Advertisement

Wandering liver, spleen, and kidney: what the radiologist needs to know
- Published: 08 February 2023
- Volume 48 , pages 1854–1861, ( 2023 )
Cite this article

- Michael J. Caruso 1 ,
- Khyati Bidani 2 &
- Ajay Kumar Singh ORCID: orcid.org/0000-0002-9774-6399 2
404 Accesses
3 Citations
Explore all metrics
The wandering spleen, wandering liver, and wandering kidney are rare diagnoses that can be asymptomatic or are associated with nonspecific symptoms, making the clinical diagnosis elusive. In addition, given the small number of cases, these conditions are not well understood. Major complications of wandering spleen result from torsion of the vascular pedicle with resultant ischemia, physiologic dysfunction, and/or infarction. Wandering liver is commonly associated with bowel obstruction, particularly colonic volvulus, with very rare reports of hepatic ischemia or infarct. Wandering kidneys are not commonly associated with serious complications. In many cases, the wandering spleen, liver or kidney can be found in their anatomic position on static imaging and are only diagnosed during ultrasound or with serial radiographic or cross-sectional imaging with different patient positioning, or with prior studies demonstrating different locations of the involved organ. Treatment approaches for uncomplicated wandering spleen, liver, or kidney include watchful waiting and splenopexy, hepatopexy, or nephropexy, respectively. Complicated wandering spleens are treated with splenectomy. Given the variable clinical presentation of these conditions, imaging plays a pivotal role in diagnosing these rare and often incidentally discovered phenomena.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
The likely association between wandering spleen and absent left kidney
A torted wandering spleen: a case report
Torsion of the wandering spleen as an abdominal emergency: a case report
National Organization for Rare Disorders (NORD). https://rarediseases.org/rare-diseases/wandering-spleen/
Magowska, Anita. “Wandering spleen: a medical enigma, its natural history and rationalization.” World journal of surgery vol. 37,3 (2013): 545-50. doi: https://doi.org/10.1007/s00268-012-1880-x
Article PubMed Google Scholar
Richman, Mark et al. “Wandering spleen.” Surgery vol. 155,4 (2014): 728. doi: https://doi.org/10.1016/j.surg.2012.11.015
Varga, Ivan et al. “Anatomic variations of the spleen: current state of terminology, classification, and embryological background.” Surgical and radiologic anatomy : SRA vol. 40,1 (2018): 21-29. doi: https://doi.org/10.1007/s00276-017-1893-0
Desai, D C et al. “Wandering spleen: a challenging diagnosis.” Southern medical journal vol. 90,4 (1997): 439-43. doi: https://doi.org/10.1097/00007611-199704000-00017
Article CAS PubMed Google Scholar
Tirkes, Temel et al. “Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging.” Radiographics : a review publication of the Radiological Society of North America, Inc vol. 32,2 (2012): 437-51. doi: https://doi.org/10.1148/rg.322115032
Patel, R R, and K Planche. “Applied peritoneal anatomy.” Clinical radiology vol. 68,5 (2013): 509-20. doi: https://doi.org/10.1016/j.crad.2012.06.135 .
Cantone, Noemi et al. “Wandering Spleen and Organoaxial Gastric Volvulus after Morgagni Hernia Repair: A Case Report and Review of the Literature.” Case reports in surgery vol. 2016 (2016): 6450765. doi: https://doi.org/10.1155/2016/6450765
Article PubMed PubMed Central Google Scholar
Sodhi, K S et al. “Marfanoid hypermobility syndrome and skeletal abnormalities in a rare case of torsion of wandering spleen.” The British journal of radiology vol. 81,965 (2008): e145-8. doi: https://doi.org/10.1259/bjr/30123041 .
Fuentes, Rafael et al. “Hepatocolonic vagrancy: a rare or underrecognized entity?.” AJR. American journal of roentgenology vol. 188,4 (2007): W331-3. doi: https://doi.org/10.2214/AJR.05.0601 .
