- About Founder
- News & Press
- See Our Reviews
- HONcode Certification
- HIPAA Compliance & Security
- Editorial Guidelines
- Sponsor Program
- Privacy Policy
- Terms & Conditions
- Adam's Book
- Hats & Fun Stuff
- About Community
- Patient News Feed
- Success Stories
- Adam's Blog

LEARNING CENTER
- Heart Valve News Feed
- Atrial Fibrillation
- Free Educational eBooks
- Medtronic Low-Risk TAVR
SURGEON FINDER
- Featured Surgeon
- Recommend Surgeon
HEART HOSPITALS
Adam's blog.
- About Adam Pick
Traveling Timeline After Heart Surgery
By Adam Pick on November 25, 2013
Travel during the holiday season is expected to increase this year, up from the 93.3 million travelers who ventured at least 50 miles away from home this time last year, according to AAA. Although many medical professionals recommend avoiding traveling during recovery, it seems practically unavoidable during this family-centered season. However, just because you might be going against this advice, it doesn’t mean you should throw all caution to the wind. These tips break down some important considerations for traveling after heart surgery.

The National Health Service recommends checking with your airline BEFORE flying, since companies have varying regulations on post-surgery travelers. However, the Civilian Aviation Authority says that 10 to 14 days is sufficient after chest surgery or a coronary artery bypass graft. After any heart operation, patients should remain moderately active to keep the heart pumping. Avoid tight clothing to prevent circulation inhibition as well.
During your early recovery, you’ll want to maintain only moderate activity at your destination. If your destination is the Midwest, consider staying at Wisconsin Dells resorts to take advantage of spas and other relaxation-enhancing amenities. In warmer weather conditions, swimming can also be a fun, light activity to stay active and cool.
Three months
At this point, you may be close to a full recovery but not quite there yet. (Hopefully, you will have taken my advice and attended a great cardiac rehab program.) Mostly, you’ll want to make sure to avoid overworking your heart. Get a full examination — BEFORE your trip — so your doctor can alert you of specific things to look out for. Taking medication like Dramamine isn’t recommended for flying, since you may sleep in a circulation-cutting position for an extended period of time. If you get nervous on airplanes or other forms of transportation, consider anti-anxiety medication instead, so you can keep your heart rate low without compromising your circulation.
Since being active can be difficult in an airplane, request to sit either in the very front or very back of the plane, so you can stretch your legs as often as possible. In the meantime, drink plenty of water, since the low humidity on planes increases the risk of dehydration.
Traveling itself may only come with minor considerations at this stage, such as staying hydrated and active. However, you’ll want to keep a close eye on your diet once you reach your destination. Especially during the holiday season, many people indulge in sugar-filled, high-fat foods. The American Heart Association recommends having less than 7 percent of saturated fat out of your total daily calories. Trans fats should comprise less than 1 percent of your daily intake, while cholesterol should never exceed 300 mg. The best way to reduce your saturated and trans fats intake is to reduce the amount of butter or margarine added to your food when cooking. Trim fat off of your meat or choose lean meats with under 10 percent fat to further cut back.
Right about this time… I traveled to Hawaii with Robyn, my wife, to celebrate my recovery. It was an amazing trip (see picture below).

At 10 months post-op, I went on a two-week business trip through five cities in Europe. During the trip, I had some chest pain — from the lifting and the moving of luggage in awkward positions — so I carried a bottle of Ibuprofen with me at all times to help ease the discomfort.
At the one year mark, many patients have reached full recovery status. Still, it’s always important to continue taking precautions when traveling. Make sure your travel insurance is up to date, since recent surgeries can often raise rates or lead to a higher copay. Access to medical care is highly important when you’re away from home, so feel free to check in with a doctor if anything feels abnormal.
I hope this timeline helps you plan your travel after heart surgery.
Keep on tickin! Adam
- Leave a Comment
- See 12 Comments
Written by Adam Pick - Patient & Website Founder

Adam Pick is a heart valve patient and author of The Patient's Guide To Heart Valve Surgery. In 2006, Adam founded HeartValveSurgery.com to educate and empower patients. This award-winning website has helped over 10 million people fight heart valve disease. Adam has been featured by the American Heart Association and Medical News Today.
12 Comments ... Click here to add one .
Name (required)
E-Mail Address (will not be published) (required)
Submit Comment
Adam's Newest Blogs
Adam's newest posts.

Patient Webinar: Ask Dr. Gerdisch Anything!

Patient Update: Koert Travels from California to New York for a Ross Procedure by Dr. Paul Stelzer
New Community Posts

Dennis says, "Past six months post surgery! Cardiac..."

Tim says, "Kevin did you have your chest wired back..."
Blog Categories
Adam's blog categories.
- Adam's Updates
- Aortic Stenosis
- Aortic Valve Repair
- Aortic Valve Replacement
- Before Surgery
- Bicuspid Aortic Valve
- Heart Valve Replacement
- Medical Technology
- Mitral Regurgitation
- Mitral Valve Repair
- Patient Stories
- Ross Procedure
- Surgeons & Hospitals
- Tricuspid Valve
Surgeon Spotlight
Dr. Marc Gerdisch is a heart valve expert having performed over 4,000 heart valve repair and replacement operations during his career.
See Patient Reviews
Heart Hospital Map

Search for heart hospitals that specialize in heart valve treatment.
See Hospital Map
New Posts From Our Community
Newest community post.
Dennis Shaffer from Texas says
Past six months post surgery! Cardiac rehab is in the rear view and I
Meet Dennis
Dennis says, "Past six months post surgery! Cardiac" Dennis's Journal

Tim Carpenter from Bellevue says
Kevin did you have your chest wired back together after surgery or did
Tim says, "Kevin did you have your chest wired back" Tim's Journal

Kevin McCarthy from Arlington, Massachusetts says
Day: 7 The big things are going well, the small things are
Kevin says, "Day: 7 The big things are going" Kevin's Journal

Find Heart Valve Surgeons
Search 1,500 patient-recommended surgeons
The Patient's Guide

