Ectopic Supraventricular Arrhythmias
Various rhythms result from supraventricular foci (usually in the atria). Diagnosis is by electrocardiography. Many are asymptomatic and require no treatment.
(See also Overview of Arrhythmias .)
Ectopic supraventricular rhythms include
Atrial premature beats
Atrial tachycardia, multifocal atrial tachycardia, nonparoxysmal junctional tachycardia, wandering atrial pacemaker.
Atrial premature beats (APB), or premature atrial contractions (PAC), are common episodic impulses. They may occur in normal hearts with or without precipitating factors (eg, coffee, tea, alcohol, pseudoephedrine ) or may be a sign of a cardiopulmonary disorder. They are common in patients with chronic obstructive pulmonary disease (COPD). They occasionally cause palpitations.
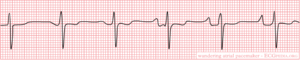
Diagnosis is by electrocardiography (ECG—see figure Atrial premature beat ).
Atrial premature beat (APB)
Image courtesy of L. Brent Mitchell, MD.
APBs may be normally, aberrantly, or not conducted and are usually followed by a noncompensatory pause. Aberrantly conducted APBs (usually with right bundle branch block morphology) must be distinguished from premature beats of ventricular origin.
Atrial escape beats are ectopic atrial beats that emerge after long sinus pauses or sinus arrest. They may be single or multiple; escape beats from a single focus may produce a continuous rhythm (called ectopic atrial rhythm). Heart rate is typically slower, P wave morphology is typically different, and PR interval is slightly shorter than in sinus rhythm.
Atrial tachycardia is a regular rhythm caused by the consistent, rapid atrial activation from a single atrial focus. Heart rate is usually 150 to 200 beats/minute; however, with a very rapid atrial rate, nodal dysfunction, and/or digitalis toxicity, atrioventricular (AV) block may be present, and ventricular rate may be slower. Mechanisms include enhanced atrial automaticity and intra-atrial reentry.
Atrial tachycardia is the least common form (5%) of paroxysmal supraventricular tachycardia and usually occurs in patients with a structural heart disorder. Other causes include atrial irritation (eg, pericarditis
Symptoms are those of other tachycardias (eg, light-headedness, dizziness, palpitations, and rarely syncope).
Diagnosis is by electrocardiography (ECG); P waves, which differ in morphology from normal sinus P waves, precede QRS complexes but may be hidden within the preceding T wave (see figure True atrial tachycardia ).
True atrial tachycardia
Vagal maneuvers may be used to slow the heart rate, allowing visualization of P waves when they are hidden, but these maneuvers do not usually terminate the arrhythmia (demonstrating that the AV node is not an obligate part of the arrhythmia circuit).
Treatment involves managing causes and slowing ventricular response rate using a beta-blocker or calcium channel blocker. An episode may be terminated by direct current cardioversion . Pharmacologic approaches to termination and prevention of atrial tachycardia include antiarrhythmic drugs in class Ia, Ic, or III. If these noninvasive measures are ineffective, alternatives include overdrive pacing and ablation .
Multifocal atrial tachycardia (chaotic atrial tachycardia) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is > 100 beats/minute. On ECG, P-wave morphology differs from beat to beat, and there are ≥ 3 distinct P-wave morphologies. The presence of P waves distinguishes multifocal atrial tachycardia from atrial fibrillation . Except for the rate, features are the same as those of wandering atrial pacemaker. Symptoms, when they occur, are those of rapid tachycardia. Multifocal atrial tachycardia can be due to an underlying pulmonary disorder such as chronic obstructive pulmonary disease coronary artery disease , and electrolyte abnormalities such as hypokalemia . Treatment is directed at the underlying disorder.
Nonparoxysmal junctional tachycardia is caused by abnormal automaticity in the AV node or adjacent tissue, which typically follows open heart surgery, acute inferior myocardial infarction, myocarditis, or digitalis toxicity. Heart rate is 60 to 120 beats/minute; thus, symptoms are usually absent. ECG shows regular, normal-appearing QRS complexes without identifiable P waves or with retrograde P waves (inverted in the inferior leads) that occur shortly before ( < 0.1 second) or after the QRS complex. The rhythm is distinguished from paroxysmal supraventricular tachycardia by the lower heart rate and gradual onset and offset. Treatment is directed at causes.