Howenstein, Matthew et al. “Wandering liver: multidetector CT features and the importance of multiplanar reformations.” Emergency radiology vol. 16,2 (2009): 155-7. doi: https://doi.org/10.1007/s10140-008-0707-4 .
Mack-Detlefsen, Birte et al. “Laparoscopic hepatopexy: a new surgical approach to hepatoptosis in an 11-year-old boy.” Journal of laparoendoscopic & advanced surgical techniques. Part A vol. 21,6 (2011): 567-9. doi: https://doi.org/10.1089/lap.2010.0485
Article Google Scholar
Nichols, Brandon W et al. “A wandering liver.” Pediatric radiology vol. 40,8 (2010): 1443-5. doi: https://doi.org/10.1007/s00247-010-1586-x .
Bruneau, Antoine et al. “Abdominal Pain due to a Wandering Liver.” Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract vol. 21,5 (2017): 923-925. doi: https://doi.org/10.1007/s11605-016-3277-x .
Bauones, Salem et al. “Wandering liver: ultrasound and magnetic resonance imaging diagnosis.” Journal of pediatric surgery vol. 47,11 (2012): e21-5. doi: https://doi.org/10.1016/j.jpedsurg.2012.07.007 .
Ordonez, Alex et al. “Wandering liver and intestinal malrotation: first report.” Surgical case reports vol. 2,1 (2016): 80. doi: https://doi.org/10.1186/s40792-016-0205-y
Tate, P S. “Hepatic torsion and dislocation with hypotension and colonic obstruction.” The American surgeon vol. 59,7 (1993): 455-8..
CAS PubMed Google Scholar
Susanto, C R, and Anne I J Arens. “A Wandering Kidney.” Kidney medicine vol. 1,6 402-403. 4 Nov. 2019, doi: https://doi.org/10.1016/j.xkme.2019.08.006
Article CAS PubMed PubMed Central Google Scholar
Srirangam, Shalom J et al. “Nephroptosis: seriously misunderstood?.” BJU international vol. 103,3 (2009): 296-300. doi: https://doi.org/10.1111/j.1464-410X.2008.08082.x
Bynum, B. “Floating kidney.” Lancet (London, England) vol. 357,9249 (2001): 76. doi: https://doi.org/10.1016/S0140-6736(05)71581-6
Sood, Akshay, and Craig Rogers. “Floating kidney.” BMJ case reports vol. 2018 bcr2018224921. 17 Apr. 2018, doi: https://doi.org/10.1136/bcr-2018-224921
Sarac, M., Bakal, U., Tartar, T., Canpolat, S., Kara, A., & Kazez, A. (2018). Bochdalek hernia and intrathoracic ectopic kidney: Presentation of two case reports and review of the literature. Nigerian journal of clinical practice , 21 (5), 681–686. https://doi-org.treadwell.idm.oclc.org/ https://doi.org/10.4103/njcp.njcp_217_17
Tchidjou, Hyppolite K et al. “Wandering spleen: 'presentation in adolescent with high thrombotic risk'.” Blood coagulation & fibrinolysis : an international journal in haemostasis and thrombosis vol. 25,5 (2014): 530-3. doi: https://doi.org/10.1097/MBC.0000000000000081
Reisner, David C, and Constantine M Burgan. “Wandering Spleen: An Overview.” Current problems in diagnostic radiology vol. 47,1 (2018): 68-70. doi: https://doi.org/10.1067/j.cpradiol.2017.02.007 .
Emanuels, Carolina S et al. “Displacement of the Spleen Mimicking Renal Cell Cancer Recurrence Post-Nephrectomy: A Case Report.” Journal of kidney cancer and VHL vol. 2,3 130-133. 20 Jun. 2015, doi: https://doi.org/10.15586/jkcvhl.2015.36
Zonca, Pavel et al. “Ectopic liver: different manifestations, one solution.” World journal of gastroenterology vol. 19,38 (2013): 6485-9. doi: https://doi.org/10.3748/wjg.v19.i38.6485 .
