
TYLER S. ROGERS, MD, MBA, FAAFP, AND BRENDAN LUSHBOUGH, DO, Martin Army Community Hospital, Fort Benning, Georgia
Am Fam Physician. 2023;107(2):187-190
Author disclosure: No relevant financial relationships.

Key Clinical Issue
What are the risks and benefits of less frequent antenatal in-person visits vs. traditional visit schedules and televisits replacing some in-person antenatal appointments?
Evidence-Based Answer
Compared with traditional schedules of antenatal appointments, reducing the number of appointments showed no difference in gestational age at birth (mean difference = 0 days), likelihood of being small for gestational age (odds ratio [OR] = 1.08; 95% CI, 0.70 to 1.66), likelihood of a low Apgar score (mean difference = 0 at one and five minutes), likelihood of neonatal intensive care unit (NICU) admission (OR = 1.05; 95% CI, 0.74 to 1.50), maternal anxiety, likelihood of preterm birth (nonsignificant OR), and likelihood of low birth weight (OR = 1.02; 95% CI, 0.82 to 1.25). (Strength of Recommendation [SOR]: B, inconsistent or limited-quality patient-oriented evidence.) Studies comparing hybrid visits (i.e., televisits and in-person) with in-person visits only did not find differences in rates of preterm births (OR = 0.93; 95% CI, 0.84 to 1.03; P = .18) or rates of NICU admissions (OR = 1.02; 95% CI, 0.82 to 1.28). (SOR: B, inconsistent or limited-quality patient-oriented evidence.) There was insufficient evidence to assess other outcomes. 1
Practice Pointers
Antenatal care is a cornerstone of obstetric practice in the United States, and millions of patients receive counseling, screening, and medical care in these visits. 2 , 3 There is clear evidence supporting the benefits of antenatal care; however, the number of appointments needed and setting of visits is less understood.
The American College of Obstetricians and Gynecologists recommends antenatal visits every four weeks until 28 weeks' gestation, every two weeks until 36 weeks' gestation, and weekly thereafter, which typically involves 10 to 12 visits. 4
Expert consensus and past meta-analyses have favored fewer antenatal care visits given similar maternal and neonatal outcomes. In 1989, the U.S. Public Health Service suggested a reduction in the antenatal visit schedule based on a multidisciplinary panel and expert opinion in conjunction with a literature review; however, the American College of Obstetricians and Gynecologists has not updated its guidelines, and practices have not changed. 5 A 2010 Cochrane review found no differences in perinatal mortality between patients randomized to higher vs. reduced antenatal care groups in high-income countries, and a 2015 Cochrane review showed no difference in neonatal outcomes for women in high-income countries. 6 , 7
The Agency for Healthcare Research and Quality (AHRQ) review showed moderate- and low-strength evidence and did not find significant differences between traditional and abbreviated schedules when looking at many outcomes, such as gestational age at birth, low birth weight, Apgar scores, NICU admission, preterm birth, and maternal anxiety. The review was limited by a small evidence base with studies that are difficult to compare. The randomized controlled trials that were eligible were adjusted for confounding, whereas the nonrandomized controlled studies were not adjusted and were at high risk for confounding.
Telemedicine, defined as the use of electronic information and telecommunication to support health care among patients, clinicians, and administrators, is a new option for antenatal care delivery. 8 Televisits, the real-time communication between patients and clinicians via phone or the internet, are the specific interactions that encompass telemedicine. Recent literature suggests that supplementing in-person visits with televisits in low-risk pregnancies resulted in similar clinical outcomes and higher patient satisfaction scores. 9 The AHRQ review found no significant differences between rates of preterm births or NICU admissions for a hybrid model of televisits and in-person visits compared with in-person visits only. The review was limited due to the lack of adjustments for potential confounders in the study. For example, some of the studies were conducted during the COVID-19 pandemic, which adds multiple confounders and potential for bias.
The AHRQ review offers limited opportunity for conclusions to suggest changes in current practice. The current evidence supports past evidence, suggesting that fewer visits are not associated with neonatal or maternal harm, and televisits may have a role in antenatal care. Many of the other outcomes of interest had insufficient evidence to generate conclusions.
Editor's Note: American Family Physician SOR ratings are different from the AHRQ Strength of Evidence ratings.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, the U.S. Department of Defense, or the U.S. government.
For the full review, go to https://effectivehealthcare.ahrq.gov/sites/default/files/product/pdf/cer-257-antenatal-care.pdf .
Balk EM, Konnyu KJ, Cao W, et al. Schedule of visits and televisits for routine antenatal care: a systematic review. Comparative effectiveness review no. 257. (Prepared by the Brown Evidence-Based Practice Center under contract no. 75Q80120D00001.) AHRQ publication no. 22-EHC031. Agency for Healthcare Research and Quality; June 2022. Accessed October 1, 2022. https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/cer-257-antenatal-care-evidence-summary.pdf
Kirkham C, Harris S, Grzybowski S. Evidence-based prenatal care: part I. General prenatal care and counseling issues. Am Fam Physician. 2005;71(7):1307-1316.
Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
Kriebs JM. Guidelines for perinatal care, sixth edition: by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. J Midwifery Womens Health. 2010;55(2):e37.
Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77(5):782-787.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010(10):CD000934.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015(7):CD000934.
Fatehi F, Samadbeik M, Kazemi A. What is digital health? Review of definitions. Stud Health Technol Inform. 2020;275:67-71.
Cantor AG, Jungbauer RM, Totten AM, et al. Telehealth strategies for the delivery of maternal health care: a rapid review. Ann Intern Med. 2022;175(9):1285-1297.
The Agency for Healthcare Research and Quality (AHRQ) conducts the Effective Health Care Program as part of its mission to produce evidence to improve health care and to make sure the evidence is understood and used. A key clinical question based on the AHRQ Effective Health Care Program systematic review of the literature is presented, followed by an evidence-based answer based on the review. AHRQ’s summary is accompanied by an interpretation by an AFP author that will help guide clinicians in making treatment decisions.
This series is coordinated by Joanna Drowos, DO, MPH, MBA, contributing editor. A collection of Implementing AHRQ Effective Health Care Reviews published in AFP is available at https://www.aafp.org/afp/ahrq .
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition. Geneva: World Health Organization; 2015.

Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition.
C antenatal care.
- Always begin with Rapid assessment and management (RAM) B3-B7 . If the woman has no emergency or priority signs and has come for antenatal care, use this section for further care.
- Next use the Pregnancy status and birth plan chart C2 to ask the woman about her present pregnancy status, history of previous pregancies, and check her for general danger signs. Decide on an appropriate place of birth for the woman using this chart and prepare the birth and emergency plan. The birth plan should be reviewed during every follow-up visit.
- Check all women for pre-eclampsia, anaemia, syphilis and HIV status according to the charts C3 - C6 .
- In cases where an abnormal sign is identified (volunteered or observed), use the charts Respond to observed signs or volunteered problems C7 - C11 to classify the condition and identify appropriate treatment(s).
- Give preventive measures due C12 .
- Develop a birth and emergency plan C14-C15 .
- Advise and counsel on nutrition C13 , family planning C16 , labour signs, danger signs C15 , routine and follow-up visits C17 using Information and Counselling sheets M1 -M19 .
- Record all positive findings, birth plan, treatments given and the next scheduled visit in the home-based maternal card/clinic recording form.
- Assess eligibility of ART for HIV-infected woman C19 .
- If the woman is HIV infected, adolescent or has special needs, see G1 - G11 H1 - H4 .
