You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Pregnancy Symptoms 5
- Can I get pregnant if… ? 3
- Paternity Tests 2
- The Bumpy Truth Blog 7
- Multiple Births 10
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Cord Blood 4
- Pregnancy Supplements & Medications 14
- Pregnancy Products & Tests 8
- Changes In Your Body 5
- Health & Nutrition 2
- Labor and Birth 65
- Planning and Preparing 24
- Breastfeeding 29
- Week by Week Newsletter 40
- Is it Safe While Pregnant 55
- The First Year 41
- Genetic Disorders & Birth Defects 17
- Pregnancy Health and Wellness 149
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Uncategorized 4
- Women's Health 34
- Prenatal Testing 16
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
- Pregnancy Questions Center
Share this post:
Similar post.

Pregnancy and Ice Cream

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict
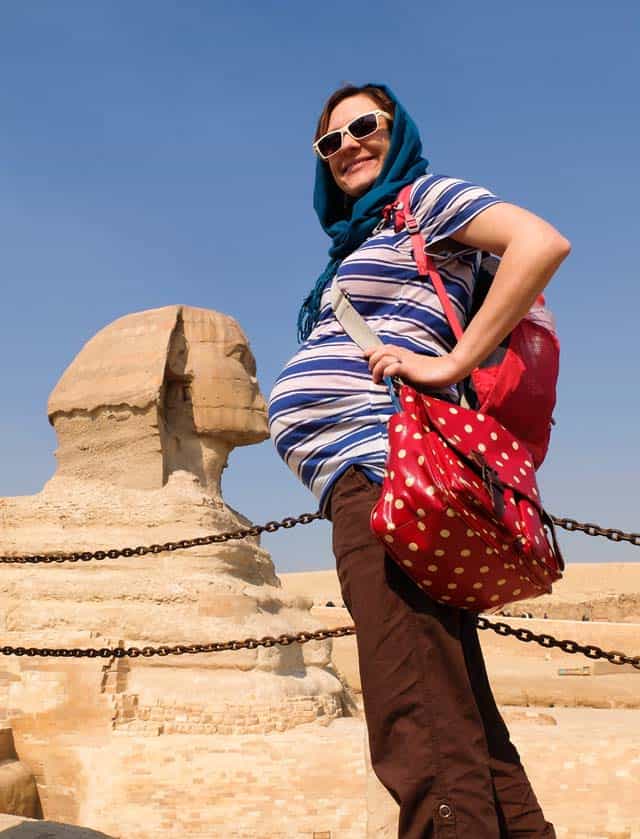
When I told people that I was planning to travel to a foreign country while 7 months pregnant, I got looked at like I was crazy. The look turned into shock when they heard I was going to a developing country: Egypt.
“Is it safe to travel while pregnant?”
“Can you fly while pregnant?”
“What if something happens???”
There are some legit concerns about traveling abroad while pregnant – but those can easily be addressed by making some smart travel choices and precautions.
This is NOT Your Last Chance to Travel
Apparently, most people believe that their lives come to a screeching halt once they have a baby. They have to travel “while they still can.” There is even a name for these pregnancy holidays – a “ babymoon .”
Fear that this is your “last chance to travel” is a terrible reason to plan a trip!!!
It is perfectly possible to travel with a baby . In some ways, traveling with a baby is even more fun (such as how you get priority treatment and meet locals easier). So don’t feel pressured to rush out and take a trip “while you still can.” There will be plenty of opportunities to travel later on.

Get the Timing Right
I am one of those unlucky women who gets hyperemesis gravidarum during pregnancy. Don’t confuse HG with morning sickness. I’m talking about puking blood because the vomit has eroded your throat. I’m talking about getting IV transfusions because I couldn’t keep water down…
So it was a bad mistake to go backpacking while 4 weeks pregnant . I ended up having to cut the trip short. It’s no fun puking all over the trail!!!
But, because this was my second pregnancy, I knew that I would probably stop puking at 6 months. So that’s when I planned my Egypt trip for.

You don’t know how you’ll feel as pregnancy progresses, so here’s what I’d recommend about planning a trip abroad:
- Go during months 6 or 7: In general, these are the best months for most pregnant women. The hormones and morning sickness have leveled off, but you aren’t so huge that you tire easily.
- Wait until the last minute to plan your trip: If possible, hold off on planning your trip until you know how you feel.
- Check refund policies: Most travel insurance policies don’t allow pregnancy as a reason for cancellation . So, be sure you understand cancellation/refund policies. Otherwise you’ll be out a lot of money if you decide to cancel the trip because you feel too crappy.
You Probably Can’t Get Travel Health Insurance while Pregnant
One of the biggest issues with traveling abroad while pregnant is that almost no travel insurance company will give coverage to pregnant women.
If something happens while on your trip, you’ll be stuck with the bill!
Consider the case of Jennifer Huculak-Kimmel and her “ million dollar baby .” The Canadian couple were on vacation in the USA when Jennifer went into premature labor. Two months in the ICU ran up a hospital bill of $950,000 – none of which was covered under her insurance policy!
I admit that the idea of being saddled with a huge hospital bill terrified me. Before going to Egypt, I intensely researched the cost of giving birth there, as well as how much a night in ICU would cost. Egypt is a poor country, so the costs weren’t too high – so I was willing to take the risk.
Know Airline Policies for Pregnant Women

Flying while pregnant is perfectly safe . The real reason that airlines put restrictions on flying while pregnant is because they are afraid you will give birth in the air.
Thus, a lot of airlines won’t let pregnant women fly after 36 weeks (or 32 weeks if you are having multiples). You may need a doctor’s note before being allowed to fly. This was the case with Air Cairo. The note had to be no more than 7 days old, so I actually had to visit a gynecologist while in Egypt – which was actually a cool part of the trip.
You can find a good breakdown on airline pregnancy restrictions here .
Choose the Right Climate
Since you are already going abroad, you might as well choose an agreeable climate! The entire reason we chose Egypt for our trip was because it was January.
While everyone else was battling snow, we were swimming in the Red Sea!
However, there is no way in hell that I’d go to Egypt in summer while pregnant. For a summer trip, I would have chosen a cooler country like Norway or gone into the mountains.

Only Plan ONE Activity Per Day
In general, I’m not the type of traveler who tries to see/do a zillion things. But I knew to take it even easier while pregnant.
I made a list of the things I absolutely wanted to do in each destination. Then planned to do just one per day. Some days we managed to do more than one thing, but only if I still felt up to it. This kept the pace relaxed so I didn't inadvertently overexert myself.
Consider the Bathroom Situation
One piece of travel advice for pregnant women which commonly gets overlooked is the bathroom situation. Since pregnancy makes you pee like crazy, this is not something which should not be overlooked.
Going to the bathroom actually ended up being the hardest part of traveling abroad while pregnant. After this ordeal, here’s what I’d recommend to other pregnant travelers:
- Make sure you can squat: Public bathrooms aren’t exactly known for their cleanliness – do you really want to sit on them? If you can’t squat over them, you are going to be in for some trouble. Squats are great exercises for preparing for childbirth anyway. 😉
- Consider a pee funnel: If you can’t squat, then get a pee funnel . This makes it possible to pee standing up.
- Map out some nicer restaurants: As is the case in many developing countries, it was very hard to find a bathroom in Egypt. The local restaurants didn’t have bathrooms (seriously!) and cafes usually only had a bathroom for men (which might just be a bucket in a corner!!!). The tourist restaurants consistently had nice bathrooms, so I mapped these out so I knew where to go to pee.
- Carry TONS of wet wipes and antiseptic gel: Once you have a baby, you’ll be carrying tons of these anyway. 🙂 For traveling abroad, these come in handy for wiping down disgusting surfaces and sanitizing your hands – don’t expect soap in every bathroom!