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Wandering Atrial Pacemaker EKG Interpretation with Rhythm Strip
Ekg features, wandering atrial pacemaker ekg interpretation example.
This website is only for professional medical education. Contact your doctor for medical care. 2024 © MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Wandering Atrial Pacemaker
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Key features, clinical presentation, diagnostic evaluation, ongoing management.
- Full Chapter
- Supplementary Content
ESSENTIALS OF DIAGNOSIS
Progressive cyclic variation in P-wave morphology
Heart rate 60–100 bpm
Variation of P-wave morphology, P-P interval, and P-R interval
GENERAL CONSIDERATIONS
This rhythm is benign
This rhythm and multifocal atrial tachycardia are similar except for heart rate
The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity
Usually, it is associated with underlying lung disease
In the elderly, it may be a manifestation of sick sinus syndrome
In the young and athletic heart, it may represent enhanced vagal tone
SYMPTOMS AND SIGNS
Usually causes no symptoms and is incidentally discovered
Occasional patient may feel skipped beats
PHYSICAL EXAM FINDINGS
Variable S 1
DIFFERENTIAL DIAGNOSIS
Multifocal atrial tachycardia (heart rate > 100 bpm)
Frequent premature atrial complexes and atrial bigeminy
LABORATORY TESTS
None specific
ELECTROCARDIOGRAPHY
ECG to document rhythm
CARDIOLOGY REFERRAL
Not required
MEDICATIONS
No specific treatment
Monitor and treat the underlying cause, such as sick sinus syndrome or lung disease
DIET AND ACTIVITY
No restrictions
General healthy lifestyle
Once a year if sinus node abnormality is suspected; otherwise when symptoms arise
COMPLICATIONS
May progress to sick sinus syndrome
This condition by itself is benign
PRACTICE GUIDELINES
Indications for pacemaker:
– If part of sick sinus syndrome
– If associated with documented symptomatic bradycardia
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- Mobile Apps
- Journal Club
- Antibiotics
- Quick Critical Care
- Residency Directory
- Recent Changes
- About WikEM
- Getting Started
- Creating & Editing
- Needed Pages
- Editorial Levels
- Contribution Score
- Elective Guide
- Citing WikEM
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Browse properties

- View source
- View history
- Create account

We need you! See something you could improve? Make an edit and help make WikEM better for everyone.
- Wandering atrial pacemaker
- 2 Clinical Features
- 3.1 Palpitations
- 4.2 Diagnosis
- 5 Management
- 6 Disposition
- 8 External Links
- 9 References
- Three or more ectopic foci within the atrial myocardium serve as the pacemaker
- Rate is less than 100bpm (in contrast to MAT )
- Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia
- Intrinsic cardiac or pulmonary disease
- Metabolic derangements
- Drug toxicity (including Digoxin )
Clinical Features
- Often seen in the extremes of age and in athletes
- Rarely causes symptoms
Differential Diagnosis
Palpitations.
- Narrow-complex tachycardias
- Wide-complex tachycardias
- Second Degree AV Block Type I (Wenckeback)
- Second Degree AV Block Type II
- Third Degree AV Block
- Premature atrial contraction
- Premature junctional contraction
- Premature ventricular contraction
- Sick sinus syndrome
- Acute coronary syndrome
- Cardiomyopathy
- Congenital heart disease
- Congestive heart failure (CHF)
- Mitral valve prolapse
- Pacemaker complication
- Pericarditis
- Myocarditis
- Valvular disease
- Panic attack
- Somatic Symptom Disorder
- Drugs of abuse (e.g. cocaine )
- Medications (e.g. digoxin , theophylline )
- Thyroid storm
- Pulmonary embolism
- Dehydration
- Pheochromocytoma

- ECG should show three distinct P wave morphologies with a ventricular rate <100bpm
- Rarely requires treatment
Disposition
- Outpatient management
- Multifocal atrial tachycardia
- Dysrhythmia
External Links
- Richard Cunningham
- fardis tavangary
- Ross Donaldson
- Privacy policy
- Disclaimers

Multifocal Atrial Tachycardia (MAT)
- Ed Burns and Robert Buttner
- Jun 4, 2021
Multifocal Atrial Tachycardia (MAT) Overview
- A rapid, irregular atrial rhythm arising from multiple ectopic foci within the atria.