C2. ASSESS THE PREGNANT WOMAN: PREGNANCY STATUS, BIRTH AND EMERGENCY PLAN
Use this chart to assess the pregnant woman at each of the four antenatal care visits. During first antenatal visit, prepare a birth and emergency plan using this chart and review them during following visits. Modify the birth plan if any complications arise.
View in own window

C3. CHECK FOR PRE-ECLAMPSIA
Screen all pregnant women at every visit.
C4. CHECK FOR ANAEMIA
C5. check for syphilis.
Test all pregnant women at first visit. Check status at every visit.
C6. CHECK FOR HIV STATUS
Test and counsel all pregnant women for HIV at the first antenatal visit. Check status at every visit.
If no problem, go to page C12 .
C7-C11. RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
C12. give preventive measures.
Advise and counsel all pregnant women at every antenatal care visit.
C13. ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE AND SUBSTANCE ABUSE
Use the information and counselling sheet to support your interaction with the woman, her partner and family.
Counsel on nutrition
- Advise the woman to eat a greater amount and variety of healthy foods, such as meat, fish, oils, nuts, seeds, cereals, beans, vegetables, cheese, milk, to help her feel well and strong (give examples of types of food and how much to eat).
- Spend more time on nutrition counselling with very thin, adolescent and HIV-infected woman.
- Determine if there are important taboos about foods which are nutritionally important for good health. Advise the woman against these taboos.
- Talk to family members such as the partner and mother-in-law, to encourage them to help ensure the woman eats enough and avoids hard physical work.
Advise on self-care during pregnancy
Advise the woman to:
- Take iron tablets F3 .
- Rest and avoid lifting heavy objects.
- Sleep under an insecticide impregnated bednet.
- Counsel on safer sex including use of condoms, if at risk for STI or HIV G2 .
- Avoid alcohol and smoking during pregnancy.
- NOT to take medication unless prescribed at the health centre/hospital.
Counsel on Substance Abuse:
- Avoid tobacco use during pregnancy.
- Avoid exposure to second-hand smoke.
- Do not take any drugs or Nicotine Replacement Therapy for tobacco cessation.
Counsel on alcohol use:
- Avoid alcohol during pregnancy.
Counsel on drug use:
- Avoid use of drugs during pregnancy.
C14-C15. DEVELOP A BIRTH AND EMERGENCY PLAN
Facility delivery.
Explain why birth in a facility is recommended
- Any complication can develop during delivery - they are not always predictable.
- A facility has staff, equipment, supplies and drugs available to provide best care if needed, and a referral system.
- If HIV-infected she will need appropriate ARV treatment for herself and her baby during childbirth.
- Complications are more common in HIV-infected women and their newborns. HIV-infected women should deliver in a facility.
Advise how to prepare
Review the arrangements for delivery:
- How will she get there? Will she have to pay for transport?
- How much will it cost to deliver at the facility? How will she pay?
- Can she start saving straight away?
- Who will go with her for support during labour and delivery?
- Who will help while she is away to care for her home and other children?
Advise when to go
- If the woman lives near the facility, she should go at the first signs of labour.
- If living far from the facility, she should go 2-3 weeks before baby due date and stay either at the maternity waiting home or with family or friends near the facility.
- Advise to ask for help from the community, if needed I2 .
Advise what to bring
- Home-based maternal record.
- Clean cloths for washing, drying and wrapping the baby.
- Additional clean cloths to use as sanitary pads after birth.
- Clothes for mother and baby.
- Food and water for woman and support person.
Home delivery with a skilled attendant
- Review the following with her:
- Who will be the companion during labour and delivery?
- Who will be close by for at least 24 hours after delivery?
- Who will help to care for her home and other children?
- Advise to call the skilled attendant at the first signs of labour.
- Advise to have her home-based maternal record ready.
Explain supplies needed for home delivery
- Warm spot for the birth with a clean surface or a clean cloth.
- Clean cloths of different sizes: for the bed, for drying and wrapping the baby, for cleaning the baby's eyes, for the birth attendant to wash and dry her hands, for use as sanitary pads.
- Buckets of clean water and some way to heat this water.
- Bowls: 2 for washing and 1 for the placenta.
- Plastic for wrapping the placenta.
Advise on labour signs
Advise to go to the facility or contact the skilled birth attendant if any of the following signs:
- a bloody sticky discharge.
- painful contractions every 20 minutes or less.
- waters have broken.
Advise on danger signs
Advise to go to the hospital/health centre immediately, day or night, WITHOUT waiting if any of the following signs:
- vaginal bleeding.
- convulsions.
- severe headaches with blurred vision.
- fever and too weak to get out of bed.
- severe abdominal pain.
- fast or difficult breathing.
- She should go to the health centre as soon as possible if any of the following signs:
- abdominal pain.
- swelling of fingers, face, legs.
Discuss how to prepare for an emergency in pregnancy
where will she go?
how will they get there?
how much it will cost for services and transport?
can she start saving straight away?
who will go with her for support during labour and delivery?
who will care for her home and other children?
- Advise the woman to ask for help from the community, if needed I1 – I3 .
- Advise her to bring her home-based maternal record to the health centre, even for an emergency visit.
C16. ADVISE AND COUNSEL ON FAMILY PLANNING
Counsel on the importance of family planning.
- If appropriate, ask the woman if she would like her partner or another family member to be included in the counselling session.
Ask about plans for having more children. If she (and her partner) want more children, advise that waiting at least 2 years before trying to become pregnant again is good for the mother and for the baby's health.
Information on when to start a method after delivery will vary depending whether a woman is breastfeeding or not.
Make arrangements for the woman to see a family planning counsellor, or counsel her directly (see the Decision-making tool for family planning providers and clients for information on methods and on the counselling process).
- Counsel on safer sex including use of condoms for dual protection from sexually transmitted infections (STI) or HIV and pregnancy. Promote especially if at risk for STI or HIV G4 .
- For HIV-infected women, see G4 for family planning considerations
- Her partner can decide to have a vasectomy (male sterilization) at any time.
Method options for the non-breastfeeding woman
Special considerations for family planning counselling during pregnancy.
Counselling should be given during the third trimester of pregnancy.
can be performed immediately postpartum if no sign of infection (ideally within 7 days, or delay for 6 weeks).
plan for delivery in hospital or health centre where they are trained to carry out the procedure.
ensure counselling and informed consent prior to labour and delivery.
can be inserted immediately postpartum if no sign of infection (up to 48 hours, or delay 4 weeks)
plan for delivery in hospital or health centre where they are trained to insert the IUD.
Method options for the breastfeeding woman
C17. advise on routine and follow-up visits.
Encourage the woman to bring her partner or family member to at least 1 visit.
Routine antenatal care visits
- All pregnant women should have 4 routine antenatal visits.
- First antenatal contact should be as early in pregnancy as possible.
- During the last visit, inform the woman to return if she does not deliver within 2 weeks after the expected date of delivery.
- More frequent visits or different schedules may be required according to national malaria or HIV policies.
- If women is HIV-infected ensure a visit between 26-28 weeks.
Follow-up visits
C18. home delivery without a skilled attendant.
Reinforce the importance of delivery with a skilled birth attendant
Instruct mother and family on clean and safer delivery at home
If the woman has chosen to deliver at home without a skilled attendant, review these simple instructions with the woman and family members.
- Give them a disposable delivery kit and explain how to use it.
Tell her/them:
- To ensure a clean delivery surface for the birth.
- To ensure that the attendant should wash her hands with clean water and soap before/after touching mother/baby. She should also keep her nails clean.