Budget for Luxury Transportation
Normally I’m fine taking cramped minibuses and crowded trains. But, at 7 months pregnant, I wasn’t keen about shoving into Egypt’s crowded local transportation.
It probably would have ended with me puking or passing out. Or, worse, someone banging into my stomach.
Luckily we were able to afford taxis everywhere (we used Uber to avoid haggling with the crooked taxi drivers). We took things a step further and even hired a private driver to take us between cities.
Since it was Egypt (and not, for example, Norway), it wasn’t too expensive. In developed countries, this sort of luxury travel will definitely cost more.
Even a short taxi ride each day in somewhere like Europe can add a huge amount to your travel budget. But in developed countries the public transportation won’t be as crazy. So really think about the cost vs. hassle of public transport and budget your trip accordingly.

Some Activities Will Be Off-Limits While Traveling Pregnant
In the weeks before my Egypt trip, I was Googling things like “Can you ride a camel while pregnant?”
It turns out that riding a camel is a relatively safe activity while pregnant (riding a horse, however, is not). But, to play it safe, I still decided not to ride a camel while at the pyramids.
I also had to pass on sandboarding, quad biking, and going into certain tombs (because of low oxygen levels inside). Unfortunately, it was only after I got into a jeep on our excursion into the desert that I realized that off-roading might be off-limits too! Luckily, the ride wasn't too bumpy — but I still held on tightly to prevent my stomach from getting bounced too much.

Playing It Safe with Food while Pregnant
Another major concern I had about traveling to Egypt (or any developing country) while pregnant was getting a stomach bug from tainted water or food.
Most of the time, food poisoning while pregnant isn’t particularly danger. The biggest risk is that you’ll get dehydrated.
The best thing to do is avoid food poisoning in the first place:
- Only drink safe water. I stuck to bottled water. I also have a Sawyer Mini water filter in case bottled water isn’t available.
- Remember to avoid ice cubes and juices too! Unless you know these were made with safe water, don’t drink them.
- Be cautious about street food. My doctor told me to not eat any street food. But that’s half the fun of traveling abroad! So I instead was careful about the street food I ate. I stuck with thing that were deep fried since this would have killed most bacteria. I’m vegetarian, but would have avoided all street meat regardless.
- Take probiotics the first few days. This will help your body adjust to and combat any “bad” bacteria it comes in contact with.
In case you do develop a stomach bug, the CDC says it is best to wait for it to go away on its own (if it’s severe, that’s when you’ll want to contact a doctor). You’ll need to stay hydrated while waiting for the diarrhea and vomiting to subside.
My traveler’s first aid kit is always stockpiled with electrolytes. It also has activated charcoal and other remedies for food poisoning.