- Most commonly seen in patients with severe COPD or congestive heart failure.
- It is typically a transitional rhythm between frequent premature atrial complexes (PACs) and atrial flutter / fibrillation.
AKA “Chaotic atrial tachycardia”
Electrocardiographic Features
- Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm).
- Irregularly irregular rhythm with varying PP, PR and RR intervals.
- At least 3 distinct P-wave morphologies in the same lead.
- Isoelectric baseline between P-waves (i.e. no flutter waves).
- Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent PACs).
- Some P waves may be nonconducted; others may be aberrantly conducted to the ventricles.
There may be additional electrocardiographic features suggestive of COPD.
Clinical Relevance
- Usually occurs in seriously ill elderly patients with respiratory failure (e.g. exacerbation of COPD / CHF).
- Tends to resolve following treatment of the underlying disorder.
- The development of MAT during an acute illness is a poor prognostic sign, associated with a 60% in-hospital mortality and mean survival of just over a year. Death occurs due to the underlying illness; not the arrhythmia itself.
Arises due to a combination of factors that are present in hospitalised patients with acute-on-chronic respiratory failure:
- Right atrial dilatation (from cor pulmonale )
- Increased sympathetic drive
- Hypoxia and hypercarbia
- Beta-agonists
- Theophylline
- Electrolyte abnormalities: Hypokalaemia and hypomagnesaemia (e.g. secondary to diuretics / beta-agonists)
The net result is increased atrial automaticity.
ECG Examples
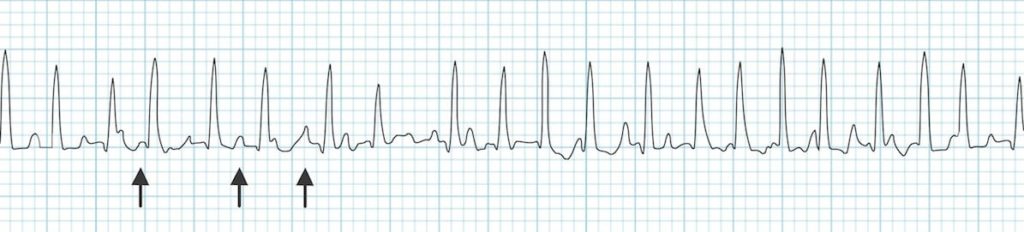
Multifocal atrial tachycardia:
- Rapid irregular rhythm > 100 bpm.
- At least 3 distinctive P-wave morphologies (arrows).
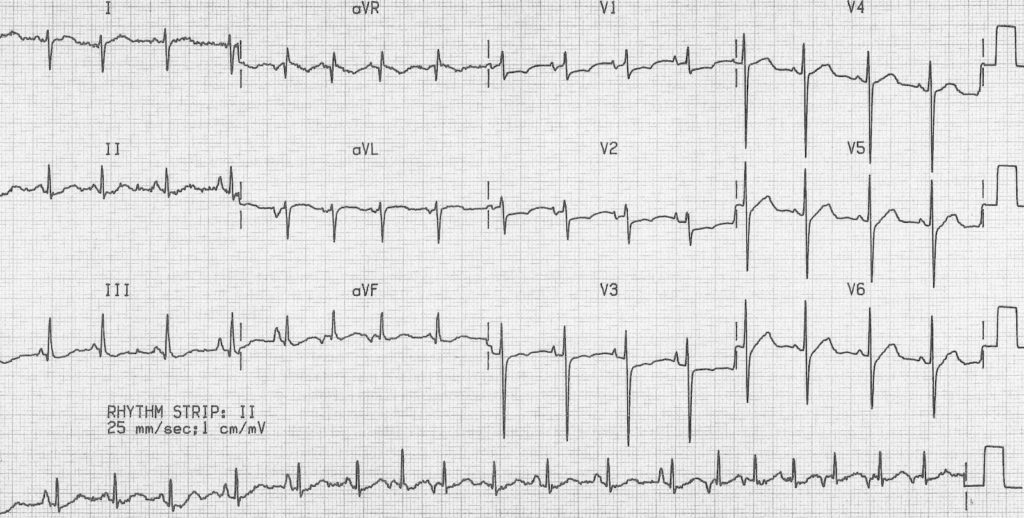
MAT with additional features of COPD :
- Rapid, irregular rhythm with multiple P-wave morphologies (best seen in the rhythm strip).