- To, after birth, dry and place the baby on the mother's chest with skin-to-skin contact and wipe the baby's eyes using a clean cloth for each eye.
- To cover the mother and the baby.
- To use the ties and razor blade from the disposable delivery kit to tie and cut the cord.The cord is cut when it stops pulsating.
- To wipe baby clean but not bathe the baby until after 6 hours.
- To wait for the placenta to deliver on its own.
- To start breastfeeding when the baby shows signs of readiness, within the first hour after birth.
- To NOT leave the mother alone for the first 24 hours.
- To keep the mother and baby warm.To dress or wrap the baby, including the baby's head.
- To dispose of the placenta in a correct, safe and culturally appropriate manner (burn or bury).
- Advise her/them on danger signs for the mother and the baby and where to go.
Advise to avoid harmful practices
For example:
not to use local medications to hasten labour.
not to wait for waters to stop before going to health facility.
NOT to insert any substances into the vagina during labour or after delivery.
NOT to push on the abdomen during labour or delivery.
NOT to pull on the cord to deliver the placenta.
NOT to put ashes, cow dung or other substance on umbilical cord/stump.
Encourage helpful traditional practices:
If the mother or baby has any of these signs, she/they must go to the health centre immediately, day or night, WITHOUT waiting
- Waters break and not in labour after 6 hours.
- Labour pains/contractions continue for more than 12 hours.
- Heavy bleeding after delivery (pad/cloth soaked in less than 5 minutes).
- Bleeding increases.
- Placenta not expelled 1 hour after birth of the baby.
- Very small.
- Difficulty in breathing.
- Feels cold.
- Not able to feed.
All rights reserved. Publications of the World Health Organization are available on the WHO website ( www.who.int ) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob ).
Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website ( www.who.int/about/licensing/copyright_form/en/index.html ).
- Cite this Page Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition. Geneva: World Health Organization; 2015. C, ANTENATAL CARE.
- PDF version of this title (2.6M)
In this Page
- ASSESS THE PREGNANT WOMAN: PREGNANCY STATUS, BIRTH AND EMERGENCY PLAN
- RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
- GIVE PREVENTIVE MEASURES
- ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE AND SUBSTANCE ABUSE
- DEVELOP A BIRTH AND EMERGENCY PLAN
- ADVISE AND COUNSEL ON FAMILY PLANNING
- ADVISE ON ROUTINE AND FOLLOW-UP VISITS
- HOME DELIVERY WITHOUT A SKILLED ATTENDANT
Other titles in this collection
- WHO Guidelines Approved by the Guidelines Review Committee
Recent Activity
- ANTENATAL CARE - Pregnancy, Childbirth, Postpartum and Newborn Care ANTENATAL CARE - Pregnancy, Childbirth, Postpartum and Newborn Care
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected] , [email protected]
Affiliation Maternal and Child Health Division, icddr,b, Dhaka, Bangladesh
Roles Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft
Roles Formal analysis, Investigation, Methodology, Software, Writing – original draft
Roles Formal analysis, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft
Roles Data curation, Investigation, Project administration, Validation, Writing – original draft
Roles Formal analysis, Project administration, Supervision, Validation
Roles Project administration, Resources, Validation, Writing – original draft
Roles Conceptualization, Formal analysis, Methodology, Writing – original draft
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing
Affiliation Department of Public Health, North South University, Dhaka, Bangladesh
Roles Conceptualization, Investigation, Methodology, Writing – review & editing
Affiliation Professor and Director of Centre of Excellence for Non-Communicable Disease, James P Grant School of Public Health, BRAC University, Dhaka, Bangladesh
- Bidhan Krishna Sarker,
- Musfikur Rahman,
- Tanjina Rahman,
- Tawhidur Rahman,
- Jubaida Jahan Khalil,
- Mehedi Hasan,
- Fariya Rahman,
- Anisuddin Ahmed,
- Dipak Kumar Mitra,

- Published: November 5, 2020
- https://doi.org/10.1371/journal.pone.0241185
- Reader Comments
There is dearth of information on the timeliness of antenatal care (ANC) uptake. This study aimed to determine the timely ANC uptake by a medically trained provider (MTP) as per the World Health Organization (WHO) recommendations and the country guideline.
Cross-sectional survey was done with 2,731 women having livebirth outcome in last one year in Dinajpur, Nilphamari and Rajshahi districts, Bangladesh from August-November,2016.
About 82%(2,232) women received at least one ANC from a MTP. Overall, 78%(2,142) women received 4 or more ANCs by any provider and 43%(1168) from a MTP. Only 14%(378) women received their first ANC at the 1 st trimester by a MTP. As per 4 schedule visits by the WHO FANC model and the country guideline 8%(203) and 20%(543) women respectively received the first 2 timely ANC by a MTP; where only 1%(32) and 3%(72) received the first 3 visits timely and 0.6%(17) and 1%(29) received all the four timely visits. Factors significantly associated with the first two timely visits are: 10 or above years of schooling of women [adj. OR 2.13 (CI: 1.05, 4.30)] and their husbands [adj. OR 2.40 (CI: 1.31, 4.38)], women’s employment [adj. OR 2.32 (CI: 1.43, 3.76)], urban residential status [adj. OR 3.49 (CI: 2.46, 4.95)] and exposure to mass media [adj. OR 1.58 (CI: 1.07, 2.34)] at 95% confidence interval. According to the 2016 WHO ANC model, only 1.5%(40) women could comply with the first two ANC contacts timely by a MTP and no one could comply with all the timely 8 contacts.
Despite high coverage of ANC utilization, timely ANC visit is low as per both the WHO recommendations and the country guideline. For better understanding, further studies on the timeliness of ANC coverage are required to design feasible intervention for improving maternal and child health.
Citation: Sarker BK, Rahman M, Rahman T, Rahman T, Khalil JJ, Hasan M, et al. (2020) Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh. PLoS ONE 15(11): e0241185. https://doi.org/10.1371/journal.pone.0241185
Editor: Kannan Navaneetham, University of Botswana, BOTSWANA
Received: November 19, 2019; Accepted: October 10, 2020; Published: November 5, 2020
Copyright: © 2020 Sarker et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting information files.
Funding: This study funded by Bill and Melinda Gates Foundation. The awarded BMGF grant number is OPP1146943. BKS received the funding. URL of funder website is https://www.gatesfoundation.org . The sponsors had no role in the study design, data collection and analysis, decision to publish and preparing manuscript.
Competing interests: The authors declare that they have no competing interests.
Introduction
Approximately, 300,000 women die annually from pregnancy or childbirth-related complications around the world and almost all of these deaths occur in low-resource settings, and most of these deaths are preventable [ 1 , 2 ]. The South Asian region alone accounts for approximately one-third of the global maternal and child deaths annually [ 3 ]. The global strategy for Women’s, Children’s and Adolescents’ Health under the Sustainable Development Goal (SDG) 3 has set the targets to reduce maternal mortality ratio (MMR) to less than 70 per 100,000 live births, and the neonatal mortality to 12 per 1,000 live births or lower by 2030 [ 4 ].
High coverage of quality Antenatal Care (ANC) can play a crucial role to decrease maternal and child mortality rates and achieve national and global targets related to maternal and child health [ 5 – 7 ]. Studies found ANC received from skilled provider reduces the risk of pregnancy complications and adverse pregnancy outcomes such as- stillbirths, intrauterine growth retardation, preterm births, low-birth weight, fetal abnormalities and other fetal complications, possibly mediated through health promotion, disease prevention, screening and treatment which increases maternal and newborn survival [ 2 , 8 – 15 ]. The study also emphasized on the timeliness of ANC to ensure healthy pregnancy outcomes [ 13 ].