This book has helped over 47,000 patients and caregivers from diagnosis to recovery.
Heart Valve Hospitals
Search Heart Hospitals Search Hospitals
- Patient Care & Health Information
- Tests & Procedures
- Coronary artery bypass surgery
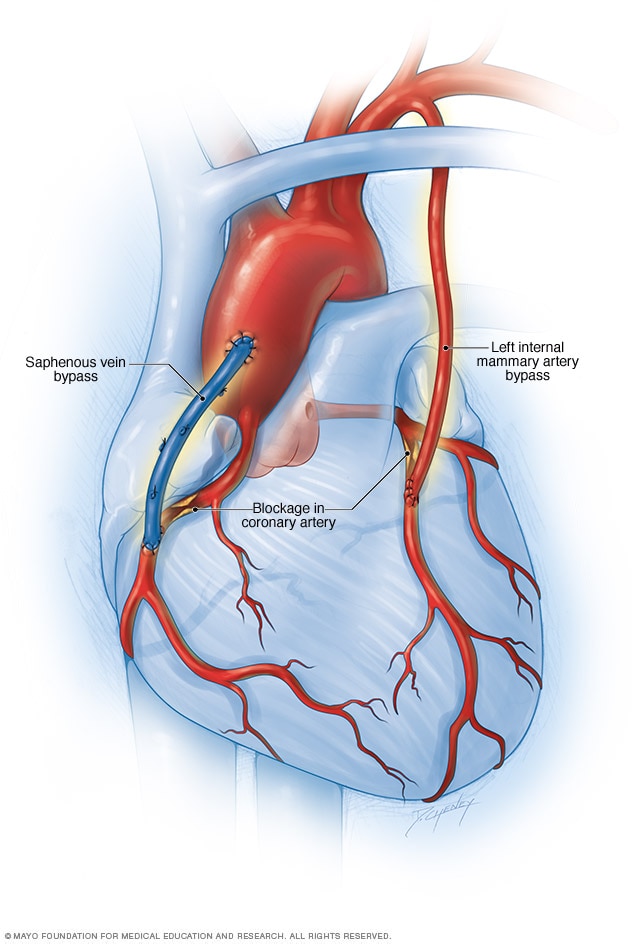
Coronary artery bypass surgery creates a new path for blood to flow to the heart. A healthy blood vessel from another part of the body is used to redirect blood around a blocked area of an artery. Usually the blood vessel is taken from an artery in the chest, called the internal mammary artery. Sometimes it's taken from a leg vein, called the saphenus vein.
Coronary artery bypass surgery creates a new path for blood to flow around a blocked or partially blocked artery in the heart. The surgery involves taking a healthy blood vessel from the chest or leg area. The vessel is connected below the blocked heart artery. The new pathway improves blood flow to the heart muscle.
Other names for this surgery are:
- Coronary artery bypass grafting.
- CABG — pronounced "cabbage."
- Coronary artery bypass graft surgery.
- Heart bypass surgery.
Coronary artery bypass surgery doesn't cure the heart disease that caused a blockage, such as atherosclerosis or coronary artery disease. But it can reduce symptoms such as chest pain and shortness of breath. The surgery, commonly called CABG, may reduce the risk of heart disease-related death.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Coronary artery bypass surgery is done to restore blood flow around a blocked heart artery. The surgery may be done as an emergency treatment for a heart attack, if other immediate treatments aren't working.
Your health care provider might recommend coronary artery bypass surgery if you have:
- A blockage in the left main heart artery. This artery supplies a lot of blood to the heart muscle.
- Severe narrowing of the main heart artery.
- Severe chest pain caused by narrowing of several heart arteries. The narrowing reduces blood flow to the heart even during light exercise or at rest.
- More than one diseased heart artery and your lower left heart chamber doesn't work well.
- A blocked heart artery that can't be treated with coronary angioplasty. This less-invasive treatment uses a balloon on the tip of a thin tube, called a catheter, to widen the artery. A small coil called a stent is typically used to keep the artery open.
- An angioplasty with or without a stent that hasn't worked. For example, an artery narrowed again after stenting.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Coronary artery bypass surgery is open-heart surgery. All surgeries have some risks. Possible complications of coronary artery bypass surgery include:
- Heart attack due to a blood clot after surgery.
- Infection at the site of the chest wound.
- Long-term need for a breathing machine.
- Irregular heart rhythms, called arrhythmias.
- Kidney problems.
- Memory loss or trouble thinking clearly, which often is temporary.
The risk of complications is higher if the surgery is done as an emergency procedure.
Your specific risk of complications after coronary artery bypass surgery also depends on your overall health before surgery. Having the following medical conditions increases the risk of complications:
- Blocked arteries in the legs.
- Chronic obstructive pulmonary disease (COPD).
- Kidney disease.
Medicines to control bleeding and blood pressure and to prevent infection are typically given before surgery to reduce the risk of complications. If you have diabetes, you may get medicine to control blood sugar during surgery.
How you prepare
Before coronary artery bypass surgery, you may need to make changes to your activities, diet and medicines. Your health care provider gives you specific instructions.
Arrange for someone to drive you home after your hospital stay. Also make plans to have help at home during your recovery.
What you can expect
Before the procedure.
If coronary artery bypass surgery is a scheduled procedure, you are usually admitted to the hospital the morning of the surgery. You have many heart tests and blood tests the days and hours before surgery.
During the procedure
Coronary artery bypass surgery is major surgery that's done in a hospital. Doctors trained in heart surgery, called cardiovascular surgeons, do the surgery. Heart doctors, called cardiologists, and a team of other providers help care for you.
Before you go into the operating room, a health care provider inserts an IV into your forearm or hand and gives you medicine called a sedative to help you relax.
When you are in the operating room, you can expect these things:
- Anesthetics. You receive a combination of medicines through the IV and a face mask. These medicines put you in a pain-free, sleep-like state. This is called general anesthesia.
- Breathing machine. A care provider inserts a breathing tube into your mouth. This tube attaches to a breathing machine called a ventilator. The machine breathes for you during and immediately after the surgery.
- Heart-lung machine. During surgery, a heart-lung machine keeps blood and oxygen flowing through your body. This is called on-pump coronary bypass.
Coronary artery bypass surgery usually takes about 3 to 6 hours. How long surgery takes depends on how many arteries are blocked.
A surgeon typically makes a long cut down the center of the chest along the breastbone. The surgeon spreads open the rib cage to show the heart. After the chest is opened, the heart is temporarily stopped with medicine. The heart-lung machine is turned on.
The surgeon removes a section of healthy blood vessel, often from inside the chest wall or from the lower leg. This piece of healthy tissue is called a graft. The surgeon attaches the ends of the graft below the blocked heart artery. This creates a new pathway for blood to flow around a blockage. More than one graft may be used during coronary artery bypass surgery.
Some variations of coronary artery bypass surgery include:
- Off-pump or beating-heart surgery. Sometimes a heart-lung machine is not used during coronary artery bypass surgery. Instead the surgery is done on the beating heart. Special equipment stabilizes the specific area of the heart being operated on. This type of surgery can be challenging because the rest of the heart is still moving. It's not an option for everyone.
- Minimally invasive surgery. A heart surgeon does the surgery through small cuts in the chest. Minimally invasive heart surgery might be called port-access or keyhole surgery.
After the surgery is done, the health care providers restore your heartbeat in the operating room and stop the heart-lung machine. The surgeon uses wire to close the chest bone. The wire stays in your body after the bone heals.
After the procedure
After coronary artery bypass surgery, a team of health care providers checks on you and makes sure you are as comfortable as possible. You may feel sore and confused when you wake up. You can usually expect the following:
- Breathing tube. The breathing tube stays in your throat until you wake up and can breathe on your own.
- Hospital stay. Expect to spend 1 to 2 days in a hospital intensive care unit. The length of your entire hospital stay depends on how you recover and if you have complications. Some people who have coronary artery bypass surgery go home within a week.
- Heart rhythm and breathing checks. Your health care team watches you closely after surgery to check for complications. Machines record your breathing and heart rhythm. You have frequent temperature checks.
- Medicines. Medicines are given to you by IV to reduce pain and prevent complications such as blood clots. If you don't already take a daily aspirin, your health care provider may recommend you do so. You may need to take the aspirin every day for life. There are specific medical recommendations about who benefits from aspirin therapy. Talk to your health care provider about aspirin use.
- Cardiac rehabilitation. Often called cardiac rehab, this supervised program of education, counseling and exercise helps improve heart health after heart surgery. You'll be encouraged to start moving and walking while you're still in the hospital. When you go home, you continue a cardiac rehab program at a medical center until you can safely follow a home program.
After surgery and when you're at home, you need to watch for symptoms of complications. Call your health care provider if you have:
- Rapid heart rate.
- New or worsened pain around your chest wound.
- A change in skin color around your chest wound.
- Bleeding or other discharge from your chest wound.
It usually takes about 6 to 12 weeks to recover after coronary artery bypass surgery. With your provider's OK, you can usually drive, return to work or the gym, and resume sexual activity after 4 to 6 weeks. But everyone recovers differently. Ask your health care provider for guidance.
After recovering from coronary artery bypass surgery, most people feel better. Some people remain symptom-free for many years. But the graft or other arteries may become clogged in the future. If this happens, you might need another surgery or procedure.
Your results and long-term outcome depend on how well you control blood pressure and cholesterol levels and chronic conditions such as diabetes. It's important to take your medicines as directed.
You can manage and even improve your heart health by making lifestyle changes. Try these recommended steps:
- Don't smoke. Smoking is a major risk factor for heart disease, especially atherosclerosis. Quitting is the best way to reduce the risk of heart disease and its complications. If you need help quitting, talk to your provider.
- Eat healthy foods. Choose plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats.
- Manage weight. Being overweight increases the risk of heart disease. Ask your provider what a healthy weight is for you.
- Exercise. Regular exercise helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. After coronary artery bypass surgery, your provider will tell you when it's safe to begin exercising again.
- Manage stress. Find ways to help reduce emotional stress. Practicing mindfulness and connecting with others in support groups might be helpful. If you have anxiety or depression, talk to your provider about strategies to help.
- Get good sleep. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Coronary artery bypass surgery care at Mayo Clinic
- What is coronary artery bypass grafting? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/coronary-artery-bypass-grafting. Accessed Aug. 31, 2022.
- Choi K, et al. Coronary artery bypass grafting in octogenarians — Risks, outcomes, and trends in 1283 consecutive patients. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2022.03.033.
- Loscalzo J, et al., eds. Ischemic heart disease. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed Aug. 31, 2022.
- Aranki S, et al. Early noncardiac complications of coronary artery bypass graft surgery. https://www.uptodate.com/contents/search. Accessed Aug. 31, 2022.
- AskMayoExpert. Cardiac rehabilitation (adult). Mayo Clinic; 2022.
- Lawton JS, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2022; doi:10.1016/j.jacc.2021.09.006.
- Aranki S, et al. Coronary artery bypass graft surgery: Long-term clinical outcomes. https://www.uptodate.com/contents/search. Accessed Sept. 12, 2022.
- Ami TR. Allscripts EPSi. Mayo Clinic. Aug. 23, 2022.
- Doenst T, et al. PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. Journal of the American College of Cardiology. 2019; doi:10.1016/j.jacc.2018.11.053.
- Bakaeen FG, et al. 2021: The American Association for Thoracic Surgery Expert Consensus Document: Coronary artery bypass grafting in patients with ischemic cardiomyopathy and heart failure. The Journal of Thoracic and Cardiovascular Surgery. 2021; doi:10.1016/j.jtcvs.2021.04.052.
- Lloyd-Jones DM, et al. Life's essential 8: Updating and enhancing the American Heart Association's construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation. 2022; doi:10.1161/CIR.0000000000001078.
- What is CABG? American Heart Association. https://www.heart.org/en/health-topics/consumer-healthcare/answers-by-heart-fact-sheets/answers-by-heart-fact-sheets-treatments-and-tests. Accessed Sept. 12, 2022.
- Mankad R (expert opinion). Mayo Clinic. Oct. 21, 2022.
- Acute coronary syndrome
- Cardiogenic shock
- Coronary artery disease
- Enlarged heart
- Heart arrhythmia
- Heart attack
- Heart disease
- Heart failure
- Myocardial ischemia
- Spontaneous coronary artery dissection (SCAD)
- Sudden cardiac arrest
- Takayasu's arteritis
- Ventricular fibrillation
News from Mayo Clinic
- Mayo Clinic Healthcare expert shares good news and bad news about angina Nov. 01, 2023, 03:00 p.m. CDT
- Coronary artery bypass grafting has potential benefits for patients over age 80 with reasonable surgical risk, Mayo Clinic study finds June 20, 2022, 02:02 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Can You Fly After Open Heart Surgery?

Open heart surgery can be minimally invasive or require a long period of recovery. In any case, you or your loved one will likely be in a more delicate state. This means your normal routine, including work, exercise, activities and travel, may not be feasible for several weeks or more. If you have a trip planned in the near future or had your surgery done in another state, traveling by plane can potentially create health complications.
Flying on a commercial airplane is not always recommended for recovering patients, especially those with conditions like diabetes. If you want to know whether it is safe to travel after heart surgery, consider the potential risks of traveling and alternative modes of long-distance patient transportation that are available.

What Is Open Heart Surgery?

Open heart surgery is an umbrella term people use to describe surgical procedures that treat heart problems. This type of surgery typically involves the heart muscle, arteries, valves, aorta and coronary arteries. Open heart surgery gets its name from the nature of the procedure itself, which often requires surgeons to cut through an individual’s breastbone and spread their ribs to perform surgery on their heart. Typically, individuals with heart problems who do not see improvements with medications, lifestyle changes or other procedures may require open heart surgery.
With open heart surgery, surgeons can access the heart to treat the following conditions :
- Coronary artery disease
- Heart valve disease
- Heart failure
- Thoracic aortic aneurysm
- Congenital heart defects, such as hypoplastic left heart syndrome or arterial septal defect
- Arrhythmias
- Atrial fibrillation
- Coronary artery bypass graft (CABG)
In some cases, an individual’s heart will be stopped during open heart surgery. If so, they are connected to a bypass pump, or heart-lung bypass machine, during the procedure. This machine acts as the heart and lungs during the surgery, moving blood through the body and providing oxygen to the blood.
However, patients who require less invasive surgery with smaller incisions may have the procedure performed while their heart is still beating. This form of surgery requires smaller cuts between the ribs. Some patients may undergo open heart surgery to repair issues from a heart attack, for a heart transplant or for valve replacement. The type of surgery a heart patient has depends on their unique condition or combination of problems.
Complications and Restrictions After Open Heart Surgery
Having a major medical procedure like open heart surgery comes with the potential for complications. It’s important to know that you may be limited or restricted in what you can do as you recover.