- Right axis deviation, dominant R wave in V1 and deep S wave in V6 suggest right ventricular hypertrophy due to cor pulmonale.
Related Topics
- The ECG in COPD
- Right atrial enlargement (P pulmonale)
- Right ventricular hypertrophy
Advanced Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course : Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop . Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog .
- Zimmerman FH. ECG Core Curriculum . 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations , 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine . 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care . 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG . 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Robert Buttner
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library . Twitter: @rob_buttner
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
Atrial Rhythms Module
Atrial dysrhythmias.
Thomas E. O'Brien AS CCT CRAT RMA
Learning Objectives
At the conclusion of this training module the reader will be able to:
- Recall and apply the 5-steps of heart rhythm interpretation
- Recognize the difference between regular and irregular rhythms
- Recall the normal range for PR interval and QRS complex
- Recognize the features and qualifying criteria for the following complexes and rhythms:
- Premature Atrial Complexes
- Wandering Atrial Pacemaker Rhythm
Multifocal Atrial Tachycardia
- Atrial Flutter
- Atrial Fibrillation
Authors and Reviewers
- EKG heart rhythm modules: Thomas O'Brien
- Medical review: Dr. Jonathan Keroes, MD
- Medical review: Dr. Pedro Azevedo, MD, Cardiology
- Last Update: 11/8/2021
- Electrocardiography for Healthcare Professionals, 6th Edition Kathryn Booth and Thomas O'Brien ISBN10: 1265013470, ISBN13: 9781265013479 McGraw Hill, 2023
- Rapid Interpretation of EKG's, Sixth Edition Dale Dublin Cover Publishing Company
- EKG Reference Guide EKG.Academy
- 12 Lead EKG for Nurses: Simple Steps to Interpret Rhythms, Arrhythmias, Blocks, Hypertrophy, Infarcts, & Cardiac Drugs Aaron Reed Create Space Independent Publishing
- The Virtual Cardiac Patient: A Multimedia Guide to Heart Sounds, Murmurs, EKG Jonathan Keroes, David Lieberman Publisher: Lippincott Williams & Wilkin) ISBN-10: 0781784425; ISBN-13: 978-0781784429
- ECG Reference Guide PracticalClinicalSkills.com
Lesson #1: Rhythm Analysis Method 312
The five steps of rhythm analysis will be followed when analyzing any rhythm strip.
- Analyze each step in the following order.
Rhythm Regularity
- P wave morphology
- P R interval or PRi
- QRS complex duration and morphology
- Carefully measure from the tip of one R wave to the next, from the beginning to the end of the tracing.
- A rhythm is considered “regular or constant” when the distance apart is either the same or varies by 1 ½ small boxes or less from one R wave to the next R wave.
Heart Rate Regular (Constant) Rhythms
- The heart rate determination technique used will be the 1500 technique.
- Starting at the beginning of the tracing through the end, measure from one R wave to the next R wave (ventricular assessment), then P wave to P wave (atrial assessment), then count the number of small boxes between each and divide that number into 1500. This technique will give you the most accurate heart rate when analyzing regular heart rhythms. You may include ½ of a small box i.e. 1500/37.5 = 40 bpm (don’t forget to round up or down if a portion of a beat is included in the answer).
Step 2 (Cont)
Heart rate - irregular rhythms.
- If the rhythm varies by two small boxes or more, the rhythm is considered “irregular”.
- The heart rate determination technique used for irregular rhythms will be the “six-second technique”.
- Simply count the number of cardiac complexes in six seconds and multiply by ten.
P wave Morphology (shape)
- Lead II is most commonly referenced in cardiac monitoring
- In this training module, lead two will specifically be referenced unless otherwise specified.
- The P wave in lead II in a normal heart is typically rounded and upright in appearance.
- Changes in shape must be reported. This can be an indicator that the locus of stimulation is changing or the pathway taken is changing.