Enjoy the Memories
Taking a trip while I was 7 months pregnant was by far the best decision I made – for both me and my family.
It was a much-needed break from all the pregnancy woes. For the first time in months, I stopped frantically Googling everything pregnancy related. I was able to RELAX and enjoy myself!
Even more importantly, I was able to spend some quality time with my husband and older daughter.
If I had a high-risk pregnancy, then I wouldn’t have done the trip. But for any other pregnant travel addicts who need a break from focusing on their growing baby, a trip is great for your mental health.
My only regret is that I didn’t take more photos using my bump. It would have been great to have a funny picture of my belly with a pyramid coming out of it. 🙂
Have you traveled abroad while pregnant? What tips would you add?
Image credit: squat toilet , by Maksym Kozlenko , Creative Commons Attribution-Share Alike 4.0 International license
Sharing is caring!
1 thought on “Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict”
Pingback: Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict – Cuddle Baby
Comments are closed.
- Search Please fill out this field.
- Newsletters
- Trip Planning
Flying While Pregnant? Check Out the Policies on 25 Global Airlines
In the absence of obstetric or medical complications, occasional air travel during pregnancy is generally safe, according to the American College of Obstetrics and Gynecology (ACOG). Like other travelers, pregnant women should use seat belts while seated.
Most commercial airlines allow pregnant women to fly up to 36 weeks of gestation, with some restrictions on international flights.
ACOG does not recommend air travel for pregnant women with medical or obstetric conditions that may be exacerbated by flight or that could require emergency care. It advises checking flight durations when planning travel and that the most common obstetric emergencies occur in the first and third trimesters.
Once aboard a flight, conditions including changes in cabin pressure and low humidity, coupled with the physiologic changes of pregnancy, do result in adaptations, including increased heart rate and blood pressure, reports ACOG. And those traveling on long-haul flights face the risks associated with immobilization and low cabin humidity. This can cause issues such as lower extremity edema and venous thrombotic events.
ACOG recommends preventive measures to minimize these risks, including the use of support stockings, regular movement of the lower extremities, avoid wearing restrictive clothing and encourage regular hydration. It also advises against consuming gas-producing foods or drinks before a flight.
Other ways for pregnant women to be comfortable on their flights include: booking a bulkhead seat for more legroom; reserving an aisle seat for easy access to lavatories and to walk; elevating your legs on a carry-on bag to avoid swelling and cramps; and wearing a layered, comfortable outfit for changing cabin temperatures.
Airlines around the world have different rules and regulations on when and how long pregnant women can fly. Below are the policies from 25 airlines around the world.
The French flag carrier does not require pregnant women to carry a medical certificate for travel during pregnancy. It recommends avoiding travel in the final month of pregnancy, as well as during the first seven days after delivery. The airline also recommends expecting mothers seek their doctor's opinion before traveling.
India’s flag carrier allows expectant mothers in good health to fly up to and including their 27th week of pregnancy. After 27 weeks, if the pregnancy is anticipated to be a normal delivery, an expectant mother will be accepted for travel up to the 35th week, but a medical certificate confirming the mother is fit to travel is required by an attending obstetrician and dated within three days of travel.
Air New Zealand
For single, uncomplicated pregnancies and clearance from a doctor or midwife women can take flights more than four hours up to the end of their 36th week. For flights under four hours, it's up to the end of the 40th week. Women pregnant with twins can fly more than four hours up to their 32nd week and less than four hours until the 36th week.
The airline recommends that women past their 28th week carry a letter from a doctor or midwife that says you are fit for travel, confirming your pregnancy dates and that there are no complications.
The airline's medical team must offer clearance for women experiencing the following: a complicated pregnancy, such as placenta previa or bleeding; a multiple pregnancy; a history of premature labor; or have begun the early stages of labor.
Italy's flag carrier has no travel restrictions for expectant mothers during the first eight months of pregnancy. But if traveling within the last four weeks of pregnancy, expecting multiple births, or having a complicated pregnancy, medical clearance is required. Completion of a Medical Information Form, MEDIF , prior to travel and signed by both the passenger and doctor is required.
Alitalia advises pregnant not to fly seven days prior to and seven days after giving birth, or if there is a risk of a premature birth or other complications. It will make staff available to escort pregnant women from the airport check-in counter to the boarding gate. Staff onboard the flight will help stow carry-on luggage. Seats can be pre-assigned and women cannot sit in an exit row.
All Nippon Airways
The Japanese carrier requires women within 15 to 28 days of their due date to fill out and carry a medical information form . Women within 14 days of their due date are required to have a medical form and travel with a doctor. The form must indicate there are no complications of pregnancy, that the passenger has no health problems preventing them from flying and the due date. It must be completed by a doctor and submitted no more than seven days prior to departure.
American Airlines
The Fort Worth-based carrier has different rules for international and domestic flights. If a due date is within four weeks of a flight, you must provide a doctor’s certificate stating that you’ve been recently examined and you’re fit to fly. For domestic flights under five hours, pregnant women won’t be permitted to travel within seven days (before and after) their delivery date. Those who need travel within this timeframe will need approval from a physician and help from a special assistance coordinator . The pregnant woman's physician will be required to fill out a passenger medical form before a flight. A special assistance coordinator will send the form directly to your physician.
Clearance from a special assistance coordinator is required for international travel or travel over water. Within four weeks of a due date also requires a physician's note stating that you’ve been examined within the past 48 hours and you’re fit to fly. And seven days before or after delivery also requires a passenger medical form to be completed by your physician.
British Airways
The U.K. carrier does not allow pregnant women to fly after the end of the 36th week if you are pregnant with one baby or the end of the 32nd week if you are pregnant with more than one baby. While it isn't mandated, British Airways recommends all expecting mothers carry a confirmation from a doctor or midwife, such as a letter or certificate, in addition to your pregnancy record. It should be written within seven days prior to travel and confirm your approximate due date, that you're fit to travel and that there are no complications with your pregnancy.
Cathay Pacific
Hong Kong's flag carrier requires that women with pregnancies after 28 weeks carry a medical certificate, dated within 10 days of travel that states the following:
- single or multiple pregnancy
- estimated week of pregnancy
- expected due date
- certifying you are in good health and the pregnancy is progressing normally, without complications
- that you are fit to travel
The airline accepts pregnant women with uncomplicated single pregnancies to travel up to 36 weeks and uncomplicated multiple pregnancies up to 32 weeks.
Delta Air Lines
The Atlanta-based carrier does not impose restrictions on flying for pregnant women, so a medical certificate is not required to travel. But the airline will not waive ticket change fees and penalties for pregnancy. The airline recommends that those flying after their eight month should check with their doctor to be sure travel is not restricted.
The U.K.-based airline has no restrictions for pregnant passengers traveling up to the end of the 35th week of single pregnancies and the end of the 32nd week for multiple pregnancies.
Pregnant women can travel up to their 29th week without a medical certificate. After that, they require a certificate or letter signed by a qualified doctor or midwife that states whether the pregnancy is single or multiple, is progressing without complications, includes an estimated due date, that you are in good health and there's no known reason to prevent you from flying. Pregnant passengers are not allowed to fly after the 32nd week of a multiple pregnancy, and after the 36th week of a single pregnancy.
This Abu Dhabi-based carrier allows women with single or multiple pregnancies to travel during the first 28 weeks without a medical certificate. For single pregnancies between 29 and 36 weeks, a medical certificate is required. After 37 weeks, pregnant women will not be allowed to travel. For multiple pregnancies, a certificate is required between the 29th and 32nd week; after that, women will not be allowed to travel.
The medical certificate must include the following:
- Be issued and signed by a doctor or midwife
- Written on a clinic/hospital letterhead and/or stamped by the doctor or midwife
- State that the guest is fit to fly
- State if the pregnancy is single or multiple
- State the number of weeks of pregnancy and the Expected Date of Delivery
- Easily understood and written in Arabic or English. Other languages are accepted but must be verified by Etihad Airways' check-in staff
The original medical certificate shall be accepted for the whole journey (originating, return and stopover flights), provided the above validity criteria is met for each sector. And it is valid for three weeks from the date of issue.
The New York-based carrier does not allow pregnant customers expecting to deliver within seven days to travel unless they provide a doctor's certificate dated no more than 72 hours prior to departure stating that the woman is physically fit for air travel to and from the destinations requested on the date of the flight and that the estimated date of delivery is after the date of the last flight.
The Dutch flag carrier recommends pregnant mothers not fly after the 36th week, along with the first week following delivery. For those expecting more than one baby, the carrier recommends consulting with a physician prior to flying. If you have had complications, you always need to have permission to fly from your physician.
Expectant mothers with complication-free pregnancies can fly on the German flag carrier until the end of the 36th week of pregnancy or up to four weeks before their expected due date without a medical certificate from a gynecologist. But the airline recommends that pregnant women beyond the 28th week have a current letter from a gynecologist that includes confirmation that the pregnancy is progressing without complications and the expected due date. The doctor should expressly state that the patient’s pregnancy does not prevent her from flying.
Because of the increased risk of thrombosis during pregnancy, the airline does recommend that expectant mothers wear compression stockings while flying.
Malaysia Airlines
The Malaysian flag carrier requires medical clearance for expectant mothers approaching 35 weeks for international travel or 36 weeks for domestic travel. If medical clearance is required, the MEDIF application form should be completed by a doctor and submitted to the airline through its ticketing offices or travel agents at least five working days before traveling.
Philippine Airlines
An expectant mother who is in normal health and with no pregnancy complications will be allowed to fly after filling out an EMIS form . Pregnant women may be accepted for travel if they are not beyond 35 weeks when they fill out Part One of the EMIS form. Those between 24 and 32 weeks of pregnancy will have to fill out EMIS Form Part 2. And if the expectant mother is below 21 years of age, the consent in writing of the husband, parent or guardian must be secured. For expectant mothers beyond 32 weeks of pregnancy, EMIS Part 3 must be accomplished by the Flight Surgeon or Company Physician, who shall issue the clearance for travel
After the 28th week, women are required to have a certificate or letter from a registered medical practitioner or registered midwife confirming the delivery date, whether it's a single or multiple pregnancy and that the pregnancy is routine.
For flights longer than four hours, women can fly up to the end of the 36th week for single pregnancies and the end of the 32nd week for multiple pregnancies. For flights under four hours, women can travel up to the end of the 40th week for single pregnancies and the end of the 36th week for multiple pregnancies. The carrier requires medical clearance if there are pregnancy complications or it's not a routine pregnancy.
Qatar Airways
No doctor's note is required for women traveling through their 28th week of pregnancy. Expectant mothers can fly between week 29 and week 32 with a doctor's note and a pregnancy with no complications. Those with a multiple pregnancy will need a doctor's note and a Medical Information Form (MEDIF) . Between weeks 33 and 35, women will need a doctor's note and a MEDIF. The airline does not accept women in their 36th week and beyond.
The low-cost Irish carrier allows expectant mothers to fly up to their 28th week of pregnancy. After that, the airline requires women to have a ‘fit to fly’ letter from their midwife or doctor. For an uncomplicated single pregnancy, travel is not permitted beyond the end of the 36th week of pregnancy, while the cut-off for an uncomplicated multiple pregnancy is 32 weeks.
Singapore Airlines
For uncomplicated single pregnancies, the carrier restricts expectant mothers from travelling beyond the 36th week of pregnancy; for uncomplicated multiple pregnancies, the restriction is the 32nd week.
For uncomplicated single pregnancies between 29 weeks and 36 weeks, expectant mothers must provide a medical certificate stating the following: (1) fitness to travel, (2) number of weeks of pregnancy and (3) estimated date of delivery. The certificate should be dated within ten days of the date of the first flight exceeding 28 weeks of pregnancy. This certificate will have to be presented at check-in when requested.
Southwest Airlines
The Dallas-based carrier advises expectant mothers at any stage of pregnancy to consult with their physicians prior to air travel. The airline recommends against air travel beginning at the 38th week of pregnancy. It warns that in some cases, traveling by air has been known to cause complications or premature labor. Depending on their physical condition, strength, and agility, pregnant women may, in some cases, be asked not to sit in the emergency exit row.
Turkish Airlines
Turkey's flag carrier allows mothers pregnant with one child to travel between the 28th and 35th week if they have a doctor's report that includes the phrase, “There is no particular reason for the patient not to fly.” For women pregnant with more then one baby, the travel cut-off is the end of the 31st week with a doctor's report. The report has to be no more than seven days from the travel date.
United Airlines
Any woman in the first 36 weeks of pregnancy will be allowed to travel on the Chicago-based carrier without medical documentation. An expectant mother traveling after the 36 weeks of pregnancy must have the original and two copies of an obstetrician’s certificate, which must be dated within 72 hours of a flight’s departure. The original certificate should be submitted to a United representative at check-in.
Virgin Atlantic
The London-based airline allows travel without restrictions until the 28th week of pregnancy provided that you're free from complications to that point. The carrier asks pregnant mothers to inform its Special Assistance department so they can offer appropriate inflight health advice. Between the 28th and 36th weeks of pregnancy, a doctor's or midwife's certificate is required, stating that the passenger is safe for travel and the expected due date (32 weeks if carrying multiples in an uncomplicated pregnancy). Beyond the 36th week of pregnancy, travel is only permitted for medical/compassionate reasons and the pregnant passenger is required to be accompanied by a medical escort. This travel is subject to the approval of a Virgin Atlantic doctor.
Related Articles
More related articles.
Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Protect Your Trip »
15 Tips for Traveling While Pregnant
These tips will help pregnant women travel the world in comfort and style.