Blackburn, Simon C, and Michael P Stanton. “Anatomy and physiology of the peritoneum.” Seminars in pediatric surgery vol. 23,6 (2014): 326-30. doi: https://doi.org/10.1053/j.sempedsurg.2014.06.002 .
Parolini, Filippo, and Daniele Alberti. “Wandering liver.” Surgery vol. 161,4 (2017): 1174-1175. doi: https://doi.org/10.1016/j.surg.2016.01.021 .
Svensson, Jan F et al. “"Wandering liver" in a neonate: case report and review of the literature.” Journal of pediatric surgery vol. 45,3 (2010): 635-8. doi: https://doi.org/10.1016/j.jpedsurg.2009.12.017 .
Siddins, M T, and R J Cade. “Hepatocolonic vagrancy: wandering liver with colonic abnormalities.” The Australian and New Zealand journal of surgery vol. 60,5 (1990): 400-3. doi: https://doi.org/10.1111/j.1445-2197.1990.tb07392.x .
Download references
Author information
Authors and affiliations.
Department of Radiology, UMass Memorial Medical Center, Worcester, USA
Michael J. Caruso
Department of Radiology, Massachusetts General Hospital, 55 Fruit Street, Boston, MA, 02114, USA
Khyati Bidani & Ajay Kumar Singh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ajay Kumar Singh .
Ethics declarations
Conflict of interest.
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Caruso, M.J., Bidani, K. & Singh, A.K. Wandering liver, spleen, and kidney: what the radiologist needs to know. Abdom Radiol 48 , 1854–1861 (2023). https://doi.org/10.1007/s00261-022-03789-7
Download citation
Received : 13 October 2022
Revised : 19 December 2022
Accepted : 20 December 2022
Published : 08 February 2023
Issue Date : May 2023
DOI : https://doi.org/10.1007/s00261-022-03789-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Wandering spleen
- Wandering liver
- Ligament laxity
- Find a journal
- Publish with us
- Track your research

- Wandering spleen
Citation, DOI, disclosures and case data
At the time the case was submitted for publication Heba Abdelmonem had no recorded disclosures.
Presentation
Follow up of a case of lymphoma.
Patient Data
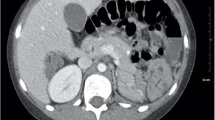
There is no evidence of splenic tissue at its normal position. A variant of the anatomic position is seen at the left lumbar region consistent with wandering spleen. No enlarged lymph nodes.
Case Discussion
Abnormally seated splenic tissue within the left lumbar region.
1 public playlist includes this case
- Prüfung by Dr. Kaan Kitapci
Related Radiopaedia articles
Promoted articles (advertising), how to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(1); 2023 Jan


Wandering Spleen: A Rare Case From the Emergency Department
Mahdi jawad.
1 Radiology, Qatif Central Hospital, Qatif, SAU
Mohamed H Yusuf
2 General Practice, Qatif Central Hospital, Qatif, SAU
Kaltham A Al Doaibel
3 General Practice, Royal College of Surgeons in Ireland, Dublin, IRL
Fatema M Nesaif
Ahlam s alharbi.
4 Family Medicine, Primary Health Care Center, Riyadh, SAU
The spleen is typically located in the left upper quadrant and is held in position by the suspensory ligaments, which include the gastrosplenic ligament, the splenorenal ligament, and the phrenicocolic ligament. Abnormalities within these ligaments result in the mobility of the spleen, so it may be located in the pelvis or iliac region, which is termed a wandering spleen. We present a case of a middle-aged man who presented to the emergency department with generalized abdominal pain and diffuse guarding and tenderness. The patient had a previous history of peptic ulcer disease and multiple emergency department visits for gastritis. Given the assumed diagnosis of perforated viscus, the patient underwent a computed tomography scan that demonstrated the absence of the spleen in its usual location and showed an ectopic pelvic spleen. The patient underwent successful surgical treatment with splenopexy. The wandering spleen is a rare medical condition that presents a clinical diagnostic challenge and requires a high index of suspicion. Despite its rarity, the wandering spleen should be considered in patients with recurrent abdominal pain.