- P waves may come in a variety of morphologies i.e. rounded and upright, peaked, flattened, notched, biphasic(pictured), inverted and even buried or absent!
- Remember to describe the shape. This can be very important to the physician when diagnosing the patient.
PR interval (PRi)
- Measurement of the PR interval reflects the amount of time from the beginning of atrial depolarization to the beginning of ventricular depolarization.
- Plainly stated, this measurement is from the beginning of the P wave to the beginning of the QRS complex.
- The normal range for PR interval is: 0.12 – 0.20 seconds (3 to 5 small boxes)
- It is important that you measure each PR interval on the rhythm strip.
- Some tracings do not have the same PRi measurement from one cardiac complex to the next. Sometimes there is a prolonging pattern, sometimes not.
- If the PR intervals are variable, report them as variable, but note if a pattern is present or not.
QRS complex
- QRS represents ventricular depolarization.
- It is very important to analyze each QRS complex on the tracing and report the duration measurement and describe the shape (including any changes in shape).
- As discussed in step 3, when referring to P waves, remember changes in the shape of the waveform can indicate the locus of stimulation has changed or a different conduction pathway was followed. It is no different when analyzing the QRS complex. The difference is that in step 3, we were looking at atrial activity. Now we are looking at ventricular activity.
- Measure from the beginning to the end of ventricular depolarization.
- The normal duration of the QRS complex is: 0.06 – 0.10 second
Lesson #2: Interpretation 312
Introduction.
- The previous slides presented the five-steps of rhythm analysis. These five steps must be followed regardless of how simple of complex the tracing is you are reviewing.
- The information gathered in these steps are telling a story.
- The title of that story is the interpretation.
Atrial Dysrhythmias Types
The dysrhythmias in this category occur as a result of problems in the atria. These atrial dysrhythmias primarily affect the P wave. We will be discussing the following complexes and rhythms:
- Premature Atrial Complexes (PAC’s)
- Wandering Atrial Pacemaker
Lesson #3: Premature Atrial Complex
Intro to pacs.
- PACs can occur for a number of different reasons i.e., diet, fatigue, stress, disease, ischemia to name a few.
- Premature complexes frequently occur in bradycardic rhythms, but may occur almost any time.
- PACs occur when an early electrical impulse occurs from a location in the atria other than the SA node.
Intro to PACs 2
- This early impulse causes an early cardiac complex which disrupts the underlying rhythm.
- The locus of stimulation being different, results in a change in the morphology of the P wave.
- PACs can occur occasionally or frequently.
- PACs ECG can be observed with or without a pattern
- The P wave with PAC's will always be upright
EKG Analysis
Notice the following: the R to R interval is irregular, the fifth complex is early and the P wave on the early complex is a different shape.
EKG Practice Strip
Analyze this tracing using the five steps of rhythm analysis.
- Rhythm: Irregular
- P wave: Upright & uniform (except early complexes - biphasic)
- PR interval: 0.16 second
- Interpretation: Sinus Bradycardia with PACs
Lesson #4: Wandering Atrial Pacemaker
Description.
- Rhythms are often named according to the origin of the electrical activity in the heart or the structure where the problem is occurring.
- Wandering Atrial Pacemaker is aptly named due to the electrical impulses causing the atrial activity are moving or wandering.
- These changes in the locus of stimulation affect the morphology of the P waves.
- In Wandering Atrial Pacemaker ECG, you must observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular.
- The PR interval is often affected, but does not have to be.
- The bottom line, is you must observe at least three different shaped P waves.
Practice Strip
- P wave: Changing Shapes (3 or more)
- PR interval: Variable
- Interpretation: Wandering Atrial Pacemaker
Lesson #5: Multifocal Atrial Tachycardia
- Multifocal Atrial Tachycardia is just a faster version of Wandering Atrial Pacemaker. The criteria is the same as Wandering Atrial Pacemaker with the only difference being the heart rate exceeds 100 bpm.
- These changes in the locus of stimulation within the atria affect the morphology of the P waves.
- Remember, you must observe at least three different shaped P waves.
- Due to the presence of irregular R to R intervals coupled with the changing P wave morphology, some people have confused this rhythm with Atrial Fibrillation.
Lesson #6: Atrial Flutter
- Atrial Flutter (sometimes called a flutter) occurs when there is an obstruction within the atrial electrical conduction system.