Getty Images
Experts share their best travel tips for expecting mothers.
Pregnancy can be a magical experience, but that doesn't mean creating new life comes without challenges. From what you wear to how you move your body to how well you sleep, pregnancy changes your day to day in myriad of ways – both good and bad.
However, that doesn't mean you should stay home and avoid travel for the entire nine months you're with child. The American College of Obstetricians and Gynecologists says it's typically safe to travel until you're 36 weeks pregnant, so you may as well get out and see the world.
These tips can help you ensure your pre-baby travel is safe, comfortable and fun.
Travel When You're Most Comfortable
According to the ACOG, the best time for pregnant women to travel is between 14 and 28 weeks, or during the middle of your pregnancy.
The most common pregnancy problems occur in the first and third trimesters, according to the health organization. "During midpregnancy, your energy has returned, morning sickness usually is gone, and it is still easy to get around," according to the ACOG.
If you have the option to be flexible with your travel dates, steering clear of early and late pregnancy trips may save you from having to endure an unenjoyable experience.
[Read: 9 Reasons Getting Away for the Weekend is Good for Your Mental Health .]
Have a Plan B
Robert Quigley, senior vice president at International SOS and MedAire, says you should meet with your doctor and get cleared to travel before you depart on any trip. Also, take the time to research medical facilities near where you'll be staying, he says, since you won't want to have to frantically figure out where to go if you experience complications.
Early planning can include checking nearby hospitals that you contact ahead of your trip, and locating pharmacies and additional prenatal resources in your destination should you go into early labor.
"This may also include a communication plan for friends or family should they need to join you, and an evacuation plan to upgrade your care in the event of a complication," he says.
Purchase Travel Insurance
Travel writer and mom of two Natalie Preddie, who blogs at NattyPOnline.com , says you should buy travel insurance that includes medical coverage before your trip if you're visiting a destination where your health insurance won't apply.
Preddie says when she was pregnant, she had to go to a hospital in Florida during a trip because she thought her baby wasn't moving. She says she was glad her health insurance was accepted right away, but she worries what would have happened if she had to pay for a lengthy hospital stay or tests out of pocket.
Bring Your Medical Records with You
Lee Roosevelt, who works as nurse midwife at the University of Michigan – Ann Arbor, says you can gain peace of mind and expedite any medical care you might need by bringing a copy of your pregnancy-related medical records along on your trip.
"Offices can take a day or two to return a request for records, and if you need care quickly it means your team of providers [is] making decisions without knowing the details of your pregnancy," she says.
Be Proactive About Your Health
Roosevelt also says that when it comes to pregnancy, you should take steps to avoid common health problems regardless of whether you're on a trip or at home. She recommends taking plenty of walking breaks since "pregnant women are at higher risk for blood clots and prolonged sitting increases that risk."
You should try to get up and walk for five to 10 minutes every few hours if you can, even if you're on an airplane.
Roosevelt also noted that buying and wearing compression socks during air travel can help you avoid swelling, blood clots and more.
[Read: 30 Travel Accessories That Make Vacationing Easier .]
Stay Hydrated
In the same vein of being mindful about your health and wellness, drink lots of water so you stay hydrated. Dehydration can make you feel unwell and put you at risk for pre-term contractions, Roosevelt says.
Plan to bring your own refillable water bottle while you travel so you can stay hydrated no matter where you are, whether that's on the road or in the air.
Pack Healthy Snacks
Airports don't always have many healthy dining options, and what is available tends to be expensive. To save money and avoid having to nosh on empty calories, it can help to bring your own selection of sensible snacks along.
Consider packing healthy snacks like dried fruit and vegetables if you can. The U.S. Department of Health and Human Services also recommends eating whole grain toast or crackers when you’re feeling nauseous or unwell, and healthy crackers should be easy to pack in your bag and bring along.
Bring Sanitizing Wipes and Gel
The ACOG says that, if you're going on a cruise specifically, you'll want to take steps to avoid norovirus – a group of viruses that can spread quickly and cause severe nausea and vomiting.
Washing your hands frequently is the best way to avoid it, but antibacterial hand gel can help you ward off germs as well. Meanwhile, disinfecting wipes are good to have on hand to wipe down airplane tray tables and arm rests.
The Government of Canada also recommends pregnant women vigorously wash their hands before eating or preparing food as well. Following these recommendations is especially important when you're in a busy airport or dining on a germ-infested airplane.
Keep Car Rides Short
If you're planning a road trip or need to drive a long distance to reach your destination, it can be beneficial to break up your travel over several days. That way, you'll only have to sit for shorter spurts of time rather than long stretches that can leave you vulnerable to swelling, blood clots and other pregnancy-related complications.
The ACOG also notes that you should buckle your seatbelt low on your hipbones, below your belly, and "place the shoulder belt off to the side of your belly and across the center of your chest."
Plan to make frequent stops so that you can get out and stretch your legs, and your car ride will be more enjoyable and keep you and the baby safe.
Book an Aisle Seat When You Fly
If you plan to fly while you're pregnant, book an aisle seat ahead of time – even if you need to pay extra for it. Having an aisle seat will make it easier for you to get up and walk around, and to head to the toilet for the many bathroom breaks you'll likely need to take.
If you can, splurge (or use points ) for business class to score some extra room.
Don't Overbook Yourself
Sightseeing is a lot of fun pregnant or not, but don't forget that your energy levels may be lower by the time you're ready to depart.
Make sure to plan an itinerary that includes plenty of breaks and downtime. You may even want to plan a relaxation-themed trip altogether, such as a spa getaway or a trip to an all-inclusive resort .
Be Choosy About Your Destination
Be mindful of seasonal weather trends and how they might work for your pregnant self. If you are planning a beach getaway in the middle of July and considering Naples in southern Florida, for example, it's smart to know ahead of time that daily high temperatures usually reach 89 degrees and humidity levels often fall in the "oppressive" or "miserable" range in the summer. Doing your research could help you find a destination with better weather, such as a beach spot with lower humidity like Virginia Beach, Virginia or Cape Cod, Massachusetts .
When it comes to trip planning, Google is your friend. Make sure you know how the weather might look no matter where you are planning to travel or you could live to regret it.
[See: 30 Relaxing Meditation Retreats Around the World .]
Pack a First-Aid Kit
There's nothing worse than being in transit for hours without supplies for headaches, heartburn and other pregnancy-related ailments. If you're prone to not feeling well at home or when you travel, you may want to bring a small first-aid kit along.
While your kit can include whatever you want, consider packing medicine for heartburn, bloating, gas and nausea – or whatever has been bugging you the most.
Check If You Need Clearance to Fly
While most airlines let you fly without question until you're up to 36 weeks pregnant, some international carriers, including Cathay Pacific and Emirates, need verification of your health from your doctor with a medical certificate before you board the plane.
If you plan to fly domestically or abroad, make sure to check with the air carriers you're considering as you organize the trip. Most airlines typically list this information on their websites, but you can also call to ask if you'll need any specific documentation.
Choose the Right Luggage
Finally, don't forget to bring luggage that's easy to move around from place to place. Spinner-style luggage on wheels is typically the easiest to transport, and you should strive to pack light (within reason) so you're not stuck lugging around all the clothing and shoes you own.
Don't hesitate to check your luggage either – especially if you have a layover to endure. The less you have to carry around, the smoother your trip should be.
30 Top Babymoon Destinations