- Reactions to anesthesia
- Temporary memory loss
- Signs of inflammation at the incision site
- Damage to the heart, lungs, kidney or liver
- Damage to surrounding blood vessels
- Blood clots that may lead to venous thromboembolism (VTE)
The severity of these risks also depends on the type of heart condition you have and your overall health.
Second, your lifestyle may change during recovery. Depending on the type of surgery you had, you may need to take medication, attend physical therapy, and get plenty of rest as your chest muscles and breastbone heal. This means your typical activities may need to be postponed until you are well enough.
Third, your travel abilities may be limited for several weeks or more. The complications of heart surgery noted above may become a greater risk if you engage in activities that are too strenuous during recovery, such as intense exercise or flying. If you plan on traveling, some airlines may require you to receive a medical clearance certificate from your doctor. This certificate shows that your health care providers “clear” you to participate in certain activities, including flying across long distances.
Your physician or surgeon will assess you via a thorough examination to determine if your condition could worsen by sitting on a plane for several hours. If you have plans to travel after your surgery, it’s important to talk to your doctors about whether you will require medical clearance.
Risks of Flying Too Soon After Open Heart Surgery
Can you fly after heart surgery? Depending on your condition and recovery time, yes. However, being on an airplane for long periods after an invasive surgery can present issues that may have a negative impact on your cardiovascular health, even if you feel OK after surgery. Commercial air travel can be risky for these reasons:

- High altitude: Flying in an airplane may have the same effect on your heart as visiting high-altitude locations. Patients who have certain heart conditions or high blood pressure may be more at risk for complications . Drastic changes in altitude can potentially worsen symptoms of existing heart conditions or lead to other heart events. Being at higher altitudes can put more strain on the heart.
- Low oxygen concentration: Airplanes, which travel at higher altitudes, also have reduced oxygen pressure. Sitting in the airplane cabin for hours means your body may not receive the optimal amount of oxygen, which can pose a risk for those with existing heart conditions like heart disease, CAD and pulmonary hypertension. Because there is less oxygen getting to your lungs on an airplane, your heart has to work even harder to pump blood to the rest of your body.
- Stress or anxiety: It’s common for people to feel general anxiety or stress about flying due to fear of heights or turbulence. Stress or anxiety can make your heart conditions worse or lead to a high heart rate, which may also prolong your recovery process.
- Changes in pressure: Passengers will feel pressure changes as the aircraft cabin altitude increases or decreases. This can cause gas to increase or expand in the body, resulting in pulmonary barotrauma . You may experience chest pain, a bloody nose or shortness or breath, which can lead to serious lung and heart damage if you’re recovering from open heart surgery.
- Dehydration: On long-haul flights, significant changes in fluid balance can occur due to controlled, dry air. Very low humidity can generally lead to faster dehydration, affecting your blood pressure. This can be problematic for those with heart disease, CAD, arrhythmia or heart failure.
- DVT risk: Sitting in a cramped plane cabin requires long periods of immobility and poor circulation. Combined with potential dehydration, you may be at a higher risk of developing a blood clot , which often forms in veins in the legs. This is also known as deep vein thrombosis (DVT). If you have an implanted heart device, artificial heart valve, arrhythmia, CAD or a coronary stent, your risk may be even greater. Blood clots can lead to a stroke or heart attack.
When flying after cardiac surgery, you may experience several of these risks at once, which could worsen the negative effects on your overall health.
Patients Who Are at Higher Risk

Your risk of complications, such as DVT, when flying after heart surgery may be greater if you have certain preexisting conditions like the following:
- Chronic obstructive pulmonary disease (COPD)
- Kidney disease
- Blocked arteries in the legs
- Heart or lung disease
- History of blood clots
- History of DVT
- Being on extended bed rest
- Having a catheter in a large vein
- Recent or current cancer treatment
- Having limited mobility
- Varicose veins
- Use of hormones, such as oral contraceptives or hormone replacement therapy
While some blood clots can dissolve on their own, and travel-related DVT is generally low , some clots can travel to your lungs. This may result in a blockage of blood flow and potentially lead to a pulmonary embolism, which can be fatal.
Your chances of these complications can also depend on your age. For example, older individuals may have a higher risk of developing blood clots than younger patients. People who smoke may also be more likely to experience post-surgical issues. The risks of experiencing complications during open heart surgery may be higher if the procedure is performed during an emergency.
You may receive medication to control your blood pressure or prevent bleeding and infection when flying after open heart surgery. This can reduce your risk of complications.
How Long Do You Have to Wait to Fly After Open Heart Surgery?
How soon after open heart surgery you can fly depends on your doctor’s recommendation about your overall condition and other factors. For example, if you’ve had a minimally invasive cardiac surgery with no complications, you may be able to fly within two to four weeks. For more moderate or intense open heart surgery, such as heart bypass surgery, you may need to wait four to six weeks .
If you had open heart surgery for a serious complication or other conditions that could potentially make certain activities during recovery more risky, you may have to wait six to eight weeks or longer. Every individual is different, but you should expect a minimum of two weeks before you can safely travel long distances. How long you have to wait to fly after open heart surgery also depends on how much you have healed and whether you have conditions that could put more strain on your heart and lungs while flying.
Tips for Traveling on an Air Flight After Cardiac Surgery

If traveling by plane is necessary, there are some ways you can make your trip more comfortable and reduce your risk of DVT and other complications.
- Speak with your doctor: Check that your prescriptions are up to date and that you have enough for your travels. Ask your doctor whether they can provide a letter describing your condition and any medications you currently take, including dosages. Your doctor will likely provide other essential information you need for your flight.
- Check your health insurance: Determine whether you are covered for travel. Some travel insurance policies may cover preexisting conditions like heart disease, but you may have to pay a higher premium. Contact your insurance broker to ensure you have health insurance coverage.
- Bring compression socks: Compression stockings, or high socks that reach just under the knee, can help you avoid blood clots in the legs during prolonged periods of sitting. Compression socks help improve blood circulation and lymphatic drainage in your legs, decrease swelling, and prevent low blood pressure when you stand up after several hours of sitting down.
- Drink plenty of water: Staying hydrated is essential no matter where you are, but it’s especially important during recovery and on a long flight. Because you’re likely to be more dehydrated on an airplane with dry air, be sure to drink plenty of water. Try to avoid coffee, soda, tea and alcohol, as these can dehydrate you more and may interact negatively with your medication.
- Move around often: Though you may not have tons of legroom, try to at least move your legs and feet for a couple of minutes each hour if you’re seated. If possible, walk up and down the aisles or go to the restroom to stretch your legs. Gentle stretching before your flight can also help with improving blood flow.
- Wear comfortable clothes: Wearing breathable, stretchy clothing can make for a better travel experience in general. Women can wear comfortable bras that are not underwired, especially while their breastbone is healing. Wearing tight clothing, like jeans, may restrict your movements on the plane.
- Bring items that increase your comfort: When traveling after heart surgery, you want to have everything you need for a worry-free flight. If you have anxiety about flying, bring headphones, a book or anything that will help make the time go by faster. You may consider getting a breathing pillow for strengthening the diaphragm and supporting optimal diaphragmatic breathing throughout the flight.
- Carry contact numbers: Whether you’re flying with someone else or alone, be sure to have the contact information of a local doctor, surgeon or specialist who knows about your condition and can assist airline employees and medical staff in the event of a complication.
What Are My Options for Flying Before or After Open Heart Surgery?
If you have a severe heart condition and need to travel for surgery or treatment immediately, flying may be your only option. While this is the quickest method, you will need to consider how to safely arrive at your destination before and after your surgery.
If you’re flying on a public commercial flight, you might consider flying with a medical escort . These trained and qualified professionals — who are also called flight nurses or patient escorts — will travel with you to ensure air travel safety. They will also provide any necessary medical care throughout your trip.

Having a medical escort with you can help you feel reassured that you’re doing what you can to mitigate any risks related to your heart condition. Whether you’re traveling short or long distances, a medical escort providing constant medical supervision can bring you peace of mind during emergency or non-emergency situations .
Another alternative is using a mode of private medical transport, like an air ambulance. If your condition is more severe, the risk of you experiencing worsening symptoms or a life-threatening emergency may be greater when flying on a commercial air flight alone. Because commercial flights are not equipped with knowledgeable medical personnel or life-saving equipment, flying in an air ambulance can be a safer way to travel. Private medical transport services can take you safely from bedside to bedside.
Whether you’re traveling to your surgeon or going home post-op, an experienced medical crew will be on board to mitigate health risks and provide medical attention if needed. In an air ambulance, the medical crew can even adjust the cabin pressure to avoid complications. Air ambulances are self-contained critical care units that can keep you comfortable and meet your needs.
Domestic Air Ambulance
International air ambulance, how air ambulances can help.
Air ambulances have the technology and medical devices to safely transport you from point A to point B. If you have a heart condition that requires care along the way, an air ambulance can make your experience more comfortable than a private aircraft.
While traveling with a medical escort on a commercial flight can be a suitable option, those who have more severe conditions or prefer to travel with more reassurance and security may find an air ambulance more ideal. You might also need an air ambulance if you:
- Need transportation to a specialized medical facility that is far away.
- Do not have access to public transportation where you reside.
- Are unable to drive yourself or fly unaccompanied due to your heart condition.
- Are flying with a commercial airline that has restrictions on the type of medication or oxygen container you have.