- Due to this impediment a series of rapid depolarizations occur.
- These depolarizations may occur two, three, four or more times per QRS complex.
- The AV node functions like a “gatekeeper” blocking the extra impulses until the ventricular conduction system is able to accept the impulse.
- The impulse that is accepted will cause the QRS complex to occur.
- Each atrial flutter ECG wave represents atrial depolarization. This will be noted next to the P wave step in rhythm analysis. Instead of P waves, this tracing has “F” waves. No P waves mean there is no PR interval measurement.
- When the tracing is interpreted, the ratio of F waves to each QRS complex will be documented along with the rhythm i.e. Atrial Flutter 4:1 (indicates 4 “F” waves to each QRS complex). Not all Atrial Flutter rhythm strips will have a regular rhythm. In that case just document and report your observations.
- Compare your answers with the answers on the next slide.
Practice Strip Answers
- Rhythm: Regular
- Rate: Ventricles - 80, Atria - 320
- P wave: "F" waves
- PR interval: absent
- Interpretation: Atrial Flutter 4:1
Lesson #7: Atrial Fibrillation
- Atrial Fibrillation (afeb) occurs when multiple electrical impulses occur within the atria. This chaotic electrical activity results in a chaotic wave form between the QRS complexes. P waves are absent. They are replaced by lower case "f" waves. No P waves means there is no PR interval measurement.
- This rapid electrical activity overwhelms the AV node causing impulses to enter the ventricular conduction system at irregular points. This results in irregular R to R intervals.
- Not all fibrillatory waves are created equal. The "f" waves can be coarse (majority measure 3 mm or more) or can be fine (majority of waveforms measure less than 3 mm) to almost absent. Regardless always report your observations. Many times when a patient has "new onset" Atrial Fibrillation the patient will report with a heart rate of 160 bpm or more.
- When a patient experiences A-fib, the atria are not contracting as they normally would. They are just quivering. This absence of contraction of the atria can result in a loss of cardiac output anywhere from 15 - 30% due to the absence of "atrial kick". This is why the heart rate is so high. The body is trying to maintain homeostasis.
- It will be impossible to determine the atrial rate. You will only be able to analyze and report the ventricular rate.
- Atrial Fibrillation with a ventricular response in excess of 100 bpm is commonly referred to as Atrial Fibrillation with “rapid ventricular response” or "uncontrolled A-fib".
- Rate: Ventricles - 90, Atria - Unable to determine (UTD)
- P wave: "f" waves
- Interpretation: Atrial Fibrillation
Lesson #8: Quiz Test Questions 312
This website provides professional medical education. For medical care contact your doctor. 2024 ©MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us | 1
Wandering Pacemaker
When several pacemakers are competing, p-waves with different origins and thus configurations occur. The rhythm is slightly different from beat to beat.
note If the heart rate increases to above 100bpm, it is called Multifocal Atrial Tachycardia . Possible causes are hypoxia, COPD and medication such as digoxin.
Navigation menu
IMAGES
VIDEO
COMMENTS
Wandering Atrial Pacemaker (WAP) is a cardiac rhythm disorder that causes irregular and variable heartbeats. Learn the Heart - Healio provides a comprehensive ECG review of this condition ...
This results in at least three different P wave morphologies, and often the PR interval may vary due to this. If the heart rate is less than 100 BPM we call this a wandering atrial pacemaker, or WAP. If it's greater than 100 BPM we call it a multifocal atrial tachycardia, or MAT for short.
A wandering atrial pacemaker is usually found with an electrocardiogram ( EKG or ECG). It's a test that lets your doctor see a record of the electrical signals in your heart. If the irregular ...
Wandering atrial pacemaker (WAP) is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. This is different from normal pacemaking activity, where the sinoatrial node (SA node) is responsible for each heartbeat and keeps a steady rate and rhythm. Causes of wandering atrial pacemaker are unclear, but there may be factors leading to its ...
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.
The electrical impulses causing the atrial activity are moving or wandering. Observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular. Wandering atrial pacemaker is an arrhythmia originating in shifting pacemaker sites from the SA node to the atria and back to the SA ...