Tags: Travel , Vacations , pregnancy , parenting , Family Vacations , Travel Tips
World's Best Places To Visit
- # 1 South Island, New Zealand
- # 4 Bora Bora
If you make a purchase from our site, we may earn a commission. This does not affect the quality or independence of our editorial content.
You May Also Like
The best weekend getaways from nyc.
Alissa Grisler and Jessica Colley Clarke Sept. 5, 2024

The Best Beach Resorts in the World
Sept. 5, 2024

The 10 Best Rome Food Tours
Laura Itzkowitz Sept. 4, 2024

Top Things to Do in Hershey, PA
Amanda Norcross Aug. 30, 2024

The Best College Town Hotels
Rachael Hood Aug. 29, 2024

Fun Fall Weekend Getaways
Aug. 29, 2024

Best Hoover Dam Tours from Las Vegas
Holly Johnson and Ann Henson Aug. 29, 2024

The Best London Tours
Kim Foley MacKinnon Aug. 29, 2024

The 18 Best Barcelona Tours
John Rodwan Aug. 28, 2024

Best Fall Family Vacations
Aug. 27, 2024

- Search Please fill out this field.
- Newsletters
- Sweepstakes
Here Are the Rules for Flying When You're Pregnant
Whether you're newly pregnant or planning a babymoon right before welcoming your baby, here's what parents-to-be need to know about airline travel during each trimester.
GETTY IMAGES
Expectant parents need to know: Can you fly when pregnant?
While it's mostly OK to travel until the last few weeks of pregnancy, there are some precautions to take depending on when you decide to book a trip and how high risk your pregnancy is. Here's what you need to know before your next vacation.
Pregnancy and Flying: Your Trimester by Trimester Guide
As a general rule of thumb, most airlines will allow pregnant people to fly right up until week 36 of pregnancy, but you should absolutely do your research before booking your flight to check restrictions. You'll also want to consult with your OB-GYN or midwife before traveling—especially if you're at a higher risk for complications during pregnancy.
Before you travel
While you may be accustomed to planning a vacation on a whim or only packing your usual necessities, there's one extra thing you should consider doing before booking a flight during your pregnancy: Opt for travel insurance.
Should travel restrictions change, your health care provider recommends you stay home, or if you experience any concerning symptoms —like bleeding, abdominal pain, swelling, headaches, vision changes, or decreased fetal movement—you'll want to postpone or cancel your plans and see your doctor as soon as possible.
According to the ACOG, travel is not recommended for pregnant people with certain complications like preeclampsia, premature rupture of membranes (PROM), or who are at risk of preterm labor.
First trimester
Flying earlier on in pregnancy is actually considered pretty safe. And, no, metal detectors won't harm your fetus.
"Pregnant women can observe the same basic precautions for air travel as the general public," Raul Artal, M.D., former vice chairman of the American College of Obstetricians and Gynecologists (ACOG) Committee on Obstetric Practice, previously told Parents .
One thing pregnant air travelers should take extra precautions to avoid at any trimester? Blood clots, which pregnant people are 7 times more likely to develop—especially during long flights. To help minimize your risk, you can book an aisle seat, walk around every so often, and wiggle your legs and toes while seated.
And since morning sickness and fatigue might be your biggest first trimester complaints, you may want to check with your health care provider about bringing anti-nausea medicine with you.
Second trimester
According to the ACOG, "The best time to travel is mid-pregnancy (14 to 28 weeks). During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily. After 28 weeks , it may be harder to move around or sit for a long time."
If you're flying during your second trimester, it's a good idea to stay hydrated, think about wearing support stockings to reduce edema and clot risk, and make sure you've done your research on hospitals located near your destination should an emergency arise.
Carrying twins or more? Your health care provider might recommend you stop traveling earlier due to the higher risk of complications.
Third trimester
How late in pregnancy can you fly? If you're relatively healthy—and not at risk of complications like preterm labor, preeclampsia, gestational diabetes, or placenta previa—then you're usually OK to travel up until 36 weeks, though some OB-GYNs may prefer you stay closer to your home near the end should you encounter any complications or in case your baby comes sooner than expected.
High-risk patients—and especially those with pregnancy-induced hypertension, diabetes, and sickle-cell disease—may be advised not to fly after 24 weeks—or not at all.
Check with your doctor before traveling at the end of your pregnancy.
Related Articles
What to expect when traveling in each trimester of pregnancy