There are a few types of air ambulances that offer different benefits. A helicopter ambulance is suitable for landing near health care facilities or in remote locations and addressing immediate response situations. Fixed-wing ambulances are larger, faster and more suitable for long-distance travel.
Both types of air ambulances come equipped with specialized medical equipment and supplies, much like you would find in an intensive care unit (ICU). Some of this equipment includes:
- Monitoring devices.
- Life support systems.
- A wide range of medications.
You will also find paramedics, doctors and nurses on board your air ambulance who are prepared to handle critical care situations. If it seems like you or a loved one could benefit from safe, tranquil travel on a private air ambulance, know that providing potentially life-saving care is not the only advantage. Here are some other key benefits of using an air ambulance:

- Time-sensitive transportation: In a life-threatening situation, patients need a rapid response. Air ambulances can get medical teams to the individual for quick transport to a specialized facility that they may not receive in a local hospital. A fast response time with a fully equipped aircraft can improve patient outcomes and the chances of survival and recovery.
- Compassionate care: Medical personnel on air ambulances are highly trained and skilled, but they are also dedicated to helping patients before, during and after transport. Loved ones can also be notified of the patient’s health with updates from multi-lingual specialists for clear and consistent communication.
- Quality aircraft: Air ambulances maintain high safety standards, as they are specifically designed to provide medical care for a wide range of injuries and illnesses. Patients will have access to a comfortable and safe environment with high-quality equipment.
- Efficient accessibility: Whether a patient needs to be moved from a mountain to a medical facility or brought back home safely from a foreign country, air ambulances have the capability to quickly transport patients over long distances and access locations that may be too difficult for ground transportation.
Contact REVA for Smooth, Comfortable Medical Transportation
If you need to travel by plane before or after open heart surgery, know that you have options. REVA offers air ambulance and medical escort services that transport you to your destination to mitigate risk. Our experienced, compassionate professionals can get you where you need to be while enhancing your safety and comfort. From critical in-flight medical care to private ground transportation, it’s our goal to help you or your loved one prevent worsening conditions after major surgery.
Traveling with REVA means you can benefit from all the benefits of a private jet along with the latest medical equipment to give you the care you need while flying. At REVA, we offer both domestic and international air ambulance flights , where our friendly medical crew is ready to help you travel to and from treatment. Contact us today to request a free quote for our air ambulance or medical escort services.


Heart Sisters
For women living with heart disease
How soon are heart patients safely fit to fly?

