to-high quality evidence that antibiotics should be used to treat moderate-to-severe symptoms ...
Episodes of travelers' diarrhea are nearly always benign and self-limited, but symptoms may disrupt planned activities and result in health care visits for some travelers . There is a growing recognition that travelers' diarrhea and its self-treatment abroad are associated with the acquisition of organisms harboring antibiotic resistance [ 5-10 ].
If you do get traveler's diarrhea, avoid caffeine, alcohol and dairy products, which may worsen symptoms or increase fluid loss. But keep drinking fluids. Drink canned fruit juices, weak tea, clear soup, decaffeinated soda or sports drinks to replace lost fluids and minerals. Later, as your diarrhea improves, try a diet of easy-to-eat complex ...
Travelers' diarrhea (TD) is the most common travel-related illness, affecting up to 70% of travelers to certain destinations. 1 Its etiology is predominantly bacterial, ... (1 or more of fever, moderate to severe abdominal pain or bloody diarrhea), then antibiotics should be used (Table 2). To ensure ready access to antibiotic treatment if ...
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant. When you visit a place where the climate or sanitary practices are ...
Travellers' diarrhoea is one of the most common illnesses in people who travel internationally, and depending on destination affects 20-60% of the more than 800 million travellers each year. In most cases the diarrhoea occurs in people who travel to areas with poor food and water hygiene.1 This review examines the approach to the prevention and treatment of diarrhoea in travellers. Much of ...
What you need to know. Enterotoxic Escherichia coli (ETEC) is the most common cause of acute travellers' diarrhoea globally. Chronic (>14 days) diarrhoea is less likely to be caused by bacterial pathogens. Prophylactic antibiotic use is only recommended for patients vulnerable to severe sequelae after a short period of diarrhoea, such as those with ileostomies or immune suppression
Traveler's diarrhea affects travelers and others who consume contaminated food or water. It's a brief but unpleasant gastrointestinal infection that typically causes loose stools and abdominal cramps. Most of the time, it's caused by bacteria, but sometimes viruses or parasites are to blame. International travelers are most at risk when ...
Traveller's diarrhoea is a common problem among travellers to destinations with deficiencies in water, sanitation, and hygiene (WASH) infrastructure, typically caused by the consumption of contaminated food or water. ... and possibly, antibiotics. Antibiotic therapy is generally reserved for moderate to severe infections. In healthy patients ...
Traveller's diarrhoea. Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. It is caused by consuming food and water, contaminated by germs (microbes) including bacteria, viruses and parasites. Other symptoms can include high temperature (fever), being sick (vomiting) and tummy (abdominal) pain.
For more information, see the CKS topic on Diarrhoea - antibiotic associated. Diarrhoea occurs after foreign travel — also request tests for ova, cysts, and parasites and state the countries visited on the form. Amoebae, Giardia, or cryptosporidium are suspected, particularly if diarrhoea is persistent (2 weeks or more) or the person has ...
In 50-80% of TD cases, TD is caused by bacterial infection. Mild diarrhoea can be managed with an antimotility agent (loperamide) alone, but for moderate or severe diarrhoea, early self-treatment with loperamide in conjunction with antibiotics is advised. Recommended empirical antibiotics are fluoroquinolones (norfloxacin / ciprofloxacin) or ...
Traveller's diarrhoea (TD) is defined as "the occurrence of three or more unformed stools in a 24 hour period during or after a journey associate with at least one of the following symptoms: fever, nausea, vomiting, abdominal cramps, tenesmus, or bloody stools" (1). Generally, symptoms begin six or seven days after arrival and often resolve ...
If you have any injuries, scratches, or bug bites. Health care or medications you received during your trip. Close contact with other people, including sexual encounters. If you got any tattoos or piercings. If your healthcare provider has trouble determining why you are feeling sick, you may want to ask to speak with an infectious disease ...
Some of the most common causes of loose stools are infections, medication side effects, and travelers' diarrhea. Chronic conditions like Crohn's disease, ulcerative colitis UC), irritable bowel ...
Thomas Volkman, Vanessa Clifford, Georgia A. Paxton. September-October 2020. Article 101680. View PDF. Article preview. In an increasingly mobile world, more children than ever before, from newborn babies to adolescents, travel and cross borders. Apart from children that travel for pleasure or to visit family, the pre- and post-travel care of ...
Side effects can include rash, dizziness, nausea, diarrhea and yeast infections. More serious side effects can include antimicrobial-resistant infections or C. diff infection, which causes diarrhea that can lead to severe colon damage and death. Call your healthcare provider if you develop any side effects while taking your antibiotic.
Travellers' diarrhea. Travellers' diarrhea is the most common illness affecting travellers. It is spread from eating or drinking contaminated food or water. Risk of developing travellers' diarrhea increases when travelling in regions with poor standards of hygiene and sanitation. Practise safe food and water precautions.
Topical antibiotics like clindamycin may help mild cases of acne, with fewer side effects than oral antibiotics, but they can still cause antimicrobial resistance. So take them in combination with ...
Last revised in September 2023. Scenario: Diarrhoea - prevention and advice for travellers: Covers the prevention of travellers' diarrhoea, and advice for people who are at risk of travellers' diarrhoea. The content on the NICE Clinical Knowledge Summaries site (CKS) is the copyright of Clarity Informatics Limited (trading as Agilio Software ...
The tent camps stretch more than 10 miles along Gaza's coast, filling the beach and spilling into empty lots, fields and streets. Families dig trenches to use as toilets. Fathers search for food ...
Diarrhoea is a common consequence of treatment with antibiotics, occurring in 2-25% of people taking antibiotics, depending on the antibiotic prescribed. Around 20% to 30% of cases of antibiotic-associated diarrhoea are due to Clostridioides difficile. Antibiotics frequently associated with C. difficile infection (CDI) include clindamycin ...
Book Godzillas Hostel Now. Godzilla's Hostel is the first proper hostel opened in Moscow. One of its main advantages is that it has both dorms and doubles, so you can get a nice hotel room for the price of a hostel. The vibe at the hostel is pretty friendly: they have a common area and a kitchen, so it's a good spot to meet fellow travelers.