As per the previous World Health Organization’s (WHO) recommended Focused Antenatal Care (FANC) Model; under normal circumstances, a pregnant woman should have at least four ANC visits [ 16 ]. Recently, WHO has issued “the 2016 WHO ANC model” with a new series of recommendations to improve the quality of ANC, which in turn help reducing the risk of stillbirths, complications and ensures a positive pregnancy experience. The new WHO model recommends a minimum of eight contacts. The 2016 WHO ANC Model covers 4+ ANC contacts that support the accomplishment of SDGs, which aims for reducing maternal and child mortality [ 6 , 17 , 18 ]. The 2016 WHO ANC model provides adequate knowledge to get prepared for birth or any complication, and lifesaving information for both mother and child as it reduces the delay of care-seeking for obstetric emergencies that contribute majority of the maternal mortality in a low-income area [ 7 ]. Though the recent 2016 WHO model recommends 8 contacts, the country guideline of Bangladesh still promotes 4 ANCs having slight time differences from the previously WHO recommended FANC model [ 19 , 20 ].
Globally, the coverage of early ANC visit within 14 weeks is reported to increase from 40.9% to 58.6% from the year 1990 to 2013 [ 21 ]. However, the uptake rate differs between developed and developing countries. In the year 2013, the rate of ANC uptake in developed and developing countries was 84.8% and 48.1% respectively [ 21 ].
According to the Bangladesh Demographic and Health Surveys (BDHS) the trend of ANC coverage by a medically trained provider (MTP) is increasing [ 16 , 22 – 24 ]. Since 2004 to 2017 (51%-82%) ANC coverage had increased by 31 point percentage [ 16 , 22 – 25 ]. The percentage of pregnant women who made four or more ANC visit by any provider has increased from 17% in 2004 to 47% in 2017 [ 22 – 24 ]. In terms of the ANC coverage, geographical and regional variation exist in Bangladesh where data from BDHS 2017-’18 shows at least one ANC by a MTP is the highest in the South-west region (Khulna division91%) and the lowest in the Northeast region (Sylhet division-71%) [ 24 ]. Besides, the Northern region (Rajshahi-85% and Rangpur-75%) and the Southeast region (Chattogram-83%) also showed a higher prevalence of at least one ANC uptake. However, this regional difference fluctuated quite often since the last decade [ 16 , 22 – 25 ].
Despite having a rise in ANC coverage in Bangladesh, it stands among the top ten countries those are contributing nearly 60% of global maternal mortality [ 26 , 27 ]. Maternal and neonatal mortality remained quite unchanged in the last few years [ 24 , 28 ]. Bangladesh Maternal Mortality and Health Care Survey (BMMS) shows the Maternal Mortality Ratio (MMR) is 196 per 100,000 live births in 2016 whereas it was 194 per 100,000 live births in 2010. Similar to maternal mortality, BDHS shows that neonatal deaths per 1,000 live births were 28 in 2014 and 30 in 2017–18 [ 16 , 24 , 28 , 29 ]. Bangladesh has the highest proportion of preterm births with 19% of births occurring before gestational weeks 37 [ 30 ]. The stillbirth rate in Bangladesh is 25.4 per 1,000 births [ 31 ]. According to BMMS 2016, the major causes behind the maternal deaths are hemorrhage (31%), eclampsia (24%), abortion (7%), obstructed/prolonged labor (3%), etc. [ 28 ]. To reduce pregnancy-related complications and adverse pregnancy outcomes, timely recommended ANC is imperative.
According to the BDHS-2017-18, less than 18% women received quality ANC care. Quality care is defined as receiving four or more antenatal visits, with at least one visit from a MTP and the components include measurement of weight and blood pressure, testing of blood and urine and receipt the information on potential danger signs during pregnancy [ 24 ]. In addition to the national survey, few other studies conducted in different parts of Bangladesh that also provide information of the total number of ANC visits that a woman receives during her pregnancy period [ 32 – 34 ]. However, none of the surveys showed how many women secured their visits timely as per WHO recommendations as well as a country guideline. So, there is a dearth of information in Bangladesh about the timeliness of ANC visits that a pregnant woman should adhere to WHO recommendations as well as to country guideline. It is essential to look deeper into the real status of the timely ANC uptake which has a greater impact on both mother and child’s odds of survival [ 32 , 35 ]. Therefore, we aimed to explore timely ANC uptake by MTPs as per the WHO recommendations and the country guideline from a cross-sectional survey in Northern Bangladesh.
Materials and methods
Study design and settings.
It was a community-based cross-sectional study conducted in both rural and urban areas. We had two study sites in rural areas and one in urban area from 3 northern districts of Bangladesh. Rural areas were Chirirbandar, a sub-district from Dinajpur and Saidpur, a sub-district from Nilphamari in Rangpur division and the urban area was Rajshahi City Corporation from Rajshahi division. According to the Population and Housing Census, the total population of Chirirbandar was 292,500, of which 146,619 were males, and 145,881 were female [ 36 ]. For Saidpur sub-district, the total population was 264,461, of which 133,737 were males, and 130,724 were females [ 37 ]. On the other hand, for Rajshahi City Corporation the total population was 449,756, of which 232,974 were males, and 216,782 were females [ 38 ]. According to census data, we found the female literacy rate was 42% in Dinajpur, whereas for both Nilphamari and Rajshahi, it was 39% [ 39 ]. In comparison to northern divisions (Rajshahi and Rangpur), southeast (Chattogram) and northeast (Sylhet) divisions had higher Maternal Mortality Ratio (Rajshahi-173/100,000 vs Chattogram-186/100,000 and Sylhet-425/100,000), Similar to maternal mortality, under-5Child Mortality Rate of Northern region (Rajshahi-43/1,000 and Rangpur-39/1,000) is lower than Southeast (Chattogram-50/1,000) and Northeast (Sylhet-67/1,000) regions [ 16 , 29 ].
Sampling and study participants
We applied two stages cluster sampling to select study participants in the study area. We considered some socio-demographic characteristics including age, years of schooling, occupation, religion, gravida and place of residence of study participants in the sampling frame to cover a range of information on similar issues from a variety of study participants. We considered government and non-government ‘Community-Based Health Workers’ (CBHW) catchment area as a cluster. We maintained similar population coverage for cluster selection. In Chirirbandar, we considered government CBHW’s catchment area, and for Saidpur and Rajshahi, we considered non-government CBHW’s areas as our clusters. In the first stage, we randomly selected one sub-district from two rural districts each and 10 wards (lowest administrative unit of city area) from the city corporation area. Then, we randomly selected 6 clusters (CBHW’s catchment area) out of 12 in Chirirbandar of Dinajpur district, 6 clusters out of 12 clusters in Saidpur of Nilphamari district and 6 clusters from 10 clusters in Rajshahi city area.
To recruit study participants, we applied the Expanded Program of Immunization method, which is a popular spatial sampling method named as the EPI method. We selected the starting point to start data collection in the selected cluster using the EPI method. We determined the midpoint of each cluster in consultation with the community people. To ensure the randomization process in interviewing eligible participants, we spun a bottle at the midpoint of each cluster to identify the direction from where we started searching study participants [ 40 , 41 ]. Interviewers visited every household on next door basis according to the direction of the bottle, and eligible participants were identified and interviewed. They collected data until the cluster’s sample size was met. During the household visit, if any eligible woman was absent, then data collectors tried at least two more times to interview her.