So you're pregnant? Congrats! It's an exciting time but also one in which many aspects of your life will begin to change, including travel. While you'll quickly need to understand the airline industry's rules for flying while pregnant , there are some more personal tips I'd like to share with you based on my experience traveling throughout the first, second and third trimesters of both of my pregnancies.
A few truths about pregnancy
Picky, starving moms need to travel with snacks.
I didn't know I was pregnant when I took the first flight of my second pregnancy. I was on a mileage run from Houston to Los Angeles, and by the time we landed, I was super tired, kinda grumpy and oh-my-so-hungry.
Then began a mad search for food. Luckily, Counter Burger was open and serving up sweet potato fries and burgers. Out of habit, I went for the veggie burger but I quickly regretted my decision, which left me far from satisfied with ground-up veggie mush.
In the early stages of pregnancy, your normal travel habits of going a little hungry for a while, or making due with what's around, may not work well.
Throughout your pregnancy, travel with water to stay hydrated and snacks to stave off hunger pangs and keep you going through travel delays. If you're feeling particularly food sensitive, research the food options at your destination ahead of time. I virtually lived on chicken noodle soup for a whole week early in my pregnancy and then, for a couple of days, all I wanted were hush puppies. I know how to get those items at home but when you are on the road, you either need to do more research or be more flexible -- which is sometimes easier said than done.
Related: 4 tips for planning travel while planning a pregnancy
Research and make choices about inflight radiation and other risks
I'm not an expert, but because I fly often, I have given some thought to inflight radiation exposure , especially during the early stages of pregnancy.
For pregnant flight attendants and pilots, the Federal Aviation Administration recommends a limit of 1 mSv during pregnancy, with no more than 0.5 mSv per month. I don't fly as much as an airline employee, but it doesn't take much research to learn that the amount of radiation you (and your gestating baby) are exposed to in the air varies dramatically from route to route. The highest-level routes are typically longer, higher-altitude polar routes. Here's some information from NASA about polar flights and radiation .
Every expectant mother should discuss the risks of flying during pregnancy with her doctor before getting on a plane. For me, nine months was a tiny moment in my traveling life, so I was OK adjusting my behavior a bit out of an abundance of caution. However, I didn't adjust to the point of never leaving my house. We still flew when I was pregnant, but I was judicious about when and where I would fly.
Check your health insurance policy
If you aren't familiar with your medical insurance coverage for when you travel, brush up on those facts now. Look at in-network and out-of-network benefits, as well as coverage for procedures for medical emergencies in other countries, if relevant. Most likely, if you do have coverage for treatment in other countries, you will still be on the hook to pay for your care up front and then submit for reimbursement from your health insurer. Plan accordingly and plan for the unexpected. If your baby decides to arrive early, for instance, check to make sure your insurance would cover possible extended and expensive care in an intensive care unit in a hospital away from your home.
Be sure to check what your health insurance coverage provides if you deliver at another facility later in your pregnancy. I once had an insurance plan that specifically did not cover out-of-network deliveries after 36 weeks, so that is something you would want to know before venturing away from home late in pregnancy.
Consider travel insurance
Trip insurance can be helpful if you are traveling while pregnant. Read the plan's fine print to determine what might be covered and whether you are covered if you already knew you were pregnant when you purchased the plan. Typically, a normal pregnancy or normal delivery would not be covered but if there are unexpected complications with the pregnancy, then related trip-cancellation or trip-interruption coverage may kick in on certain plans in certain situations.
Here are some travel insurance providers to check out: Allianz Travel Insurance, Travel Guard and Travelex Insurance . You can also compare a variety of plans at a portal like SquareMouth .
Here are some articles that will help you brush up on your travel insurance knowledge:
- The best travel insurance policies and providers
- What is independent travel insurance and when is it worth it?
- When to buy travel insurance versus when to rely on credit card protections
- Is credit card travel insurance sufficient on its own?
- Why I buy travel insurance
Traveling in the first trimester
Traveling in the first trimester can range from "no big deal" to "I think I'm going to die from misery right this very instant." Symptoms in early pregnancy can vary widely and can change by the day. A flight in your first trimester may be no different from any other flight you've ever taken or it may feel like you are flying with the worst hangover of your life.
Unless you are very high risk or have other extenuating medical issues, your doctor will probably give you the green light to travel in early pregnancy. Feeling extra tired, nauseous and queasy doesn't make for the perfect travel experience, so here are some tips to make travel easier:
Pick an aisle seat and move about the cabin
When you do hit the skies early on, choose a seat where you will be the most comfortable, likely an aisle seat so you can get to the restroom easily. I also recommend getting up to walk around and stretch your legs. (Here are tips for credit cards that will defeat basic economy and let you get a seat assignment in advance.)
Room service come to the rescue
In my first trimester of my second pregnancy, I went on a trip with my daughter and parents to New York City to see the Macy's Thanksgiving Day Parade and I was met with another challenge. I was at the point in my pregnancy when I needed food immediately upon waking or I was going to get queasy. Since I was staying in a hotel room with my young daughter, this meant room service. I also had granola bars and fruit on hand, but that was not enough to really do the trick some mornings. Had my husband been there, he could have gone in search of a warm bagel and juice, but since he wasn't on this trip, we had to improvise. Thanks goodness Marriott elite status helped defray the cost of most of the breakfast!

Take it easy when you need to
Once you are further along in your pregnancy and you actually look pregnant, you will sometimes get a little sympathy or, at least, empathy while traveling. Strangers may offer to help with your bag and people may have more patience with you if you're moving slowly. However, in the first trimester nobody can tell you are pregnant, and no one is going to feel sorry for you. If you act queasy on the plane, you will pretty much be treated like you have Ebola, and any other issue or ailment will pretty much not interest anyone. I once told the flight attendant I was pregnant when she was giving me the eye about looking queasy.
Take care of yourself, don't overdo it and know when to say enough is enough. You may be used to very busy travel days, but now find yourself needing a nap during your first trimester, and that's OK. Listen to your body and adjust accordingly.
Traveling in the second trimester
You have probably heard that the second trimester is generally the easiest of the three trimesters for most expecting moms. You usually aren't as sick and or as tired as in the first trimester, and you aren't as large, uncomfortable and exhausted as in the third trimester. From roughly weeks 13 to 27 of a pregnancy, your activity and comfort levels are often good, and this means that it can be a great time to travel. Couples that like to take "babymoons" (one last couples trip before the baby arrives) often try to schedule them in the second trimester.
Related: The best babymoon destinations for every month of the year
The beginning and end of the second trimester are quite different
You will probably enter the second trimester not really looking pregnant, and end it looking quite different. This means that you may feel very different at the beginning and end of the second trimester. The second trimester is when lots of belly growing happens and this can mean that some types of travel will be more uncomfortable toward the end of these few months of pregnancy than at the beginning.