Introduction
The spleen is normally located in the left hypochondriac region of the abdomen. It is primarily held in position by the suspensory ligaments, including the gastrosplenic ligament, the splenorenal ligament, and the phrenicocolic ligament. The absence or laxity of these ligaments leads to the migration of the spleen from its normal location to the pelvic region [ 1 ]. This condition is referred to as a wandering spleen, which is a rare condition. It is estimated that the incidence of wandering spleen is 0.2%, with fewer than 500 cases reported in the literature [ 2 ]. The wandering spleen may be due to congenital or acquired laxity of the ligaments. Due to hormonal factors, this condition is more common among women, particularly in multiparous women. Here, we present a case of a wandering spleen in a middle-aged man who presented with intermittent abdominal pain and underwent a successful splenopexy procedure. The clinical manifestations of the wandering spleen are variable, as it may be asymptomatic or present with acute abdomen due to splenic torsion [ 3 ].
Case presentation
We present a case of a 42-year-old man who presented to the emergency department complaining of abdominal pain for one day. He reported that the pain was generalized and had a sudden onset. The pain was sharp in nature with no radiations. It was associated with nausea and vomiting. However, the pain was not related to food intake. The patient could not identify any aggravating factors. The pain was partially alleviated by the use of nonsteroidal anti-inflammatory drugs. He rated the pain as 7 out of 10 on a 10-point severity scale. The patient reported similar, but milder, episodes of such pain over the past six months that had spontaneous resolution. The past medical history of the patient was remarkable for hypertension, diabetes mellitus, and peptic ulcer disease. The patient did not undergo any previous surgery. The patient had multiple visits to the emergency department over the last five years for intermittent abdominal pain that was clinically diagnosed as gastritis. The medication history included metformin 1000 mg, amlodipine 5 mg, and omeprazole 40 mg daily. The family history was remarkable for colon cancer in his father who was diagnosed at 50 years of age.
On physical examination, the patient appeared in severe pain. There were no signs of respiratory distress. The vital signs included a respiratory rate of 15 breaths/minute, pulse rate of 110 beats/minute, blood pressure of 136/90 mmHg, and a temperature of 37.1°C (measured by oral route). Abdominal examination revealed a distended abdomen with generalized tenderness. The patient had diffuse guarding and rigidity, suggesting peritonitis. The bowel sounds had normal intensity and quality. Examination of the cardiac and respiratory systems was normal. The laboratory findings showed no significant abnormalities. Considering the patient's history of peptic ulcer disease, the provisional diagnosis was a perforated peptic ulcer disease. Hence, the patient was referred to have a computed tomography scan of the abdomen.
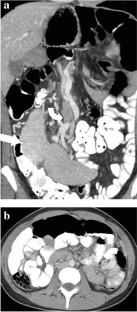
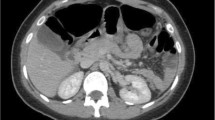
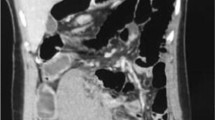
The computed tomography scan was performed after oral and intravenous contrast administration. The scan revealed the absence of the spleen in the expected normal location and showed a homogeneous pelvic mass of similar attenuation to that of the normal spleen. There were no hypodense lesions within the mass to suggest infarction. The supplying artery was patent. Such findings represented the diagnosis of a wandering spleen (Figures (Figures1, 1 , ,2 2 ).

Subsequently, the patient underwent laparotomy with a midline incision under general anesthesia. During exploration, the spleen was seen on the right side of the abdomen and measured 12 x 14 x 9 cm in maximum dimensions. The spleen appeared viable with no evidence of torsion or gangrene. The spleen was placed at its anatomical position and fixed with absorbable mesh. The operation was uncomplicated. The patient tolerated the procedure and had an uneventful recovery. The patient was discharged on the seventh postoperative day in good condition. He required this length of stay as the patient could not fully tolerate oral intake before the fifth postoperative day due to nausea.