In each study area, around 900 women were interviewed, and finally, we completed 2731 interviews from the 3 study areas. Followings were the inclusion criteria for the study enrolment: (1) the woman had a live birth outcome in the last one year prior to interview (2) the woman passed 28 or more days after last delivery (3) the woman could hear, see and speak (4) the woman had permanent residence in the study area.
Data collection
We conducted this survey from August to November 2016. An expert research team from the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) was involved in preparing a survey tool based on the research question and objectives of the study. Study investigators trained all the data collectors on the data collection tool. After that, a field test was done as pre-testing to check the feasibility of the survey tool in the real field. We checked the consistency of the survey tool and incorporated the feedback into the final version after pre-testing. The survey was administered through face-to-face interviews with eligible women.
Data management and quality assurance
An efficient team with an experienced team leader was closely involved with the data collection for ensuring the quality data. The team leader checked the completeness of every interview on the spot after the data collection through day to day supervision. Furthermore, a project research physician (PRP) and a research investigator (RI) coordinated all the data collection teams and team leaders on a daily and weekly basis for ensuring quality data and completeness of the interview. Re-interview was done by the team leaders, PRP and RI in a significant amount to check the accuracy and validity of data. At the same time, a database template was designed by an expert programmer of the Maternal and Child Health Division (MCHD), icddr,b to enter all the data online. Dot net (Version-10) software was used for data template design as appropriate [ 42 ]. The data template was designed in such a way that while entering data, none of the variables could go missing. Skipping options were also maintained strictly and logically to avoid entry mistakes. The expert data management team entered all the data through an online database. During entering data, this team entered both pre-coded and postcoded data simultaneously. For post coding of data, the research team was also closely involved with the data management team.
This study had no more than minimal risk to study participants. We obtained written informed consent from each of the participants prior to the interviews. We received approval from the Institutional Review Board (IRB) of icddr,b before data collection in the field. All the participants were married, and there was no need for obtaining consent for the minors from the guardian or parents as per IRB.
All the information given by the mothers were self-reported, however, we found 27% had a pregnancy registration card (also known as ANC card) and we checked their documents for relevance. Rest of the women who did not have a pregnancy registration card, we applied the probing technique to get the actual information from them. We determined the timely ANC coverage with regards to the WHO and the country guidelines. The primary outcome variable was the first two timely ANC visits by a skilled provider as per the WHO FANC model. Our country guideline resembles with the WHO FANC model and did not yet adopt the WHO 2016 model [ 43 ]. We considered the uptake rate of the first two timely ANC visits by MTP as per the WHO FANC guideline. We collected numbers of ANC received by a woman and when as per gestational weeks; and the providers of ANC. To estimate the ANC uptake, we considered women who had received at least one ANC from any provider. If any woman reported that, she had more than one ANC in the same week from different service providers, then ANC by the highest qualified service provider was considered. We followed the criteria of skilled or unskilled provider from the Bangladesh Demographic and Health Survey (BDHS) and considered qualified doctor, nurse/midwife/paramedic, family welfare visitor (FWV) and community skilled birth attendant (CSBA) as skilled or MTP. We used skilled provider and MTP interchangeably [ 16 ].
To analyze the timely ANC visits, we followed the criteria suggested by the two WHO models and country guideline. According to “the WHO FANC model”, the timely ANC visits refer to the 1st ANC visit between 8–12 weeks of pregnancy, the 2 nd ANC visit between 24–26 weeks, the 3rd ANC visit at 32 nd week, and the 4th ANC Visit between 36–38 weeks of gestation [ 43 ].
The timely ANC visits recommended by “the WHO 2016 ANC model”, refers to 1st contact within 12 weeks, the 2nd contact at 20 th week, the 3rd contact at 26 th week, the 4th at 30 th week, the 5th at 34 th week, the 6th at 36 th week, the 7th at 38 th week and the 8th contact at 40 th week [ 43 ]. Like the WHO FANC model, the country guideline also suggests at least 4 scheduled ANC visits where the timely ANC visits refer to the 1st ANC visit within 16 weeks of pregnancy, the 2 nd ANC visit between 24–28 weeks, the 3rd ANC visit at 32 nd week, and the 4th ANC Visit at 36 th week of gestation [ 20 ].
There is a slight difference among the 2016 WHO ANC Model, the WHO FANC Model and the Bangladesh guideline for recommending the1st timing of ANC. The 2016 WHO ANC Model recommended within 12 weeks of gestation for the 1 st contact whereas the WHO FANC Model recommended the 1 st visit between 8–12 weeks of gestation and the Bangladesh guideline recommended the 1 st visit within 16 weeks of gestation.
All the guidelines mentioned about the exact timing and ranges depending on gestational age. The WHO FANC model suggests timing for 1 st , 2 nd and 4 th visits in ranges and 3 rd visit on the exact time of gestational age. The country guideline suggests timing for 1 st and 2 nd visits in ranges and 3 rd and 4 th visits on the exact time of gestational age. The recent WHO 2016 ANC model suggests only first contact in range of gestational weeks and remaining 7 contacts on the exact timing of gestational weeks.
We considered Anderson and Newman’s framework of health services utilization to select the covariates that are associated with ANC utilization. This framework consists of three individual determinants- i. Predisposing ii. Enabling iii. Illness level [ 44 , 45 ]. We adopted age, sex as demographic and years of schooling, religion, occupation, women’s partner years of schooling and his occupation as social structure from disposing factors. In addition to previous literature and known confounder, we included these socio-demographic characteristics such as age, religion, place of residence, years of schooling status, primary occupation, number of pregnancies and living children [ 32 , 33 , 46 ]. Regarding age and schooling, we considered completed years. Age was categorized into three different groups such as less than or equal to 19 years, 20 to 29 years and greater than or equal to 30 years. Similarly, years of schooling was categorized into four groups as 0 to 4 years, 5 to 7 years, 8 to 9 years and greater or equivalent to 10 years of schooling. If a woman and her husband had multiple occupations, the primary occupation was considered based on their preferences in terms of their income and time spent on that occupation. We took the information about the current occupation of the survey respondents. We ensured their primary occupation by asking “what is your primary occupation?”, “What kind of work do you mainly do?”, “Are you involved in any income generating activities?” during our interview. Point to be noted here, mothers who were on maternity leave their occupation was marked as employed during the period of data collection. The women who were housewives referred to as homemakers for their occupation. By gravida, we meant the total number of confirmed pregnancies that our participant had in her lifetime.
Statistical analysis
We performed statistical analysis using the statistical software package STATA version 13.1 [ 47 ]. To identify differences between the groups, we used the χ2 (Chi-square) test for categorical data and independent sample t-test for continuous data. We checked the linearity assumption between the predictor and the outcome variable. We found there was a non-linear relationship between the predictors and the outcome variable. Then we transformed the covariate (age and years of schooling) into categories. We estimated both unadjusted and adjusted odds ratio using simple and multiple logistic regression models considering different covariates (age, years of schooling, gravida, occupation and place of residence etc.) to see the effect of covariates on the first two timely visits by MTPs. Bivariate logistic regression analysis was conducted to examine the association between the predictor and outcome variables using the Crude Odds Ratio (COR) at a 95% confidence interval (CI). Factors that were significant with a p-value of less than 0.05 were considered for further estimation of the multiple logistic regression model. For example, the variable religion showed an insignificant relationship with the first two timely ANC visits and we excluded this variable from the regression analysis. Conventionally, p value of 0.05 is taken to indicate statistical significance. This 5% level is, however, an arbitrary minimum and p values should be much smaller to provide strong evidence. Before fitting the multiple logistic regression model, we did regression for the outcome of the first three and all four timely ANC visits by a medically trained provider, but almost all predictors were crudely insignificant for these two outcome variables separately. Furthermore, the number of observation was very low for the first three and all four timely visits by MTPs. Therefore, we considered the regression model for the first two timely visits by MTP according to the WHO FANC model.