Consider where you are comfortable traveling
A very personal and important decision to make during the second trimester is to determine if there are certain restrictions you will place on yourself in terms of where you're comfortable traveling. Some types of travel will ban women from traveling during the second trimester. For example, many cruise lines will not allow a woman to book a cruise if she will enter her 24th week of pregnancy (or later) while on the voyage.
Royal Caribbean's policy bars pregnant women from sailing at and after the 24th week. It was developed in concert with the Cruise Lines International Association endorsement of the American College of Emergency Physicians Health Care Guidelines for Cruise Ship Medical Facilities .
Many consider unborn fetuses to be viable if born beginning around 24 weeks (though that age threshold is getting earlier and earlier). This means that a baby born at 24 weeks gestation would have anywhere from a 50% to 70% chance of survival outside the womb if (and only if) there is immediate access to advanced medical care. A cruise ship clearly doesn't have an advanced neonatal care unit on board, so presumably the policy is related to why cruise lines draw the line for pregnant passengers.
I personally draw the line for travel at 23 or 24 weeks when talking about destinations that don't have the same level of advanced medical care as the United States -- or long flights or a flight path that could hinder prompt access to advanced medical care if I happened to unexpectedly go into labor. The Maldives is an example of somewhere I would not want to travel in this instance because there would be significant delays in obtaining medical care on these remote islands.
Plan big, but not too big
The second trimester is a great time to squeeze in a pre-baby trip or two since you will probably feel relatively like to your pre-pregnant self much of the time. We went to Aruba when I was 14 weeks pregnant and it was a fantastic trip. I had lots of energy and a normal appetite. Flying was not uncomfortable because my belly was still pretty small and the only real adjustment was to make sure I had a somewhat larger bathing suit before the trip.
At 23 weeks, I traveled to Spain and still felt pretty energetic and "normal." I will admit that the flight in economy wasn't super comfortable since I did have a belly that was hindering curling up in positions that usually help me sleep on the plane, but our time on the ground in Spain wasn't really impacted at all by the pregnancy other than missing out on the Spanish wine.
The great thing about both of those trips was that they were at my own pace. This meant that if I didn't feel like doing much one afternoon, I could take it easy. Even though you may feel great in the second trimester, you can still tire more quickly than normal, so be sure to limit your vacation activities to those you can manage. There are also activities that some doctors might advise against by the second trimester like thrill rides, scuba diving or horseback riding, so double-check any restrictions before planning more adventurous outings.

Traveling in the third trimester
Pregnancy isn't an illness or disease. For many families, it's just a normal phase in a woman's life before a new baby joins the family. Assuming things are going well, it's not a time when you have to cancel all travel. However, once the third trimester rolls around, travel can get a more complicated and does eventually have to stop.
The beginning and end of the third trimester are quite different
Changes come even more quickly in the third trimester. You enter the third trimester about 28 weeks pregnant and end it with a newborn. This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant.
Select destinations and activities carefully
In the final months of pregnancy, some activities are probably going to be more comfortable and enjoyable than others. For example, swimming and spa time may be exactly what you need.
I give strong preference to visiting beach and resort destinations in the final trimester. Trust me when I say that few activities are as comfortable in the third trimester as floating in the water! We went to The Phoenician (a Marriott property) in Scottsdale, Arizona, when I was about 31 weeks pregnant and even with my big belly, it was the perfect mix of spa, swimming and fun activities for our 5 year old before both our lives changed.

You are going to get uncomfortable
Maybe this isn't universal and there are some magical creatures out there who never feel uncomfortable during pregnancy, but every mom I know eventually hit a point in her pregnancy when she wasn't comfortable. For many, this means that sitting for an extended time in a small airline seat, standing in long lines or trekking around in the heat to explore a city all day eventually become pretty miserable activities.
No one can tell you when you will hit that point, but it will likely happen in the third trimester. For me, my back started giving me a bunch of trouble at around week 30 or 31. I was incredibly grateful there were no more flights scheduled during that pregnancy beyond that point.
If you are going to fly during the later weeks of your third trimester and have the ability to secure a more comfortable seat up front, or at least one with extra legroom so you can stretch out, it may well be a good investment in your comfort. I brought a tennis ball with me when I flew so I could give myself a bit of a "back massage" against the airplane seat.

Bring your own pillows
Sleep becomes a challenge in the third trimester for many women and a pillow fort of sorts becomes a necessity to get some good shut-eye. Many pregnant moms find that using some sort of body pillow or pillow arrangement helps to keep their bellies supported and comfortable at night. You can't assume that the hotel will have similar pillows, so bring your own if they become essential to good rest in your third trimester. I had no shame in hauling my pillow fort with me on our last road trip at eight months pregnant.
See if you are allowed to fly
Even if your doctor OKs it, many airlines have rules about women flying in the third trimester. Check out airline rules for traveling while pregnant for complete details, but generally speaking, most U.S. airlines don't have many flight restrictions until the last month of pregnancy. However, many international airlines do have restrictions and documentation requirements beginning at 28 weeks. If you are pregnant with more than one baby, the restrictions kick in even earlier.
Decide when to stop traveling
I'm all for traveling while pregnant but, realistically, most women will want to stop traveling at some point in the third trimester. I would imagine by about 36 or 37 weeks, most women will probably decide to stay closer to home. I went on a road trip about three hours from home at 35 weeks and then called it quits for the rest of the pregnancy. There's still a whole new world of travel waiting once a new baby joins the family .

Bottom line
There is usually no reason to stop traveling when you're expecting. During my last pregnancy, I went on 12 trips, 28 flights, visited four countries and I'm very glad I had the opportunity to stay that active. I'm also glad that I grounded myself from flight after 31 weeks and from road trips at 35 weeks because those were the right decisions for my comfort level.
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours
Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane
- Tips for healthy travel
Ready Steady Baby
Travelling when pregnant.
Whether you’re doing short journeys in the car or getting on a plane for a holiday abroad, it’s important to take extra care of yourself when you’re pregnant. Making a few small changes and planning ahead will help to make sure you have a comfortable and safe journey.
Wherever you’re going, it’s a good idea to take your maternity notes with you in case you need medical help.

It’s fine to drive or be a passenger in a car while you’re pregnant.
It’s important to wear a seat belt as you normally would. Make sure the straps don’t go over your bump by:
- placing the lap strap across your hips so it fits comfortably under your bump
- placing the diagonal strap between your breasts and around your bump
Take regular breaks when driving and make sure you bring some water and snacks with you for the journey.
Going on holiday or abroad
If you’re planning a holiday, seek health advice as early as possible.
You should give some thought to where you want to go as:
- the things you may normally love, like hot sunny weather, may not be a great idea if you’re uncomfortable or finding it hard to sleep
- you shouldn’t travel to areas where there’s malaria or the Zika virus if you can avoid it
You should also consider the quality of medical care in the country you plan to visit.
Fitfortravel has more advice for pregnant travellers
Staying safe on holiday
Activities like walking and swimming are fine while you’re pregnant, but it’s not a good idea to do any activity where you might fall.
Take care to avoid coming into contact with water or food that could cause tummy upsets. Some medicines for treating diarrhoea may not be suitable in pregnancy.
Talk to your midwife if you have questions.
Travel vaccinations
You’ll need vaccinations before you travel to certain countries.
There are some vaccinations you shouldn’t have when you’re pregnant, especially in the first 3 months, so always check before you book anything.
Find out which travel vaccinations you might need
Travel insurance
Before you travel, you’ll need special travel insurance that:
- covers any medical costs
- allows you to cancel for any issues with your pregnancy
If you don’t tell your insurer you’re pregnant before you travel, your insurance may not be valid.
If you’re travelling in Europe, the European Health Insurance Card (EHIC) may allow you to use the health services in these countries.
Apply for a European Health Insurance Card
Flying while pregnant
Air travel is generally safe if you’re having an uncomplicated pregnancy.
If you have any pregnancy complications, check with your midwife or GP that there’s no medical reason to stop you flying, such as high blood pressure or a risk of deep vein thrombosis .
Most airlines won’t let you fly if you’re within about a month of your due date. Some will need a letter from your GP or midwife saying you’re fit to fly when you’re 7 months pregnant. Check with the airline before you book.
Having a comfortable flight
When travelling by plane:
- drink plenty of water as you’re much more likely to get dehydration while flying.
- take healthy snacks with you so you can follow your own eating plan
- take whatever makes you more comfortable, such as an extra pillow or warm socks
Be aware it may take you a bit longer than before to recover from jet lag.
Deep vein thrombosis
Deep vein thrombosis (DVT) is a blood clot in a deep vein in your leg, calf or pelvis.
You’re more likely to get DVT if:
- you sit for long periods of time
- do very little activity
If you’re travelling on a long-distance flight or sitting for 4 hours or more, talk to your midwife as you may need medication. F ollow your midwife or doctor’s advice.
More about deep vein thrombosis
Further information, other languages and alternative formats
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 14 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
- Travel health and vaccinations
Other health sites
- fitfortravel: Advice for pregnant women
- Institute for Health Visiting: Travelling with your baby
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)
Natasha was diagnosed with cancer when she was 22 weeks pregnant
By Jo Abi | 4 days ago
Natasha Strapps was young and in love when she received devastating news .
The Adelaide woman was 22 weeks pregnant with her first child when she began feeling short of breath.
"To me, I felt like I only had two to four weeks of being happy ," Strapps, 26, tells 9honey
READ MORE: Meghan Gale announces major comeback