We presented a rare case of wandering spleen in a middle-aged man who presented with a history of intermittent abdominal pain. Wandering spleen, also known as the hypermobile spleen, refers to the abnormal increase in mobility of the spleen so that it migrates from its normal position in the left hypochondriac fossa because of excessively long splenic pedicles and improper fixation of the splenic tissue to the underlying posterior abdominal wall [ 4 , 5 ]. The first case of wandering spleen was reported by Von Horne in 1667 [ 4 ]. It is reported that less than 600 cases of wandering spleen have been reported to date [ 6 ].
The wandering spleen may occur due to congenital or acquired etiologies. The congenital form involves the absent formation of the suspensory ligaments of the spleen. The spleen forms from the dorsal mesogastrium, which then rotates to the left side. The absence of suspensory ligaments results in long splenic pedicles, which are responsible for the increased mobility of the spleen. Furthermore, hypermobile colon and prune-belly syndrome are classic causes of the congenital wandering spleen. The acquired form of the wandering spleen has the same pathology of abnormal long splenic pedicles. The acquired form typically occurs in women of reproductive age, due to maternal hormones. It was found that both estrogen and progesterone increased the relaxin receptors on cells, promoting their action of increased ligamentous laxity [ 7 ]. Therefore, multiparous women are more prone to develop acquired wandering spleen. Nearly one-third of patients with wandering spleen present during childhood. Prepuberty and wandering spleen have equal gender preponderance. In adults, the prevalence of wandering spleen is much higher among women [ 1 , 3 ]. In the present case, the diagnosis of wandering spleen was unusual since the patient was male and had no identifiable risk factors [ 5 ].
The clinical manifestations of the wandering spleen are variable. The wandering spleen can be asymptomatic and found incidentally on physical examination or radiological investigations. It may also present with acute abdominal pain due to a splenic infarct. Furthermore, as in our case, the wandering spleen may present with intermittent abdominal pain that may be related to intermittent torsion and spontaneous detorsion of the splenic pedicle. Interestingly, our patient was clinically misdiagnosed as having gastritis and was on proton pump therapy for years. This highlights the importance of doing proper endoscopic and radiological investigations in patients with vague abdominal pain and not using an empiric treatment for common conditions without appropriate investigations. Acute presentations of the wandering spleen are likely due to torsion or mass effects on adjacent structures, causing intestinal obstruction, gastric volvulus, or pancreatitis [ 5 ]. The differential diagnosis of the wandering spleen depends on its presentation. For example, the differential diagnosis in patients with acute torsion includes ovarian torsion, acute appendicitis, and intestinal obstruction [ 5 ]. The presence of long splenic pedicles, which carry the blood supply to the spleen, predisposes to torsion of the pedicle leading to a partial or complete splenic infraction. Furthermore, the risk of torsion is aggravated if the spleen weight is greater than 500 grams [ 2 ].
The clinical diagnosis of a wandering spleen can be challenging, but the diagnosis can readily be made by cross-sectional imaging investigations. A computed tomography scan of the abdomen can demonstrate the absence of a spleen in its normal position in the left upper quadrant of the abdomen along with the presence of a mass in the lower abdominopelvic cavity that has similar attenuation to that of the normal splenic tissue. It can confirm the diagnosis and also identify the potential complications (e.g. splenic infarct). Ultrasound is another modality to diagnose the wandering spleen, as it is an affordable investigation and has no association with radiation risks. However, it is operator-dependent and its diagnostic accuracy is degraded by bowel gases, which may obscure the findings. In the present case, the patient underwent a computed tomography scan for a presumed diagnosis of perforated viscus given the findings of the clinical examination.
Surgical treatment is the only recommended management for wandering spleen [ 4 ]. Splenectomy is often required in cases of splenic torsion with infarction [ 3 ]. It may also be advised in the massive wandering spleen that cannot have splenopexy [ 4 ]. In other situations, splenic preservation with splenopexy should be attempted to avoid the future risks of overwhelming post-splenectomy sepsis [ 1 ]. Surgical treatment is needed even in asymptomatic patients because the rate of complications is substantial [ 4 , 5 ]. Laparoscopic splenopexy may also be used currently [ 8 ]. Conservative management is not advised, as it is associated with a complication rate that exceeds 50% [ 6 ].