“ Table 1 ” describes the socio-demographic characteristics of study participants living in both urban and rural areas. Result shows that almost two-third of the respondents (62%) belonged to the age group of 20 to 29 years and the majority of the respondents were Muslims (88%). A bit more than half of women (51%) passed grade 8 and higher. Years of schooling with 10 or more were higher among the respondents in the urban area (35%) than the rural area (26%). Overall, 95% of women were homemakers. In terms of the number of pregnancies, more than one-third of women (38%) had single gravida and the 50th percentile of respondents mentioned that they had experienced two pregnancies (median 2). Almost half of women’s husband had completed 8 or more years of schooling. About three-fourth of women (77%) had television exposure and only 11% of women read newspaper or magazine.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0241185.t001
Table 2 presents the ANC coverage of study participants by their place of residence. Almost all the women (98%) from both rural and urban sites received at least one ANC from any provider and overall 82% women (90% urban and 77% rural women) received at least one ANC from MTP. More than three-fourths of women (78%) had 4 or more ANCs by any provider while less than half of women (43%) received 4 or more ANC by a MTP. More than half of urban women (58%) and one-third of (35%) rural women reported to have received four or more ANC from MTP. However, about 17% of women received eight or more contacts by any provider and only 4% women received eight or more contacts from MTPs. Urban women (10%) were more likely to receive 8 or more ANC by MTPs than rural women (1%).
https://doi.org/10.1371/journal.pone.0241185.t002
Fig 1 shows women received their 1 st ANC visit by gestational weeks from a skilled, unskilled and any provider. About one-fifth of the women (21%) received their 1st ANC within 12 weeks from any provider whereas 14% of them received from a skilled provider. The highest number of women (29%) received their 1st ANC between 13–16 weeks by any provider, whereas half of them (16%) received from a skilled provider.
https://doi.org/10.1371/journal.pone.0241185.g001
“ Table 3 ” shows almost two-thirds of the women (63%) made the timely visit 2 between 24–26 weeks from any provider followed by more than one-third of the women (35%) received the visit 4 between 36–38 weeks. Overall, only 1.2% women received all the 4 timely visits and 18% women did not receive any timely ANC visit. There was a significant difference in receiving all the timely ANC visits by any provider depending on the residence.
https://doi.org/10.1371/journal.pone.0241185.t003
Fig 2 shows that, only 13% women received visit 1 (between 8–12 weeks) timely, but a higher proportion of women (37%) received visit 2 (between 24–26 weeks) at the recommended time. The figure also presents that only 8% of women received the first 2 timely visits (visit 1 & 2) while less than one percent women (0.6%) received all 4 ANC visits (visit 1, 2, 3 & 4) as per recommended timing of the WHO FANC model.
https://doi.org/10.1371/journal.pone.0241185.g002
“ Table 4 ” describes that the majority women (74%) received ANC visit 2 between 24–28 weeks from any provider and 46% from a skilled provider. Half of the women received ANC visit 1 within 16 weeks from any provider while almost one-third of the women (32%) received from a skilled provider. More than one-third of the women (37%) received the first 2 timely visits (visit 1 & 2) by any provider whereas one-fifth of the women (20%) received by a skilled provider. Only 2% women received all the 4 timely visits (visit 1, 2, 3 & 4) from any provider while 1% women received from a skilled provider. In terms of all the timely ANC visits, more urban women received timely ANC visits than those of rural women. There were significant differences in receiving timely ANC visits by any provider except visit 4 and for all the timely ANC visits by a skilled provider based on place of residence.
https://doi.org/10.1371/journal.pone.0241185.t004
“ Table 5 ” presents that less than half of the women (43%) received contact 4 at 30 th week from any provider and near to one-third (27%) from a skilled provider. More than one-third of the women (39%) received contact 3 at 26 th week and contact 5 at 34 th week by any provider whereas one-fourth women received those contacts from a skilled provider. In line with the 2016 WHO ANC model, less than one-fifth of the women (16%) did not have any timely ANC contact from any provider and almost two-thirds of the women (63%) received at least one timing contact from a skilled provider. Only a few women (0.15%) received the timely first five contacts as per the 2016 ANC model from MTP. None of the women received all the 8 timely ANC contact either by a MTP or by any provider. Urban women were more likely to receive timely ANC contacts than those of rural women. There were significant differences in receiving timely contacts by any provider except contact 2 and 6; and by a skilled provider except contact 2 based on place of residence.
https://doi.org/10.1371/journal.pone.0241185.t005
“ Table 6 ” shows that the first two timely ANC visits are estimated derived from the WHO FANC model. Results suggest that there is a strong association between the first two timely ANC visits and all the socio-demographic characteristics except religion.
https://doi.org/10.1371/journal.pone.0241185.t006
“ Table 7 ” shows that almost all the indicators were crudely associated with a higher prevalence of receiving the first two timely visits. After adjustment, the odds ratio of the first two timely ANC visits for the women and their husbands who had completed 10 or more years of schooling were higher than those who did not pass primary school (0–4 years of schooling). Similarly, the likelihood of receiving the first two timely visits for employed women was more than two times than the women who were homemakers. Women who had exposure to mass media (newspaper/magazine) were more likely to receive the first two timely ANC than who were not exposed. Urban women were more than three times more likely to receive the first two timely ANC from a skilled provider than those of rural women.
https://doi.org/10.1371/journal.pone.0241185.t007
This study shows that almost all the women from both rural and urban sites received at least one ANC and more than three-fourth of the women received 4 or more ANC visits by any provider in their last pregnancy. Less than one-fifth of the women received 8 or more contacts by any provider whereas only 4% women received at least 8 contacts by MTPs. However, this uptake rate significantly differs between urban and rural women.
According to the WHO FANC and the 2016 ANC model, the practice of receiving the 1 st ANC visit within recommended time is mostly delayed. There is very little difference in terms of receiving the timely 1 st ANC visit by both MTPs and any provider between the two WHO models. There is slight difference (13% Vs 14% by MTP and 20% Vs 21% by any provider) between the two models on the 1st ANC uptake and that is due to different recommended timings. The FANC model recommends first ANC between 8–12 weeks while the 2016 ANC model suggests to have the first ANC contact within 12 weeks. Therefore, when ANCs are received before 8 weeks, have been considered in the 2016 ANC model and was excluded in the FANC model. However, as per country guideline, the number of the 1st ANC uptake within 16 weeks of gestation by both MTPs and any provider was two times higher than the both WHO models. As Bangladeshi country guideline recommends an elaborated time range for the initiation of ANC, it kindles curiosity among all on the difference. Similar to our findings, three more studies were done in Bangladesh suggest that the uptake of first ANC is substantially delayed and another study revealed that the reasons could be maternal age, women’s education, residence, wealth index, pregnancy intention status, child’s birth order, and wanting more children [ 24 , 33 , 48 , 49 ]. Though no justification has found from the national guideline but our experience from working with the program in the field, we understand that culturally our women delay to disclose about their pregnancies even to their family members and relatives. They delay to seek 1 st ANC for few weeks thinking that pregnancy may terminate (abortion may occur) at an earlier stage, so they wait until 3 to 4 months of the pregnancy to report or visit healthcare centre. May be considering the cultural context, the national guideline adopted 1 st ANC by 16 weeks. Although there is no evidence, however, we are assuming that socio-cultural factors associated with delayed ANC care seeking might have been reflected on our national guideline and thus on the recommendations of the time ranges.