by Carolyn Thomas ♥ @HeartSisters
Five months after my heart attack, I boarded a plane from the West Coast bound for Rochester, Minnesota. Considering that I’d suffered two terrifying cardiac events on another long flight just five months earlier made this trip just a wee bit scary for me.
Only the reality that I was headed to the world-famous Mayo Clinic helped to propel me onboard. I told myself that if anything happened to me and my heart during this flight, the board-certified cardiologists at the Mayo Women’s Heart Clinic would know exactly what to do for me. If I survived the flight, that is . . . . .
Like many freshly-diagnosed heart attack survivors, my fear of having a heart attack on a plane was very strong. (Note: many survivors experience a very strong fear of having another heart attack just walking down the street).
So being strapped into a metal box 35,000 feet up in the sky, hour after endless hour, inhaling stale air, in a pressurized germ-infested environment, with reduced circulating oxygen levels in my blood, risking the onset of hypobaric hypoxia , and with no guarantee at all that my seatmate would be a board-certified cardiologist seemed just plain crazy.
But apparently there is good news about heart patients and flying from the British Cardiovascular Society.
Most people with heart disease who are not critically ill can safely fly on commercial aircraft, according to a U.K. report. (1) Lead author Dr. David Smith (Royal Devon and Exeter NHS Foundation Trust) told H eartwire:
” The overwhelming conclusion is that the cabin environment poses very little threat. It’s not the flying that’s the problem for heart patients, but the stability or instability of someone’s underlying condition that indicates the probability of a spontaneous cardiac event occurring while they are in the air.”
The passengers who might feel some minor physical effects of low blood oxygen (hypoxia) include those already at risk of:
- myocardial infarction (heart attack)
- heart failure
- abnormal heart rhythms
But according to Dr. Smith, the blood oxygen levels induced by flying “ appear to have little or no adverse circulatory effects, certainly not for short- and medium-haul flights.”
However, some heart patients at high risk are advised to “ defer travel ” until their condition is stable, including those:
- having an ejection fraction <40%
- showing signs and symptoms of poorly controlled heart failure
- with unstable angina or uncontrolled arrhythmias
- awaiting further investigation, revascularization, or device therapy
And here’s how soon after a cardiac procedure you are generally safe to fly:
- After uncompl icated elective (non-emergency) cardiac catheterization (angioplasty, wi th or without stent implants), patients can fly after a few days.
- If patients suffer from stable angina with infrequent attacks, they should be able to fly. It is safe to use nitroglycerin spray in a pressurized aircraft cabin.
- Patients with pacemakers implanted can fly after a few days, unless they have suffered a pneumothorax , in which case they should wait until two weeks after it has fully healed.
- Those with ICD s (Implantable Cardioverter Defibrillators) can fly after a few days, with the added recommendation that they should not fly after the ICD has delivered a shock until the condition is considered stable again.
- Those who have experienced a heart attack (myocardial infarction) can fly after 10-14 days. If you are older than 65 or if you’ve had another heart attack in the past, you’re statistically more likely to have one again. The U.K. Civil Aviation Authority recommends that i f you have no symptoms or other heart conditions and no further cardiac treatment is planned, you’re considered to be at low-medium risk to fly. But if further cardiac treatment is planned, you’re considered to be at higher risk of another heart attack – best not to fly at this time.
- Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts ( open heart surgery ) can usually fly after 4-6 weeks (longer if they have had pulmonary complications).
Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
But even when your physician has officially given you the green light to fly again, remember that severe fatigue can continue to be a serious issue for heart patients long after the other physical effects of cardiac procedures have healed.
Anticipating this fatigue may influence your decision, for example, to request an airport wheelchair or a ride to connecting gates on the airline golf cart, and to limit the weight and size of your carry-on bag. Please plan ahead and arrive at the airport significantly early for any flight to minimize rushing or stress.
The anxiety surrounding air travel can be debilitating even for non-heart patients. If fear of flying has ever been a serious issue even before your own cardiac event, it may indeed feel worse now. If you really must fly, ask your own doctor about managing this anxiety before your flight.
Long flights can mean crossing time zones, sleep deprivation and jet lag. Probably the most important effect of changes in sleep patterns for passengers with cardiovascular disease is the potential disruption in taking daily medications. It can be difficult to stick to a normal meds routine when that routine is altered, especially if we’re confused about what time it really is. The U.K. report warns that it’s especially important for passengers with stable heart failure, angina or arrhythmia to maintain the regularity of their medications.
If you’re planning an out-of-country flight in the near future, remember that most major insurance companies will not provide travel medical insurance earlier than 90 days after a cardiac event, or even after a change in your medical treatment. In some cases, just a doctor’s appointment in the past 90 days at which your medication dosage is changed (either increased OR decreased) can mean your condition can be considered “unstable” and thus grounds for denial when you file a travel medical insurance claim.
Each airline has its own policy for allowing flying passengers after a cardiac event – and as you’ll see from the Oregon heart patient’s experience with Alaska Airlines (described below), some of these policies appear to defy accepted medical guidelines. So call both your insurance broker and the airline before you book a flight to double-check all details relevant to your own travel and clinical circumstances.
For heart patients who sport implanted medical devices, it may be comforting to know that the amount of metal used in most implanted heart devices like pacemakers, heart valves or ICDs is very small, according to cardiologists at St. Jude Medical. It is usually not enough to set off airport security metal detectors ; if it does, simply show security personnel your patient identification card. Passing through a metal detector should not hurt your device. However, do not linger near the security system arches or poles.
Dr. Clemens Jilek and his team of researchers from the German Heart Center in Munich recently did a study on 388 heart patients, published in the journal Annals of Internal Medicine . They concluded that metal detector security screening appears safe for those with pacemakers or ICDs implanted.
What about those new full body scans at airport security gates and people with implanted pacemakers or ICDs? According to cardiologist Dr. Richard Fogoros , there are few if any controlled clinical studies or even written information about the safety of these full body scanners for heart patients:
“I called the technical support departments of two major pacemaker manufacturers. I was told that they regard the full body scanner as completely safe for those with implanted pacemakers and ICDs, and this is what they tell patients and doctors when they call for advice (which apparently they do frequently, since there is no written advice anywhere). I was told that:
- 1) their engineers have determined it is extraordinarily unlikely that these scanners are capable of negatively affecting implantable medical devices
- 2) many thousands of people with pacemakers and ICDs have used total body scanners over the past several years, and there has been no allegation of any problems.
“So, both engineering theory and a large volume of real-world experience indicates they are safe, according to them.
“There is no reason to believe that a full body scanner will effect a pacemaker or ICD, and medical device companies are willing to say that verbally (but not in writing).
“If you want to wait until some authority is willing to make a definitive written statement about this, you can opt for a pat-down instead when you go through airport security. Since this issue is in the hands of bureaucrats, however, don’t hold your breath waiting for a resolution.”
A serious health problem you may have also heard linked with air travel, particularly long flights, is deep vein thrombosis (DVT) and venous thromboembolism .
Although a long-haul flight doubles the risk of DVT, it is actually similar to that incurred during car, bus, or train travel for a similar period, the U.K. researchers state. And the absolute risk of DVT for a fit and healthy person is one in 6,000 for a flight of more than four hours, they note, pointing out that pilots are at no greater risk than the general population, a statistic that is not particularly comforting.
Now I have to worry not only about myself, but about my pilots. Why not take the advice of my heart sister Jaynie, who always harps at us to wear compression knee-high stockings while flying?
There are some recommended common sense flight precautions for those at risk of DVT:
- consume plenty of fluids
- exclude caffeine and alcohol
- wear compression stockings
- take a dose of low-molecular-weight heparin (a blood thinner)
- wear a MedicAlert bracelet or dogtag necklace at all times
- talk to your doctor to confirm that your cardiac disease is stable
- carry adequate supplies of all prescribed medicine
- carry a copy of your medical history
- carry emergency phone numbers for your doctor(s), family members and destination contacts
Having memorized these precautions, you might want to also consider the alarming case of one Oregon heart patient who describes her “very interesting flight” to Rochester, Minnesota to see cardiologist Dr. Sharonne Hayes at the Mayo Women’s Heart Clinic. Here is the transcript of her complaint against Alaska Airlines filed with the FAA:
“I mentioned to the E/C flight attendant that I carry nitroglycerin for chest pain in my pocket should I request assistance, and that it was only cautionary in nature because I was traveling alone. “The Head Flight Attendant ordered me off the flight because she ‘assumed’ that I was unhealthy. She required me to provide a doctors’ note clearing me to fly. She informed me that the FAA allows flight crew to decide who is fit to fly or not, and they can remove whomever they feel is unfit to fly. “Alaska Airlines customer services representative and flight attendant refused to speak with my cardiologist who was wakened at 6:30 a.m. on a Sunday morning because I did not have the “requested” doctor’s note. “I explained that the flight crew had no data to support their assumption that I was unfit to fly, nor did they request the other passengers to produce doctors’ notes. “Alaska Airlines discriminated against me based on the fact that I carry nitro in my pocket. They created a very stressful environment and threatened to impair my ability to seek medical care at the Mayo Clinic. They humiliated me in front of a plane full of passengers. “An air carrier may not discriminate against an otherwise qualified individual on the following grounds: 1) the individual has a physical or mental impairment that substantially limits one or more major life activities. 2) the individual has a record of such an impairment. 3) the individual is regarded as having such an impairment.”
(1) Smith D, Toff W, Joy M, et al. “ Fitness to fly for passengers with cardiovascular disease. The report of a working group of the British Cardiovascular Society “ . H eart 2010
COVID-19 UPDATE 2020: “ S hould I avoid plane travel just to be safe?”
“ Planes tend to be low humidity, but the air’s actually pretty clean. It gets re-circulated through these HEPA [high-efficiency particulate air] filters that really are very good at clearing stuff out,” said Dr. Vicki Hertzberg , a biostatistician at Emory University, who co-led a study on flights and disease transmission with scientists at Boeing. “Also, they suck in about 50% clean air with every re-circulation. So in some aspects, the air on a plane is cleaner than what’s going on in your new office buildings.”
Remember that Dr. Hertzberg’s advice applies only to passengers while the plane is in the air. As soon as that aircraft lands, passengers exit the plane and are no longer protected by HEPA filters while walking through the airport, or waiting at the baggage carousel, or shopping or dining in the airport, or getting onto airport transportation vehicles.
NOTE FROM CAROLYN: I wrote more about my fateful five-hour flight in Chapter One of my book, A Woman’s Guide to Living with Heart Disease . You can ask for it at your local library or favourite bookshop, or order it online (paperback, hardcover or e-book) at Amazon , or order it directly from my publisher, Johns Hopkins University Press (use the code HTWN to save 30% off the list price).
Like this? Share it with others!
- Click to email a link to a friend (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to print (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Tumblr (Opens in new window)
Published by Carolyn Thomas
View all posts by Carolyn Thomas
21 thoughts on “ How soon are heart patients safely fit to fly? ”
Very interesting . I have recently travelled from Houston to Perth. I had 2 heart stents inserted 3 weeks prior to my journey home. I have been home for 5 days now. I’m experiencing shortness of breath and nausea if I do too much.
I’m wondering if the jet lag and fatigue is the cause. I can’t do a lot as I become so exhausted.
Hello Kathleen – I’m sorry you’re experiencing these puzzling new symptoms. I’m not a physician so cannot comment specifically on your situation, but I can tell you generally that you’re still in relatively early days, post-stents. And as this post mentions, “severe fatigue can continue to be an issue for heart patients long after the other physical effects of cardiac procedures have healed.” It’s quite possible that the effects of jet lag and the travel itself are adding to that fatigue. If I were in your shoes, I’d contact my doctor just to check this out – especially if symptoms seem to be worsening instead of gradually improving.
Meanwhile, you could start a Symptom Journal ( more details here ) to track which specific activities seem to aggravate those symptoms. It’s important that recently diagnosed heart patients remain as physically active as possible – so you don’t want to stop moving or start dreading “doing too much” out of a fear of possible after-effects, but you also don’t want to be suffering!
Good luck to you! ♥
Hi Carolyn, I just some how have fallen outside of of the safety zones for flying. I was told from the point of my AMI that my heart was to weak to withstand G-force meaning flying will forever be out of range. Since then I’ve developed Supraventricular tachycardia (SVT-fast or irregular heartbeat) with episodes of SCD that won me an A-ICD (implanted defibrillator). The worse part of all is I don’t feel my SVTs, and my SCD has me going down in slow motion. I’m not allowed to move to far from where I am.
Lastly I have a stent and an A-ICD, I have set off security alarms and it does hurt. They say that we shouldn’t but my stent has set of the alarm. We were given color coded cards to carry with us when the devices were implanted. My stent is at the top of the list. In the 12 years since my AMI I’ve two long road trips. Both were 12 hour bus trips to New York. The first with the cardiac therapist and staff at the heart hospital, super safe trip. The second was with family for a weekend trip, they had to stop every three hours to slow swelling of feet and legs. Robin
This was so interesting to learn about my condìtion. And I will use the knowledge to teach others.
I am with CABG 2 months ago, I have breathing problem, can I traveling by air?
Hello Majid, only your cardiologist can answer you. The U.K. report suggests 6 weeks minimum before CABG patients fly, but longer if you have pulmonary problems. Ask your doctor – and good luck to you.
The NHS choices website also gives information apparently after discussion with the CAA. This suggests that you can safely fly 10 days after chest surgery or CABG. Clearly there is enormous variation in the advice given by different bodies.
With breathing complications like Majid describes, that 10-day suggestion may not be appropriate, which is why the best answer is to consult with her own physician.
Very comprehensive article. Thanks for this useful list of flying-related tips and facts. Now if you could just help us make the airlines run on time to get rid of those long delays . . .
Yeah, I’ll get right on that . . . 😉
Hi, I enjoyed this post. As a person who has congenital heart disease I have often faced “complications” at airports, with one particular gentleman asking what the “HUGE” scar was.. Well how rude.
I am from England and I have had lots of operations, ablations, implants, etc. But travelled a lot as I do not let it get in the way. I just would like to say that I have always brought insurance to cover myself (and family), especially for my heart, and although it costs a lot sometimes, it’s worth every penny.
Do not let it stop you travelling but always listen to your doctor too, if they say no, then go with that; save your money and go another time (she says through grumbled teeth, wanting to see her friends in America).
Great article.
That IS rude! (what’s the huge scar from? Preferred answer: How about “None of your frickety-frackin’ business!” ?!?) Travel insurance is such an important issue for heart patients as some policies will NOT cover pre-existing conditions or even incidents that follow a recent doctor’s appointment or meds change! Always read the fine print. Good luck with getting to America to see your friends!
Rude question answer, “I had my heart removed so insensitive questions like yours won’t hurt it.” But then, I am a brat! 🙂
Elizabeth Youmans RN, BSN
Like Liked by 1 person
My husband had a heart attack and cardiac arrest last week, not sure how much of the large muscle will return but hopeful, and he’s walking and breathing good. We also go abroad. Now feel worried as lots of people who have had heart attacks go, but have not seen any post re cardiac arrest. Whether this makes a difference, also been told as a cardiac arrest person it’s very difficult to get insurance, can you shed any light?
Hi Brian – The good news is that walking and breathing seem fine so far! I just went back and re-read the U.K. report mentioned in my post. You are right – nothing specifically about cardiac arrest; they seem to include that condition within heart attack criteria. Your cardiologist involved will have far more info and be able to advise both of you on the safety of international flights based on unique details of the case. Getting out-of-country travel medical insurance – regardless of cardiac arrest or any other cardiac diagnosis – is fraught with fine print designed to deny medical claims based on how “unstable” the patient’s condition is (but even a doctor’s appointment during the past 90 days at which any treatment decision is adjusted – like decreasing the dosage of a previously prescribed drug because the patient is doing better! – can suggest to the insurance company that the condition is now “unstable”). Talk to a trusted insurance broker for more info. Best of luck to you…
- Pingback: Tea&Biscotti
Hi Carolyn,
This is a very good post and one you should run every year at the start of vacation time. I said that I had been given paper work somewhere regarding travel and not to for this first year. It was clearly written in this post. When I went on my trip, they were running tests on me because of my edema. It dropped my EF (ejection fraction) down to 40% and they still haven’t been able to find out why. I also have congestive heart failure, when I talk about taking a trip I mean going outside of my state.
I went on a 12 hours-one way, and 12 hours-back home trip. I know that they had told me not to take trips without first talking it over with the doctor; this was one of those times in which I looked for someone to agree with me as opposed to following orders.
But it wasn’t an uneventful trip. I began to feel the discomfort shortly after heading back. They wanted to know if I wanted them to get emergency help, and I told them I could make it home. It was a week before I began to feel better.
I won’t make that mistake again, this is a very good posting for all of us, it reminds us of things we try to forget.
Very useful overview for those of us wondering about how soon is “too soon to fly”. Thanks for sharing this.
After I had heart surgery 4 years ago, I worried constantly about having another incident. But my most recently job had me traveling 50 – 75% of the time including many flights or long drives in the car. What my cardiologist was able to reassure me is that my continuing to control my diet, exercise and blood pressure should keep me healthy. Thanks for the article and the common sense flight precautions.
hallo there, thanks for this info on flying.I don’t have heart disease but the last time I flew, at Easter week the woman sitting next to me on the plane suffered a heart attack about 30 min out of Gatwick. The airline staff were very good, and they managed to keep her calm and the plane landed safely within a very short time and she was immed evacuated. I don’t know what happened to her after that but I can see how terrifying it might be if U are a heart patient and U are trapped in a plane. It was certainly terrifying for the rest of us to witness. Thx for your very good work here on this website. Useful and well-done.
Very excellent advice of highest quality on flying following a heart incident. My wife must fly to our daughter’s wedding in two months and already she is worried very much since her own heart incident so I’m showing to her this article. Thank you.
Your opinion matters. What do you think? Cancel reply