Conclusions
A wandering spleen is a rare medical condition that poses a clinical diagnostic challenge and requires a high index of suspicion. Cross-sectional imaging studies can readily confirm the diagnosis and identify the possible complications. Surgical treatment, preferably with splenopexy, should be performed even in mildly symptomatic patients to prevent the complication of torsion and infarction. The diagnosis of the wandering spleen should be considered in patients with recurrent abdominal pain.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Ministry of Health Ethics Committee issued approval Exempt. Case reports are waived by the institutional review committee. Informed consent was obtained from the patient for the publication of this case report.
Wandering spleen: anatomic and radiologic considerations
Affiliation.
- 1 Department of Surgery, Carlos Center for Surgical Anatomy and Technique, Emory University School of Medicine, Atlanta, GA 30322.
- PMID: 1411739
- DOI: 10.1097/00007611-199210000-00011
Wandering spleen is a rare clinical entity and remains an elusive clinical diagnosis, particularly in the pediatric patient. Among the imaging modalities (computerized tomography, magnetic resonance imaging, nuclear medicine, ultrasonography, plain films) used in the diagnosis of wandering spleen, ultrasonography is the least invasive and most effective. Elective splenopexy remains the treatment of choice when the diagnosis is made before splenic infarction. We present two cases of wandering spleen manifested as a lower abdominal mass, and we discuss the surgical anatomy of the spleen and splenic ligaments and the hypothetical responsibility of these ligaments for the genesis of this clinical entity.
Publication types
- Case Reports
- Congenital Abnormalities* / diagnosis
- Congenital Abnormalities* / embryology
- Congenital Abnormalities* / pathology
- Ligaments / anatomy & histology
- Ligaments / embryology
- Ligaments / pathology
- Magnetic Resonance Imaging
- Radionuclide Imaging
- Spleen / abnormalities*
- Tomography, X-Ray Computed
- Ultrasonography

Wandering Spleen
Wandering spleen can be found on imaging studies as a spleen that is located somewhere other than it’s usual position in the left upper abdomen. This article will discuss diagnosis, complications and treatment of wandering spleen.
What is Wandering Spleen?
A wandering spleen, also known as a floating spleen or splenoptosis, is a condition where the spleen migrates from its usual position in the upper left abdomen. The spleen is a crucial organ involved in filtering blood and fighting infections.
In individuals with a wandering spleen, the ligaments that hold the spleen in place are either elongated or weakened, allowing it to move freely within the abdomen. This mobility can lead to various health issues, including abdominal pain, bloating, and in severe cases, spleen torsion or infarction, where the blood supply to the spleen is cut off, leading to tissue death.
Symptoms of Wandering Spleen
The symptoms of a wandering spleen can vary widely from person to person. Some individuals may not experience any symptoms at all, while others may have noticeable signs. Common symptoms include:
– **Abdominal pain or discomfort:** Often reported in the lower abdomen and may vary in intensity. – **A palpable mass:** Some patients may feel a movable lump in their abdomen. – **Gastrointestinal symptoms:** Such as bloating, constipation, or indigestion.
In cases where the spleen becomes twisted (torsion), symptoms can quickly escalate to sharp abdominal pain, vomiting, and fever, necessitating immediate medical attention.
Causes and Risk Factors
The exact cause of a wandering spleen is not always clear, but it is often related to the weakening or malformation of the ligaments that secure the spleen. This condition can be congenital (present at birth) or acquired due to injury, pregnancy, or previous abdominal surgeries. Factors that may increase the risk of developing a wandering spleen include:
– **Ligamentous laxity:** Natural or acquired looseness of the ligaments. – **Trauma:** Abdominal injuries that may damage spleen ligaments. – **Pregnancy and childbirth:** Hormonal changes and physical strain can weaken abdominal structures.