This rhythm and multifocal atrial tachycardia are similar except for heart rate. The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity. Usually, it is associated with underlying lung disease. In the elderly, it may be a manifestation of sick sinus syndrome.
Wandering Atrial Pacemaker Rhythm Strip Features. Rate: Normal (60-100 bpm) Rhythm: May be irregular. P Wave: Changing shape and size from beat to beat (at least three different forms) PR Interval: Variable. QRS: Normal (0.06-0.10 sec) The electrical impulses causing the atrial activity are moving or wandering.
Three or more ectopic foci within the atrial myocardium serve as the pacemaker; Rate is less than 100bpm (in contrast to MAT) Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia; Causes. Intrinsic cardiac or pulmonary disease; Metabolic derangements; Drug toxicity (including Digoxin) Clinical Features
AF is addressed in the 2014 ACC/AHA/HRS Guideline for the Management of Atrial Fibrillation (2014 AF guideline). 10 The present guideline addresses other SVTs, including regular narrow-QRS complex tachycardias, as well as other, irregular SVTs (eg, atrial flutter with irregular ventricular response and multifocal atrial tachycardia [MAT]).
Analysis. In Wandering Atrial Pacemaker ECG, you must observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular. The PR interval is often affected, but does not have to be. The bottom line, is you must observe at least three different shaped P waves.
Whereas atrial tachycardia is due to a single ectopic focus in the atrium, wandering atrial pacemaker and MAT are due to multiple microreentry foci in the atrium. If the ventricular rate is less than 100 bpm, it is considered a wandering atrial pacemaker; if the ventricular rate is greater than 100 bpm, it is considered MAT.
Name that strip: Answers. Rhythm: Irregular. Rate: 60 beats/minute. P waves: Vary in size and shape. PR interval: 0.08 to 0.12 second. QRS complex: 0.04 to 0.08 second. Interpretation: Wandering atrial pacemaker. Wandering atrial pacemaker (WAP) occurs when the pacemaker site shifts back and forth between the sinus node and ectopic atrial sites ...
The pacemaker is activated and delivers a stimulus only when the intrinsic ventricular rate falls below a predetermined lower limit; pacemaker activity is suppressed when …. ECG tutorial: Basic principles of ECG analysis. … block; multifocal atrial rhythm (wandering atrial pacemaker) when the rate is <100 or multifocal atrial tachycardia ...
A wandering atrial pacemaker is an atrial arrhythmia that occurs when the natural cardiac pacemaker site shifts between sinoatrial and atrioventricular nodes. ... including an irregular beat, an extra beat, and a fast or slow heart rate. ... The differential diagnosis involves sinus tachycardia with regular premature atrial contractions and ...
A rapid, irregular atrial rhythm arising from multiple ectopic foci within the atria. Most commonly seen in patients with severe COPD or congestive heart failure. It is typically a transitional rhythm between frequent premature atrial complexes (PACs) and atrial flutter / fibrillation. AKA "Chaotic atrial tachycardia".
Recognize the difference between regular and irregular rhythms; ... The criteria is the same as Wandering Atrial Pacemaker with the only difference being the heart rate exceeds 100 bpm. ... morphology of the P waves. Remember, you must observe at least three different shaped P waves. Due to the presence of irregular R to R intervals coupled ...
Wandering Pacemaker. Wandering pacemaker. Every p-wave is different and thus has a different origin. When several pacemakers are competing, p-waves with different origins and thus configurations occur. The rhythm is slightly different from beat to beat. note If the heart rate increases to above 100bpm, it is called Multifocal Atrial Tachycardia.
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury. ... His pulse was irregularly irregular at 78/minute, and his blood pressure was 110/ ...
Sinus arrhythmia is lethal; wandering atrial pacemaker is benign. Sinus arrhythmia has a regular rhythm; wandering atrial pacemaker is irregular., Atrial fibrillation has _____. no P waves at all P waves with uniform shape sawtooth-shaped waves between the QRS complexes P waves of multiple shapes and more.
A) Sinus arrhythmia has uniform P wave shapes; wandering atrial pacemaker has at least three different shaped P waves. B) Sinus arrhythmia has a regular rhythm; wandering atrial pacemaker is irregular. C) Sinus arrhythmia has a heart rate of less than 100; wandering atrial pacemaker has a rate greater than 100.