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- What to Expect
Triple Bypass Surgery: What to Expect on the Day of Surgery
Before the surgery, during the surgery, after the surgery.
- Next in Triple Bypass Surgery Guide Triple Bypass Surgery: Recovery
Triple bypass surgery is a major surgery that takes between three to six hours. It requires general anesthesia, meaning you'll be unconscious while it's happening. On average, you'll remain in the hospital for up to seven days.
By understanding what happens before, during, and after triple bypass surgery, you can increase your chances of success.
The day of triple bypass surgery can be hectic and overwhelming. If the surgery is planned, you will have more time to prepare both mentally and physically for the procedure. If it is an emergency, preoperative tests are very time sensitive and multiple examinations may be happening at once.
On the day of the procedure, you will meet with the entire healthcare team including the cardiothoracic surgeon , cardiologist, anesthesiologist , perfusionist , operating room nurses, and other surgeons as needed. All operative consent forms will be signed at this time to ensure you are fully prepared and do not have any additional questions or concerns.
The registered nurse will take vital signs including:
- Blood pressure
- Temperature
- Respirations
- Pulse oximetry
Prior to going into the operating room for the procedure, patients will have preoperative tests done. This may include:
- Echocardiogram
- Electrocardiogram (EKG or ECG)
- Chest X-ray
- Carotid ultrasound
- Pregnancy test (if indicated)
You will also be given a surgical soap that must be used on the surgical sites to properly cleanse the area and prevent infection. After cleaning, you will be given a hospital gown and the nurse will shave the surgical area if needed. The surgeon will mark the surgical site after you are fully prepped.
Your medications will be reviewed by the nurse and surgical team. Be prepared to discuss all of your medications, vitamins, and supplements at this time including the dosages, the last time they were taken, and how often they are taken. Bringing a list of the information is helpful so nothing is missed.
Patients are instructed to empty their bladder prior to going into the operating room, and asked to remove all jewelry, glasses, contact lenses, and dentures if applicable.
Finally, the nurse will insert an intravenous catheter (IV) that will be used to provide hydration, medications, and anesthetics during the procedure.
When it’s time for the surgery, you will be taken into the operating room on a stretcher and then placed onto the operating room table. You will then be prepared for general anesthesia , which will last for the duration of the surgery. Before the operation begins, the following will take place:
- You will be given a small dose of medication to help you relax while the surgical team is preparing.
- Vital sign monitors are placed.
- Your skin will be cleaned again with surgical cleaner and draped in sterile drapes, exposing only the surgical area(s).
- Once you are sedated by the anesthesiologist, an endotracheal tube will be placed to help you breathe during the procedure. Anesthesia medications relax your muscles making it difficult to breathe and this procedure will allow the team to help control your breathing while on the ventilator .
Once you are fully prepped for surgery, the surgical team will first harvest the three vessels needed for the bypass. Blood vessels can be taken from your leg ( saphenous vein ), inside your chest (internal mammary artery), or your arm ( radial artery ).
After the surgeons harvest the vessels, a midsternal vertical incision is made in the center of the chest in order to access the heart. The patient may be placed on a bypass machine during the procedure depending on the surgeon. The surgery can be performed "on-pump" or "off-pump".
On-pump surgery refers to the use of a heart-lung machine that circulates blood and breathes for the body throughout the surgery. The machine allows doctors to stop the heart.
The second technique used is off-pump surgery , also called “beating heart surgery.” It is done while the heart is still beating, and does not use the heart-lung machine. This is a more difficult surgery to perform because of its technical precision, but is the preferred approach for some surgeons.
According to the National Institute for Health and Care Excellence (NICE) , the procedure works as well as a coronary artery bypass using a pump. It is a newer technique that has shown some increased benefits, including:
- Quicker than the conventional procedure
- Reduces the chance of bleeding during the surgery
- Decreased risk of certain serious complications after surgery, such as a stroke
- Shortened hospital stay
After the grafts have been placed, the heart is restarted (if needed) via controlled electrical shocks. The surgical incision is closed using mesh webbing, sutures, and/or staples depending on the surgeon's preference.
Immediately following triple bypass surgery, you will be transferred to the intensive care unit (ICU) or cardiac intensive care unit (CICU or CCU) for close monitoring. You will typically have an endotracheal breathing tube for several hours after surgery and still be connected to a ventilator.
You will be given medication to keep you sleepy. If you start to wake up, you will not be able to talk with the breathing tube. It may feel uncomfortable but shouldn't be painful. Once fully awake, the breathing tube will be removed.
You will spend a minimum of one day in the intensive care unit and will be hooked up to a variety of machines including a monitor for vital signs, an IV pump to deliver fluids and medications, and a catheter to drain your bladder.
After the initial ICU recovery, you will be moved to a post-surgical unit to continue your recovery. At this time, you will meet with a physical therapist, occupational therapist, and nutritionist to continue the recovery process.
Following the procedure, everything will be harder to do including eating, dressing, bathing, and other activities of daily living. This is normal and to be expected after undergoing triple bypass surgery. Working with the healthcare team will help you start to feel more normal.
A Word From Verywell
It's important to follow all instructions from the healthcare team before, after, and during triple bypass surgery. This surgery, while the most common open heart procedure, is very serious and there is the possibility of life-threatening complications.
Discuss any concerns and questions with your surgeon prior to the procedure to fully understand not only the surgical procedure but also the recovery process.
Society for Cardiovascular Angiography and Interventions. Your care team during coronary bypass surgery .
National Heart, Lung, and Blood Institute. Coronary artery bypass grafting .
Johns Hopkins Medicine. Coronary artery bypass graft surgery .
University of Michigan Health. Coronary artery bypass surgery: When you arrive at the hospital .
Martínez-González B, Reyes-Hernández CG, Quiroga-Garza A, et al. Conduits used in coronary artery bypass grafting: A review of morphological studies . ATCS . 2017;23(2):55-65. doi:10.5761/atcs.ra.16-00178
Melly L, Torregrossa G, Lee T, Jansens JL, Puskas JD. Fifty years of coronary artery bypass grafting . J Thorac Dis . 2018;10(3):1960-1967. doi:10.21037/jtd.2018.02.43
Johns Hopkins Medicine. Off-pump coronary artery bypass surgery .
National Institute for Health and Care Excellence. Off-pump coronary artery bypass grafting: Interventional procedures guidance . Published January 26, 2011.
By Kathleen Gaines, MSN, RN, CBC Kathleen Gaines, MSN, RN, CBC, is a nurse and health journalist, as well as an adjunct clinical faculty member at hospitals in the Philadelphia area.

- See All Locations
- Primary Care
- Urgent Care Facilities
- Emergency Rooms
- Surgery Centers
- Medical Offices
- Imaging Facilities
- Browse All Specialties
- Diabetes & Endocrinology
- Digestive & Liver Diseases
- Ear, Nose & Throat
- General Surgery
- Neurology & Neurosurgery
- Obstetrics & Gynecology
- Orthopaedics
- Pain Medicine
- Pediatrics at Guerin Children’s
- Urgent Care
- Medical Records Request
- Insurance & Billing
- Pay Your Bill
- Advanced Healthcare Directive
- Initiate a Request
- Help Paying Your Bill
.cls-1{fill:#2e64ab;}.cls-2{fill:#fff;} CS-Blog Cedars-Sinai Blog
Bypass patient on the road to recovery.
May 01, 2019 Cedars-Sinai Staff

Jim Calio was having an ordinary day until he walked up a flight of stairs and nearly passed out. A trip to the Smidt Heart Institute revealed that two of his arteries were 70 percent blocked and that he would need triple bypass surgery .
"I was on track for a massive heart attack if I hadn't taken care of this," Calio says.
Today, thanks to at the institute's Preventive and Rehabilitative Cardiac Center , the 70-year-old journalist is energetic and healthy.
"The crazy thing was that a week before I went in the hospital I was working out every day on machines, lifting weights, and I felt great. "It was when I was walking that I said, 'Something's not right.'"

Jim Calio's dog, Samantha, has been a constant companion through his recovery from triple-bypass surgery. A crucial element of his recovery was the monitored exercise program at the Preventive and Rehabilitative Cardiac Center.
During outings with his dog, Samantha, Calio first felt the shortness of breath that was signaling his heart trouble. But he didn't take the symptom seriously. He knew he had plaque buildup in at least one artery, but he thought he had it under control with cholesterol medications and a healthy diet.
"The crazy thing was that a week before I went in the hospital I was working out every day on machines, lifting weights, and I felt great," he says. "It was when I was walking that I said, 'Something's not right.'"
A crucial element of Calio's recovery was an exercise regimen, which he chose to complete at the Preventive and Rehabilitative Cardiac Center. He could have attended a rehabilitation facility closer to his home, but he wanted to continue working with the Cedars-Sinai staff he trusted.
Read: Shortness of Breath: When to See Your Doctor
"They know me, they have my chart and they are very attentive," Calio says.
"If you let it, a [heart event] can become all-consuming. Early on in the recovery, maybe out of fear, you think, 'Gee, I wonder if it's going to be OK? Will I be able to exercise again?'"
The center is outfitted with equipment designed to assist and strengthen the cardiovascular system. Patients in the exercise program wear heart monitors that display their heart rate and rhythm during exercise. The center's team members closely watch the heart rhythm from monitors and advise patients on how hard to exert themselves on the treadmills, stationary bicycles and other equipment.
Read: Heart Attack, Cardiac Arrest, Heart Failure—What's the Difference?
"My confidence came back right away," Calio says of his experience at the center. "I walked in my neighborhood, too—first without the dog, then with her. I felt great. No huffing and puffing."
Calio has an affectionate nickname for the center: "I call it the Cardio Club."
His dedication to his prescribed exercise and rehabilitation program has been crucial to his full recovery. He is back to his normal exercise routine, including weightlifting, and is planning travel-writing trips such places as London, Hong Kong and Ireland.
"This is a lot of fun, and it's kind of gravy on my career," he says of his travel writing, which he took up after working as a journalist for publications such as People, Newsweek and Life magazines in the 1970s, '80s and '90s. "I'm not going to retire. I'll keep cranking out stories as long as I can."

Jim Calio walking with his dog Samantha after undergoing triple bypass surgery at Cedars-Sinai.
Popular Categories
Blog & magazines, popular topics, make an appointment, call us 7 days a week, 6 am - 9 pm pt, support cedars-sinai.