Diagnosis of Wandering Spleen
Diagnosing a wandering spleen involves a combination of physical examinations, medical history, and imaging tests. Physicians may initially suspect the condition based on symptoms and a physical exam. Diagnostic imaging, such as ultrasound, CT scans, or MRI, plays a crucial role in confirming the diagnosis by visually locating the spleen’s position and assessing its condition.
Treatment Options
The treatment for a wandering spleen depends on the severity of the symptoms and the overall health of the patient. Options include:
– **Observation:** In asymptomatic cases, regular monitoring may be recommended. – **Surgical intervention:** For symptomatic patients, surgery is often necessary. The two main surgical options are: – **Splenopexy:** Reattaching the spleen to its correct position using synthetic materials or tissue. – **Splenectomy:** Removal of the spleen, typically reserved for cases where the spleen is damaged or has become necrotic.
Post-Treatment Care and Considerations
After treatment for a wandering spleen, patients will need to follow up with their healthcare provider for regular check-ups. If the spleen was removed, vaccinations against certain bacteria may be recommended since the spleen plays a critical role in fighting infections. Patients who undergo splenopexy should avoid activities that may risk abdominal trauma to prevent recurrence.
A wandering spleen is a rare condition that can lead to significant health issues if not properly addressed. Understanding the symptoms, causes, and available treatment options is important for anyone diagnosed with this condition. With timely and appropriate medical care, individuals with a wandering spleen can lead healthy and active lives. Always consult with a healthcare provider for an accurate diagnosis and personalized treatment plan tailored to your specific needs.
Similar Posts
Colonic anastamosis.
Please read the disclaimer Medical imaging, specifically through techniques like CT (Computed Tomography) and MRI (Magnetic Resonance Imaging), plays a pivotal role in the evaluation and monitoring of colonic anastomosis….
Liver Cirrhosis On Ultrasound, CT, MRI
Please read the disclaimer Liver cirrhosis is a serious medical condition that affects the liver’s ability to function properly. Detecting cirrhosis at an early stage is crucial for effective treatment…
Does Fat Stranding On CT Mean Infection?
Please read the disclaimer Fat stranding on CT means that the fat which is ordinarily dark and uniform becomes dirty looking with brighter patchy areas. This can happen for many…
Pancreatic Adenocarcinoma on CT
Please read the disclaimer Pancreatic adenocarcinoma is the most common cancer of the pancreas having a very poor prognosis. Pancreatic cancer is most commonly diagnosed when a patient gets a…
Pancreatic Necrosis
Please read the disclaimer Pancreatic necrosis is a severe condition that affects the pancreas, an essential organ in the digestive system. This guide aims to provide information about pancreatic necrosis,…
Diverting Loop Ileostomy
Please read the disclaimer A diverting loop ileostomy is a surgical procedure often performed to give the lower part of the intestine time to heal. This operation involves bringing a…

IMAGES
VIDEO
COMMENTS
Clinical presentation. A wandering spleen can be an elusive diagnosis as its presentation is greatly variable and intermittent torsion can cause non-specific signs and symptoms. It can present as an asymptomatic or painful abdominal mass, intermittent abdominal pain, or as an acute abdomen (e.g. bowel obstruction, acute pancreatitis) 3,4,6.
Case Discussion. Wandering spleen results from abnormality of the suspensory ligaments of the spleen, namely the gastrosplenic and lienorenal ligaments. There may either be a congenital absence or underdevelopment of these ligaments, or an acquired laxity. The resultant elongated splenic pedicle predisposes to splenic torsion and infarct.
Wandering spleen is a rare condition that raises the possibility of splenic torsion. It is usually discovered in 20~40 years and is more common in women. Treatment of uncomplicated cases is by splenopexy.
Wandering spleen is a rare clinical entity seen mainly in male infants or women of reproductive age group (20-40 years), in which spleen is present at an ectopic location. [ 5, 6] This has been attributed to the laxity of splenic ligaments which can be congenital or an acquired weakness due to hormonal changes or multiple pregnancies. [ 7, 8, 9 ...