"I had what we thought was a virus or a chest infection," she recalls.
"I had this terrible cough and just had no energy whatsoever."
Multiple courses of antibiotics failed to alleviate her symptoms.
After two weeks in bed and a month of feeling unwell, Strapps tried to return to work but couldn't manage it.
READ MORE: 'It started with brain fog': Before long she was struggling to talk

She rang Josh crying and he told her to go to the hospital.
"I'm like, 'That's a bit excessive'."
She was seen quickly due to her pregnancy and was initially told she had "atypical pneumonia."

"I started on IV antibiotics for three or four days, and I told them that it wasn't doing anything," she says.
"They said that I was just presenting fine. Because I'm quite a bubbly person even when I'm not at my best, you wouldn't know I'm not at my best, I guess."
A lung specialist was called in to see Strapps and he was immediately concerned, sending her for a CT scan.
READ MORE: Our guide to the mattress toppers to match your sleeping needs

"They found a large mass in my chest," she says.
Further testing would confirm Hodgkin's Lymphoma.
Strapps was in the maternity ward when she was told of her diagnosis, and her immediate concern was for her unborn child.
"The night that I found out it was cancer, hearing the other babies cry, I just held onto my belly and cried because I was like, 'Is this the end?'"

Josh told her she had to come first but they were both relieved when they were told they would be able to treat her during her pregnancy.
Strapps was diagnosed on May 31 and began chemotherapy on June 5.
"There was a sense of urgency that I needed to start treatment because the mass was quite large," she says.
"It was over 15 centimetres in my chest, which is fairly excessive, and close to my heart."
For a daily dose of 9honey, subscribe to our newsletter here .

After seven sessions of chemotherapy during pregnancy, Strapps and Josh welcomed their daughter via emergency caesarean and a week later she was back to treatment.
"I had to finish my cycle, I think it was 12 chemotherapy treatments all up as part of that regime," she says.
Strapps did her best to juggle her treatment and new motherhood. Daughter Mia, now 11 months old, was a "great sleeper", which helped.
"I had a stem cell transplant in June and had my final scan to see where we're at," she explains.

Following the scan, she was told she is "now officially in remission",although she remains cautious.
"It's still not guaranteed. You can still relapse after."
September is Blood Cancer Awareness Month . Find out more at the Leukaemia Foundation Australia website .
FOLLOW US ON WHATSAPP HERE : Stay across all the latest in celebrity, lifestyle and opinion via our WhatsApp channel. No comments, no algorithm and nobody can see your private details.
- Womens Health
- Pregnancy And Fertility
Auto news : Toyota's first car mysteriously vanished.

All the celebrities spotted at the Sydney Spring Racing Carnival

Keanu Reeves' life and career in pictures

AI and humanoid tutors set to transform Aussie education
COMMENTS
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
The best time to travel is mid-pregnancy (14 to 28 weeks). During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily. ... Trimesters: The 3-month periods of time in pregnancy. They are referred to as first, second, or third. Zika: A disease caused by the Zika virus, which is ...
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
Most airlines do allow pregnant women to fly until about a month before their due dates. Chervenak agrees: "As long as there are no known complications to pregnancy, traveling on an airplane is ...
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
Flying while pregnant is perfectly safe. The real reason that airlines put restrictions on flying while pregnant is because they are afraid you will give birth in the air. Thus, a lot of airlines won't let pregnant women fly after 36 weeks (or 32 weeks if you are having multiples).
In general, most airlines won't allow you to fly in your last month of pregnancy, though some limit travel as early as 28 or 29 weeks of pregnancy. And international flights often have an ...
After 37 weeks, pregnant women will not be allowed to travel. For multiple pregnancies, a certificate is required between the 29th and 32nd week; after that, women will not be allowed to travel. The medical certificate must include the following: Be issued and signed by a doctor or midwife.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months. Flying in pregnancy. Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
Dr. Gaither says pregnant travelers should stop "at least every two hours" and get out of the car, stretch, and walk around. This increases blood flow to the lower body which helps prevent ...
Answer From Mary Marnach, M.D. Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy ...
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
She recommends taking plenty of walking breaks since "pregnant women are at higher risk for blood clots and prolonged sitting increases that risk." You should try to get up and walk for five to 10 ...
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor.
If you are enjoying a healthy pregnancy, plane travel is likely to be safe. The second trimester is probably the best time to fly. You're likely to be over morning sickness.Later, your expanding ...
As a general rule of thumb, most airlines will allow pregnant people to fly right up until week 36 of pregnancy, but you should absolutely do your research before booking your flight to check ...
This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant. Select destinations and activities carefully. In the final months of pregnancy, some activities are probably going to be more comfortable and enjoyable than others.
You should avoid travelling to an altitude above 3,658 metres (12,000 feet). However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet). If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
But there's an additional consideration, particularly if you are close to your due date: In early 2020, the U.S. State Department (DOS) issued a major amendment to its regulations, restricting the ability of pregnant women to obtain B-2 tourist visas for travel to the United States. The idea is to prevent "birth tourism," or the practice of ...
Travel vaccinations. You'll need vaccinations before you travel to certain countries. There are some vaccinations you shouldn't have when you're pregnant, especially in the first 3 months, so always check before you book anything. Find out which travel vaccinations you might need. Travel insurance
By 6 months, your baby has fully formed lungs and a unique set of fingerprints, and they're beginning to focus on sounds outside the uterus (like you and your partner talking). They're also ...
After two weeks in bed and a month of feeling unwell, Strapps tried to return to work but couldn't manage it. ... The Adelaide local was 22 weeks pregnant and newly engaged when a diagnosis turned ...
In a risk free pregnancy you can fly until the 36week. That's what doctors recommend and the airlines as well. Actually most of the airlines won't let you fly if you are 36+ weeks. I flew when I was 23-24 weeks ~ 6 months and that was ok. I also went to visit my family and it was a 3h flight.