- Weill Cornell Medicine

- When You Can Fly
Generally, you should wait to fly until after you have had your first postoperative visit with your surgeon.
- Remember that in the airport terminal, you may not have the stamina to walk as fast or far as you did before the surgery.
- Also remember that you cannot carry anything heavier than 10 pounds for the first six weeks after the surgery, so you'll have to arrange for your heavier bags to be carried by someone else.
Related Links
- Postoperative Incisional Pain
- When You Can Drive
- Diet Following Stomach Fundoplication
Contact Us Digital Health Services
Weill Cornell Medicine Cardiothoracic Surgery 525 East 68th Street Box 110 Suite M 404 New York, NY 10065 Directions Phone: (212) 746-5166 Email: [email protected]
- Your Presurgical Appointment
- The Day of Your Surgery
- Information for Families
- Guide to Heart and Aortic Surgery
- Guide to Lung, Stomach, Mediastinal, or Esophageal Surgery
Many good years after heart bypass surgery, but something happens after ten years
The probability of continuing your life following bypass surgery is close to being the same as for the population in general - once a patient has completed the procedure. but a study from aarhus, denmark, shows that mortality increases after 8-10 years..
The probability of continuing your life following bypass surgery is close to being the same as for the population in general -- once the patient has completed the procedure itself. But a register study from the Department of Clinical Epidemiology at Aarhus University, Denmark, shows that mortality increases after 8-10 years.
The prognosis following heart bypass surgery is both good and has improved over the past three decades. In fact, the survival rate for bypass patients who make it through the first month after the operation is close to that of the population in general. But 8-10 years after a heart bypass operation, mortality increases by 60-80 per cent. This is new and important knowledge for the doctors who monitor these patients.
This is the main conclusion of a comprehensive national register-based study that sheds light on the thirty-year prognosis following a heart bypass operation, which has just been published by the Department of Clinical Epidemiology under the Department of Clinical Medicine at Aarhus University. The basis for the study is all of the approx. 51,000 Danish patients who have undergone surgery in the period 1980 -- 2009. They have subsequently been correlated with a control group of 500,000 people of the same age and gender drawn at random from the general population.
"The study shows that the rate of survival has improved over the last three decades, so that the probability of continuing your life following bypass surgery is close to being the same as in the general population. This holds true providing that the patient has successful surgery and for the eight-ten years after the surgery. However, after this point the prognosis changes," says medical doctor and PhD student Kasper Adelborg from the Department of Clinical Epidemiology.
Kasper Adelborg is the primary author of the publication 'Thirty-Year Mortality After Coronary Artery Bypass Graft Surgery. A Danish Nationwide Population-Based Cohort Study', which has recently been published in the American journal Circulation: Cardiovascular Quality and Outcomes .
The study shows that ten-year-survivors have an increased mortality of between 60 and 80 per cent when compared with the general population. This may be due to the fact that the disease is progressive and that the atherosclerosis or hardening of the arteries increases, or that the implanted material begins to fail.
"Our register study covers all patients who underwent bypass surgery throughout the last decades throughout Denmark, and there will naturally be differences in the prognosis from patient to patient. So the clinicians who are in contact with the patients should therefore assess their prognosis individually -- and there are special reasons to do this after the initial eight -ten years, as we now know that 'something' happens," says Kasper Adelborg about the perspectives of the study, which is currently being tweeted all over the world -- and which has triggered a personal email to Kasper Adelborg from the journal's chief editor, who is impressed by the possibilities for studying long-term prognosis following heart bypass surgery using high quality data.
"Of course, this has to do with the fact that we in Denmark have unique opportunities to link register information from the registries. When we work with a control group of half a million Danes, we have the possibility of directly comparing the prognosis for a 55-year-old man who has undergone bypass surgery with a 55-year-old man who has not had surgery from the control group," explains Kasper Adelborg.
"It may be that we see this as an obvious correlation to make in Denmark, but the fact is that we in Denmark keep such good track of our citizens that many other countries envy us. In other places such as the US, it is not possible to simply extract information about when people have undergone surgery or died. This is information which is not centrally registered and which can therefore be lost if, for example, someone moves to a different region or state," says Kasper Adelborg.
In addition to the new knowledge about a special 'period of attention' 8-10 years after the bypass surgery, the first month is particularly critical.
Within the first 30 days after bypass surgery, patients have an increased risk of dying in connection with the operation, which is not in itself new.
"It is well-known that there are risks associated with a complicated operation in the heart, but fortunately mortality in connection with the surgery itself is quite low. What is new is that we have precise figures for the prognosis, including the long-term prognosis for patients who have undergone bypass surgery, compared with the rest of the population," says Kasper Adelborg.
- Heart Disease
- Today's Healthcare
- Wounds and Healing
- Cosmetic Surgery
- Diet and Weight Loss
- Patient Education and Counseling
- Liposuction
- Artificial heart
- Coronary heart disease
- Ischaemic heart disease
- Parasympathetic nervous system
Story Source:
Materials provided by Aarhus University . Note: Content may be edited for style and length.
Journal Reference :
- Kasper Adelborg, Erzsébet Horváth-Puhó, Morten Schmidt, Troels Munch, Lars Pedersen, Per Hostrup Nielsen, Hans Erik Bøtker, Henrik Toft Sørensen. Thirty-Year Mortality After Coronary Artery Bypass Graft Surgery . Circulation: Cardiovascular Quality and Outcomes , 2017; 10 (5): e002708 DOI: 10.1161/CIRCOUTCOMES.116.002708
Cite This Page :
Explore More
- Record Low Antarctic Sea Ice: Climate Change
- Brain 'Assembloids' Mimic Blood-Brain Barrier
- 'Doomsday' Glacier: Catastrophic Melting
- Blueprints of Self-Assembly
- Meerkat Chit-Chat
- First Glimpse of an Exoplanet's Interior
- High-Efficiency Photonic Integrated Circuit
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
Trending Topics
Strange & offbeat.
NEWS... BUT NOT AS YOU KNOW IT
I was feeling tired and then one simple health test saved my life

Share this with

I’ve always really enjoyed working out.
I appreciate that might seem obvious given I spent decades as a professional footballer, but even now, long since I’ve retired, I’m in the gym constantly. I’m the type of person who, if he works out six days in a week, feels guilty for missing that seventh.
That’s why, in 1992, when I was 38, just two years after playing my final game for Rangers, I didn’t expect to have any major health problems, not least the life saving heart surgery that I had to have.
At the time, I was managing Liverpool , and I was following the exact same training regime as the players – in fact, when they went home at lunchtime after a morning session, I was usually straight back in the gym.
Looking back, the only clue I had that something was wrong was just the tiredness. It was something I’d never experienced before.
I also noticed that just one glass of wine or pint of beer would start a headache coming on, but I still didn’t think there was anything badly wrong, other than a vague sense of being a bit out-of-sorts.
So to say it was a shock to discover I had coronary heart disease, which is when a blockage stops blood supply to the heart, meaning I needed a triple bypass, is an understatement.
It was all down to bad cholesterol levels and extremely high blood pressure.
A club doctor at Rangers had told me previously that my blood pressure was previously a bit high – but I attributed that to the stresses and strains of football.
But in 1992, back at Liverpool, a doctor classed my blood pressure as ‘very high’, and further tests, including two electrocardiograms, revealed I needed the triple bypass.

At the time, I was surprised given my level of fitness, but I was just determined to get through the operations and get back to work.
Almost exactly 32 years on from having open heart surgery, and managing my condition with simple medication, I’m the perfect example of how high blood pressure can truly impact anyone, no matter who they are, and why I’m backing a new campaign by NHS England to encourage adults to get their blood pressure checked.
High blood pressure is one of the major risk factors for cardiovascular disease (an umbrella term for a number of conditions including coronary heart disease) – untreated, it can lead to serious health problems, from heart attacks to strokes to vascular dementia.

But the good news for me, and for the millions of others dealing with high blood pressure is that not only is it incredibly treatable, it’s really easy to get checked.
So my message is simple – go and get checked. It’s scary thinking back that I had no idea how badly wrong things were going in my body, but now we have much better awareness, and knowing your blood pressure could genuinely save your life.
It’s incredibly helpful as well that pharmacies are able to help with this campaign – it’s free and you don’t need to book in advance. It’s simply a matter of Googling your nearest pharmacy, getting that sleeve on the arm and the quick check, and you’re on your way within five minutes.
Two of my uncles died prematurely, and my dad had his own bypass at 70, so it was always likely to be an issue for me.
Frankly, if you are at risk (for example having a family history like I did, or being overweight or over the age of 65) – you owe it to yourself and your family to stay healthy, whether that’s making lifestyle changes or taking the medication that has been so helpful for me.
For me, I knew that I owed it to my children especially to get better, and to continue to look after myself. I’ve had a great life, but without the drugs I’ve taken for the past thirty-odd years, which help keep my blood vessels in good shape, I’d have been in serious trouble.