Wandering spleen is most commonly diagnosed in young children as well as women between the ages of 20 and 40. Even so, the disease is very rare and fewer than 500 occurrences of the disease have been reported as of 2005, [3] of which around 148 (including both children and adult cases) were documented to have been from between 1960 and 1992. [4]
Wandering spleen results from abnormality of the suspensory ligaments of the spleen, namely the gastrosplenic and lienorenal ligaments. There may either be a congenital absence or underdevelopment of these ligaments, or an acquired laxity. The re...
Wandering spleen is a rare clinical condition found in less that 0.5% of splenectomies that is characterized by ectopic positioning of the spleen within the abdomen or pelvis . The first description of this entity is attributed to Van Horne, a Dutch physician in 1667 with confirmation by autopsy . Soleimani et al performed an extensive review ...
Wandering spleen is a rare condition in which the spleen migrates from its usual anatomical position, commonly to the lower abdomen or pelvis. Wandering spleen is rare, with a reported incidence of <0.5%. It can present as an asymptomatic or pai...
Wandering spleen (or ectopic spleen) is a rare anomaly resulting from hyperlaxity or even absence of the ligaments that hold the spleen in its anatomical position. Although more frequently a congenital condition, it can also be acquired. Torsion of the vascular pedicle is its potential main complication with subsequent development of splenic infarct. In this paper we will describe the ...
Wandering spleen or hypermobile spleen results from the elongation or maldevelopment of the spleen's suspensory ligaments. It is a rare clinical entity that mainly affects children. Among adults, it is most commonly found in females of active reproductive age. It may present as an asymptomatic mass in the abdomen, or it may present with ...
Wandering spleen is a rare entity in which the spleen is hypermobile and ectopic in position, and attached only by an elongated vascular pedicle which becomes prone to torsion. Wandering spleen is found in less than 0.5% of splenectomies and occurs mainly in children and women aged 20-40 years [ 4 ]. This condition is a result of congenital ...
The wandering spleen, wandering liver, and wandering kidney are rare diagnoses that can be asymptomatic or are associated with nonspecific symptoms, making the clinical diagnosis elusive. In addition, given the small number of cases, these conditions are not well understood. Major complications of wandering spleen result from torsion of the vascular pedicle with resultant ischemia, physiologic ...
Eight cases of wandering spleen demonstrate that this rare entity has a characteristic constellation of findings which, though nonspecific, are highly suggestive of the diagnosis. Angiography or isotopic imaging specific for the spleen confirms the diagnosis. Asymptomatic patients may be carefully observed, with the institution of splenectomy should signs of torsion develop.
Abdelmonem H, Wandering spleen. Case study, Radiopaedia.org (Accessed on 22 Mar 2024) https://doi.org/10.53347/rID-59618
To report the CT features of wandering spleen, a rare condition which can be incidentally detected as an abdominal or pelvic mass or can present with torsion, ... Torsion of the spleen and associated 'prune belly syndrome'. A case report and review of the literature. S Afr Med J. 1978; 53: 637-639.
The absence or laxity of these ligaments leads to the migration of the spleen from its normal location to the pelvic region [ 1 ]. This condition is referred to as a wandering spleen, which is a rare condition. It is estimated that the incidence of wandering spleen is 0.2%, with fewer than 500 cases reported in the literature [ 2 ].
Wandering spleen is a rare clinical entity and remains an elusive clinical diagnosis, particularly in the pediatric patient. Among the imaging modalities (computerized tomography, magnetic resonance imaging, nuclear medicine, ultrasonography, plain films) used in the diagnosis of wandering spleen, ultrasonography is the least invasive and most effective.
820 Jorie Blvd., Suite 200 Oak Brook, IL 60523-2251 U.S. & Canada: 1-877-776-2636 Outside U.S. & Canada: 1-630-571-7873
A wandering spleen, also known as a floating spleen or splenoptosis, is a condition where the spleen migrates from its usual position in the upper left abdomen. The spleen is a crucial organ involved in filtering blood and fighting infections. In individuals with a wandering spleen, the ligaments that hold the spleen in place are either ...