Though there are differences in timing, according to the WHO FANC model and the country guideline the highest proportion of the women received the timely ANC visit 2 by MTPs. Whereas according to the 2016 WHO ANC model, the highest proportion of the women complied with the contact 4 by MTPs. The country guideline mostly matches with the WHO FANC model but the 2016 WHO ANC model focused on the ANC contacts on exact weeks rather than considering ranges of weeks except ‘contact 1’ thus influences the variation of ANC uptake.
As per the WHO FANC model and the country guideline, coverage of all four timely ANC visits were extremely low and no woman could follow all the 8 timely contacts recommended by the 2016 WHO ANC model regardless of the providers. However, completing the 8 contacts is not applicable if women delivered babies before 38 weeks.
Because of the low observations for the all timely visits in both of the WHO models, the regression analysis of this study was limited to only the first two timely visits by a skilled provider as per the WHO FANC model. The regression analysis shows that women and their husbands with more years of schooling, employment, and living in the urban area were more likely to have the 1st two timely visits by MTPs.
Regarding the socio-demographic characteristics like marriage, family planning, and childbearing, Northern Bangladesh shows some variations with other Northeast and Southeast regions of Bangladesh. Early marriage (marriage before 18 years) among Northern Bangladeshi women (Rajshahi: 70% and Rangpur: 67%) is relatively higher than other parts of Bangladesh; therefore the prevalence of teenage childbearing status is also higher (Rajshahi: 33 and Rangpur: 32 vsSylhet: 14 and Chattogram: 27). However, Total Fertility Rate is lower in Northern part (Rajshahi and Rangpur: 2.1) than Northeast (Sylhet: 2.6) and Southeast (Chattogram: 2.5) regions. Regarding the modern contraceptive usage and unmet need for family planning, Rajshahi (modern method: 55%, unmet need: 10%) and Rangpur (modern method: 59%, unmet need: 8%) stand in better position than Sylhet (modern method: 45%, unmet need: 14%) and Chattogram (modern method: 45%, unmet need: 18%) divisions [ 24 ].
The BDHS 2017–18 data shows that the four or more ANC coverage raised to 47% from 31% in 2014. From the BDHS data for the Northern region, we found almost similar results with our study in terms of any ANC coverage by a MTP (BDHS: Rajshahi-84.5% and Rangpur-74.6% Vs this study-82%). The BDHS does not provide regional variation for number of ANCs, so, we couldn’t compare ANC coverage by numbers with BDHS. In addition to that, BDHS also does not present ANC coverage for 8 contacts [ 24 ]. Our study shows more ANC coverage for at least 8 ANC contacts by any provider compared to Bangladesh Multiple Indicator Cluster Survey (MICS) conducted in 2019 (17% Vs 5%) [ 50 ]. However, this difference might have induced due to having different sample size, study sites (local vs national), higher engagement of non-government organizations in providing maternal health services; especially in ANC services in our study areas, low human resource gap, access to health care, etc. [ 51 – 53 ].
In terms of four or more ANC coverage by any provider, a noticeable regional variation was observed for several South-Asian countries [ 24 , 54 – 60 ]. A national survey from Afghanistan shows that in 2015 their national ANC uptake rate for four or more ANC by any provider was 18%, likewise for Bhutan- 85% in 2015, India- 51% in 2016, Myanmar- 59% in 2016, Nepal-69% in 2016 and Pakistan-51% in 2017–2018 [ 55 , 58 , 59 ]. Despite sharing geo-economics commonalities, these South-Asian countries exhibit a good range of variation [ 61 ].
Regarding the 1 st ANC uptake by gestational age, this study found that only one-fifth of the women availed their 1 st ANC in the 1 st trimester (within 12 weeks) and more than one-fourth of the women received their 1 st ANC during 13–16 gestational weeks by any provider. Another Bangladeshi study conducted in Netrokona district found ANC uptake by a formal provider (Doctor, midwives, nurse, FWV, CHCP, health assistant, family welfare assistant, community skilled birth attendant and NGO health workers) in the 1 st trimester is 18% [ 32 ]. Although the operational definition of formal provider of that study slightly differ from our definition of any provider and MTP. If we compare it with our study findings, it shows 21% of the women received the 1 st ANC by any provider and 14% received by MTPs [ 32 ]. We assume the difference between the definition of the skilled and unskilled care provider might have influenced the difference. Many studies conducted in different parts of Asia show, there is a huge national and regional difference in terms of the 1 st ANC uptake [ 54 , 56 – 60 ]. Regarding the 1 st ANC uptake in the 1 st trimester, findings from several studies conducted in India showed the regional variation [ 56 , 57 , 60 ]. Indian national data showed, in 2016 more than half of the women received the 1 st ANC in the 1 st trimester, whereas in Andhra Pradesh more than three-fourth of the women and in eight other EAG states (Empowered Action Group) less than one-fifth of the women took the 1 st ANC uptake in the first trimester [ 56 , 57 , 60 ]. However, EAG states are defined as underprivileged and economically backward compared to other states of India and coverage from EAG states quite similar to our study findings [ 62 ].
Though we found Afghanistan’s four or more ANC uptake is lower than our study, but surprisingly; Afghanistan’s 1st ANC uptake in the 1st trimester was a bit higher than that of ours while Pakistan and Nepal showed more than double ANC uptake rate than our findings [ 54 , 58 , 59 ].
Studies show that the utilization of ANC in developing countries depends on many different factors [ 63 – 66 ]. Different studies done in Asian, European and African continents adopting Andersen behavioral model revealed that factors associated with underutilization of the ANC services in these regions are young age of the mothers, fewer years of schooling, lack of a paid job, poor language proficiency, support from a social network and lack of knowledge of the health care system [ 67 ]. Studies conducted in Bangladesh, different parts of India, Nepal, Afghanistan, Pakistan and Ethiopia explored that years of schooling and place of residence have influence over ANC uptake rate [ 32 , 54 , 56 – 60 , 68 – 70 ]. In comparison to this study; findings from the above cited studies share similarity with our findings on the findings about years of schooling and place of residence. Apart from those, geographical setting and socio-economic inequalities, cultural and normative barriers are attributing to this issue [ 71 ].
Similar to other low and middle-income countries (LMIC), Bangladesh is also improving its ANC coverage. The recommended 4 ANC visits was in a view of cost-effective model and result of extensive research, further, WHO recommended 8 ANC contacts in 2016 to expedite the improvement of Maternal and Child Health related status [ 33 , 72 ]. However, Bangladesh is still focusing on ensuring a higher uptake rate of 4 ANC visits with its government and non-government organizational initiatives [ 33 , 34 , 73 ].
Mounting all findings together from this and previous studies, we found that urban women can avail more ANC services than rural women although the ANC services are free of cost in government facilities everywhere in Bangladesh [ 74 , 75 ]. Based on those shreds of evidence, it can be asserted that ANC service inequality exists based on place of residence agreeing to the fact that 78% of people living in rural Bangladesh, while 70% doctors are stationed in urban areas [ 76 ]. In addition to unavailability of skilled provider, rural Bangladeshi women face various types of challenges to access maternal health services such as: poverty, long distance of health facility, waiting time at hospital, lack of female health staff, lack of skilled birth attendant, lack of education [ 77 – 79 ].