There’s of course an element of social conscience about dealing with high blood pressure, which is another reason I’m part of this campaign.
But it’s important not to focus just on those who have experienced high blood pressure as a result of something like being overweight.
I know there’ll be young men and women reading a warning like this and thinking ‘well obviously this won’t apply to me, I’ve run marathons, I’m in the gym all the time, I eat well and I’m sensible with my alcohol intake.’
I was doing all those things too! I was a professional football player from the age of 15 to my late thirties, and I still found myself dealing with high blood pressure through no fault of my own.
In the world of football, which I’m still involved in as a pundit, there’s been a number of high-profile incidents involving athletes with heart issues (like Tom Lockyer of Luton, who suffered a cardiac arrest on the pitch last year, or Christian Eriksen, who collapsed during Euro 2020 while playing for Denmark.)
While those cases weren’t related to high blood pressure, for me it all underlines that message that if serious health conditions can happen to these super fit athletes, it can happen to you, much like it did to me over three decades ago.
Getting checked over is an investment for your future health, looking after yourself while you are young – and even at my age – is the right thing to do for your health and your family!
Taking a couple of pills every day is a small price to pay for the health and time with my family I’ve enjoyed since that first diagnosis.
I want the same for everyone, no matter how at risk they think they are, or aren’t.
Take it from someone who never thought they would have high blood pressure, much less major heart surgery – it can happen to absolutely anyone, at any time.
So go and get that check.
As told to Ross McCafferty
More from Metro

Run clubs have become our new nightclubs – here’s why
You can find a pharmacy that offers free blood pressure checks near you by searching “pharmacy blood pressure check” or visiting the NHS website here .
Do you have a story you’d like to share? Get in touch by emailing [email protected] .
Share your views in the comments below.
MORE : Paul Merson fumes after Chelsea star who is ‘best in the business’ misses out on England’s Euro 2024 squad
MORE : Thousands could receive just £215 after parasite outbreak left water undrinkable
MORE : I was told by my GP that my nasty hangover was actually an STI I’d never heard of
Sign up to our guide to what’s on in London, trusted reviews, brilliant offers and competitions. London’s best bits in your inbox
By ticking this box, you confirm you are over the age of 18*. Privacy Policy »

You were sitting down, wearing a blue top and with sunglasses on top of…
To Issy/Izzy, the kind, intelligent and chatty girl, originally from…
Enter your birthday for your free daily horoscope sent straight to your inbox!
Get us in your feed
- Sports Betting
- Sports Entertainment
- New York Yankees
- New York Mets
- Transactions
Recommended
Mark vientos responds to mets chance with home run in strong outing.
- View Author Archive
- Email the Author
- Follow on Twitter
- Get author RSS feed
Contact The Author
Thanks for contacting us. We've received your submission.
Thanks for contacting us. We've received your submission.
CLEVELAND — Mark Vientos received an opportunity Tuesday to show he’s more than just a part-time bat against left-handed pitchers.
With Brett Baty struggling at the plate, manager Carlos Mendoza gave Vientos a start at third base. Mendoza cited the fact that Guardians starting pitcher Xzavion Curry had reverse splits and was tougher against left-handed hitters.
Vientos responded with a 2-for-4 performance that included a homer in the Mets’ 7-6 loss at Progressive Field.

“It all starts with your routine and your plan and I feel like we did a good job over here talking about our approach and plan and I kind of feel that when you speak it out loud you go do it out there,” Vientos said.
Baty entered the day with a .180/.255/.320 slash line with two homers and six RBIs in May. He had struck out in 42 percent of his plate appearances, including three times in Monday’s loss.
“[Monday] he had one of those where he was in between, missing his pitches and chasing when he gets behind in the count,” Mendoza said. “I thought Sunday he had a better day, but right now it’s one of those where he is going through it, but I like where he’s at mentally and he’s putting the work in.”
"It must be the shoes!" Mark Vientos gets the Mets on the board with a homer pic.twitter.com/iz2hnGrSft — SNY (@SNYtv) May 21, 2024
Baty’s ability to block out his offensive troubles and not let it affect the rest of his game is the best sign to Mendoza.
“He’s separating the offense from the defense, he’s still bringing it, his attitude in the dugout, his energy, so there’s a lot to like,” Mendoza said.
Vientos was recalled from Triple-A Syracuse last week and showed life at the plate in the weekend series in Miami. Vientos hasn’t committed an error since his recall.

Kodai Senga played catch, according to Mendoza, and has rescheduled his bullpen session for Friday. The right-hander skipped his bullpen on Sunday because of triceps soreness. Senga has been delayed in starting a minor league rehab assignment as he looks to work on his mechanics.
Drew Smith threw a bullpen session and will be evaluated for a minor league rehab assignment.
Jeff McNeil, who went 2-for-4 with a homer, owns an .812 OPS on the road this season. McNeil’s OPS at Citi Field is .449.
Share this article:

IMAGES
VIDEO
COMMENTS
Two weeks. The National Health Service recommends checking with your airline BEFORE flying, since companies have varying regulations on post-surgery travelers. However, the Civilian Aviation Authority says that 10 to 14 days is sufficient after chest surgery or a coronary artery bypass graft. After any heart operation, patients should remain ...
After triple bypass surgery, most people stay in the hospital for five to seven days. Once you've returned home, it can take up to 12 weeks to fully recover. During this time, your healthcare provider will likely refer you to an outpatient cardiac rehabilitation program. Find out how to recover from triple bypass surgery, including recovery ...
When you get home from the hospital, you might experience: frequently and go away within a couple of weeks. If it worsens, contact your surgeon. • Muscle pain or tightness — You might feel discomfort. • Reduced appetite — It takes a few weeks for your appetite to return. Your sense of taste may be weaker and certain smells might make ...
Life expectancy after a first bypass surgery is estimated to be 18 years. This varies based on many factors, such as age and overall health. Survival rates after a triple bypass have been shown to be about 71% at 10 years, 28% at 20 years, and 9% at 30 years.
Overview. Coronary artery bypass surgery creates a new path for blood to flow around a blocked or partially blocked artery in the heart. The surgery involves taking a healthy blood vessel from the chest or leg area. The vessel is connected below the blocked heart artery. The new pathway improves blood flow to the heart muscle.
Many people complain of having trouble sleeping for some time after heart surgery. You may experience insomnia (an inability to sleep) because of: Effects of anesthesia. Discomfort related to healing. Changes in your daily routine. Stress from personal concerns. Normal sleeping patterns typically return in two to three weeks.
How soon after open heart surgery you can fly depends on your doctor's recommendation about your overall condition and other factors. For example, if you've had a minimally invasive cardiac surgery with no complications, you may be able to fly within two to four weeks. For more moderate or intense open heart surgery, such as heart bypass ...
Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts (open heart surgery) can usually fly after 4-6 weeks (longer if they have had pulmonary complications). Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
Heart bypass surgery is a procedure to improve blood flow to your heart when you have coronary artery disease. A surgeon takes a blood vessel from another part of your body to go around, or bypass ...
Coronary bypass surgery treats blockages or the narrowing of one or more arteries that surround the heart. This operation aims to restore blood supply to the heart muscle. Your doctor will likely ...
Apply lidocaine patches to minimize pain and itching near your incision site. Hold a pillow to your chest. This is especially important when coughing or laughing. Use a heating pad or ice pack ...
during and shortly after surgery. You can't talk, eat or drink while the tube supports your breathing. It's uncomfortable, but it's usually removed within hours after surgery. You may stay in the ICU for a few days depending on . the type of surgery you had and your recovery time. Afterward, you may move to a regular hospital room.
CABG can be lifesaving. The average life expectancy after CABG is about 18 years . CABG is a major operation that can take between 3 to 6 hours to complete. And most people make a good recovery — serious complications after CABG surgery aren't common. Heart surgeons go through years of specialized training.
What is the life expectancy after triple bypass surgery? People can live many years after a triple bypass surgery. Ten years after having a coronary artery bypass, more than 75% of people are still alive. Taking prescribed medicines and making lifestyle changes give you a better long-term prognosis. These changes include: Eating a healthy diet.
Triple bypass surgery is a major surgery that takes between three to six hours. It requires general anesthesia, meaning you'll be unconscious while it's happening. On average, you'll remain in the hospital for up to seven days. By understanding what happens before, during, and after triple bypass surgery, you can increase your chances of success.
During CABG surgery, your surgeon either has to stop your heart temporarily or connect a blood vessel graft to your heart while it's still beating. "You can have an off-pump CABG or on-pump ...
Bypass Patient on the Road to Recovery. Jim Calio was having an ordinary day until he walked up a flight of stairs and nearly passed out. A trip to the Smidt Heart Institute revealed that two of his arteries were 70 percent blocked and that he would need triple bypass surgery. "I was on track for a massive heart attack if I hadn't taken care of ...
Your surgeon took a vein or artery from another part of your body to create a detour, or bypass, around an artery that was blocked and could not bring enough blood to your heart muscle. Your surgery was done through an incision (cut) in your chest. If the surgeon went through your breastbone, the surgeon repaired it with wire and a metal plate ...
We answer three common questions about heart bypass surgery. How long will it take to recover after heart bypass surgery? This can vary. The average is two to three months, but people over the age of 80 may find it takes longer than this. It's not unusual for it to take six months to a year to derive the full benefits of heart bypass surgery.
When You Can Fly. Generally, you should wait to fly until after you have had your first postoperative visit with your surgeon. Remember that in the airport terminal, you may not have the stamina to walk as fast or far as you did before the surgery. Also remember that you cannot carry anything heavier than 10 pounds for the first six weeks after ...
Never disregard or delay professional medical advice in person because of anything on HealthTap. Call your doctor or 911 if you think you may have a medical emergency. Depends: Immediately should be with care. After a month or so, same as most flyers, presuming all checkups are on target!
Travel after bypass. Jorj. Oct 3, 2014 • 10:14 PM. Thanks to all who replied to my earlier queries. My brother was operated in the neighbouring country, triple bypass on 23 september. In a week or so he will return home. I understand travel by plane is not recommended for a while. Can he travel by train ( 26 hours) safely ?
Many good years after heart bypass surgery, but something happens after ten years. ScienceDaily . Retrieved May 21, 2024 from www.sciencedaily.com / releases / 2017 / 06 / 170607123935.htm
5 minutes ago. Former Sunderland striker Marco Gabbiadini has revealed he is to undergo a triple heart bypass operation. Gabbiadini, now a pundit on BBC Radio Newcastle's Total Sport programme ...
New guidelines let the patients steer the process. For years, patients recovering from pelvic prolapse surgery have received variable and conservative post-operative activity restrictions, but the guidance has begun to change. These days, experts at Cleveland Clinic and elsewhere are rethinking their approach. Advertisement.
Very large text size. Cardiac surgery has been suspended at one of Melbourne's largest hospitals after a fault in a machine was discovered during a heart operation - the second equipment ...
Brooks Raley will undergo surgery next week for ligament damage and bone spurs in his left elbow, manager Carlos Mendoza said after the Mets' 7-6 loss to the Guardians on Tuesday.
An Austin Health spokeswoman said they were "aware of a technical issue involving our cardiopulmonary bypass machine", which plays a vital role during surgery and essentially acts as a patient ...
But in 1992, back at Liverpool, a doctor classed my blood pressure as 'very high', and further tests, including two electrocardiograms, revealed I needed the triple bypass. Graeme has been ...
Vientos responded with a 2-for-4 performance that included a homer in the Mets' 7-6 loss at Progressive Field. Mark Vientos celebrates his home run against the Guardians on Tuesday. USA TODAY ...