Even after conducting our study in high performing areas in terms of ANC coverage, extremely low prevalence of timely ANC uptake was observed maintaining the WHO and country guidelines. We can assume further worst-case scenario for low performing areas. Although we focused to discuss about ANC uptake by skilled provider in our result mostly but we found that many other national and also global studies we discussed in our paper tend to discuss the ANC uptake by any provider and used slightly different definition of skilled provider than country guideline [ 32 , 54 – 59 , 68 – 70 ]. We are assuming that it is due to low ANC uptake by skilled provider in Bangladesh and other Asian and African countries. So, to understand the countrywide situation, further evidence on timely ANC uptake is required.
Strength and limitation
Study team strictly maintained the quality of data collection in the field with close monitoring and supervision. The data derived from participants were rigorously rechecked and re-interviewed by team supervisors including a physician to minimize the scope of inaccuracy. We also checked relevant documents (such as- ANC card, pregnancy registration card, etc.) during our data collection to minimize the errors. Since this study was conducted only in part with higher ANC coverage, findings of this study hence do not represent Bangladesh uniformly. Again, the analysis was done depending on self-reported information without having a robust surveillance system; therefore, the scope of over or under-reporting may exist. Because of self-reported data, number and timing of ANC visits can be varied. According to all three guidelines, there are variations on the timing of ANC visits by exact week (e.g. 30th week) and range of weeks (e.g. 8–12 weeks); and result from range weeks will vary less but results from exact weeks may vary little bit higher. More to add, we did not explore important potential exposure variables such as household income, awareness about maternity care, cost of service, availability of healthcare services and proximity to the health facility which might have served as confounders and affected the result and the interpretation of the findings.
Conclusions
The coverage of ANC visits is quite high but the timeliness of ANC visits is very low as per both WHO models and country guideline. Initiation for the first ANC visit is also highly delayed. Government and non-government maternal health programs should focus on ensuring timely ANC visits. Ensuring at least 4 timely visits may help to make a way forward for Bangladesh endorsing 8 ANC contacts in the near future that is recommended by the recent 2016 ANC model. We suggest policy makers to promote education, women’s employment and health education through mass media as well as to ensure universal maternal healthcare coverage. Understanding the significance of timely ANC visits we further suggest to carry out more parallel studies both in countrywide and regional perspective putting emphasis on the feasibility of 8 contacts. The findings of this study will help the program and policy makers to design interventions to improve antenatal care coverage maintaining timeliness and thus reduce maternal and child mortality across Bangladesh.
Supporting information
https://doi.org/10.1371/journal.pone.0241185.s001
https://doi.org/10.1371/journal.pone.0241185.s002
Acknowledgments
icddr,b acknowledges with gratitude the commitment of Bill & Melinda Gates Foundation to its research efforts. We are grateful to our study participants for their spontaneous participation and sincere commitment to fulfill the research endeavor. icddr,b is also grateful to the Government of Bangladesh, Canada, Sweden and the UK for providing core/ unrestricted support.
- View Article
- Google Scholar
- PubMed/NCBI
- 4. General Assembly UN. Global indicator framework for the Sustainable Development Goals and targets of the 2030 Agenda for Sustainable Development 2017 [ https://unstats.un.org/sdgs/indicators/Global%20Indicator%20Framework_A.RES.71.313%20Annex.pdf .
- 13. Lucas AO, Stoll BJ, Bale JR. Improving birth outcomes: meeting the challenge in the developing world: National Academies Press; 2003.
- 16. National Institute of Population Research and Training (NIPORT), Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2014. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2016.
- 17. WHO, UNICEF, Mathers C. Global strategy for women’s, children’s and adolescents’ health (2016–2030). Organization. 2016.
- 18. World Health Organization. World health statistics 2016: monitoring health for the SDGs sustainable development goals: World Health Organization; 2016.
- 19. Ministry of Health and Family Welfare (MOHFW). Health, Population, Nutrition eToolkit for Field Workers. 2018.
- 20. Ministry of Health and Family Welfare (MOHFW). Union Health and Family welfare Center operating manual. 2014.
- 22. National Institute of Population Research and Training (NIPORT), Mitra and Associates, ORC Macro. Bangladesh Demographic and Health Survey 2004. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2005.
- 23. National Institute of Population Research and Training (NIPORT), Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2011. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2013.
- 24. National Institute of Population Research and Training (NIPORT), ICF. Bangladesh Demographic and Health Survey 2017–18: Key Indicators. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2019.
- 25. National Institute of Population Research and Training (NIPORT), Mitra and Associates, Macro International. Bangladesh Demographic and Health Survey 2007. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2009.
- 27. World Health Organization, Unicef. Trends in maternal Mortality: 1990–2015: Estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. 2015.
- 28. National Institute of Population ResearchTraining, International Centre for Diarrhoeal Disease Research Bangladesh, MEASURE Evaluation. Bangladesh Maternal Mortality and Health Care Survey 2016: Preliminary Report. 2017.
- 29. National Institute of Population Research Training, MEASURE Evaluation, ICDDR B. Bangladesh maternal mortality and health care survey 2010. NIPORT, MEASURE Evaluation, and icddr, b Dhaka, Bangladesh; 2012.
- 36. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division, Ministry of Planning. Bangladesh Population and Housing Census 2011, Community report, Dinajpur. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division (SID), Ministry of Planning; 2014.
- 37. Bangladesh Bureau of Statistics, Statistics and Informatics Division, Ministry of Planning. Population and Housing Census, Community report, Nilphamari. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division (SID), Ministry of Planning; 2013.
- 38. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division, Ministry of Planning. District Statistics 2011, Rajshahi. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division (SID), Ministry of Planning; 2013.
- 39. Bangladesh Bureau of Statistics, Statistics and Informatics Division, Ministry of Planning. Population and Housing Census 2011. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division (SID) and Ministry of Planning; 2015.
- 41. Myatt M. A short guide to undertaking surveys using the Simple Spatial Survey Method (S3M)2012.
- 42. Dot net framework [ https://dotnet.microsoft.com/download/dotnet-framework .
- 43. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience: World Health Organization; 2016.
- 47. StataCorp. Stata Statistical Software: Release 13. College Station, TX. StataCorp LP; 2013.
- 50. Bangladesh Bureau of Statistics (BBS). Bangladesh Multiple Indicator Cluster Survey 2019, Key Findings. Bangladesh Bureau of Statistics (BBS); 2019.
- 51. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division, Ministry of Planning. Bangladesh Population and Housing Census 2011. Bangladesh Bureau of Statistics (BBS), Statistics and Informatics Division, Ministry of Planning; 2015.
- 52. Human Resource management (HRM), Ministry of Health and Family Welfare (MOHFW). HRH Data Sheet 2014. Human Resource management (HRM), Ministry of Health and Family Welfare (MOHFW), Bangladesh Secretariat, Dhaka; 2014.
- 53. World Mission Prayer League (LAMB Hospital). LAMB Annual Report 2017. [ https://static1.squarespace.com/static/5c72ccf37a1fbd5b042f922c/t/5ca4bebe4e17b61118e6b70f/1554300705648/LAMB+Annual+Report+2017.pdf .
- 54. Central Statistics Organization (CSO), Ministry of Public Health (MoPH), ICF. Afghanistan Demographic and Health Survey 2015. Central Statistics Organization (CSO), Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF; 2017.
- 55. United Nations International Children’s Emergency Fund (unicef). Antenatal care 2016 [ https://data.unicef.org/topic/maternal-health/antenatal-care/ .
- 57. International Institute for Population Sciences (IIPS), ICF. India National Family Health Survey NFHS‐4 2015–16. Mumbai: IIPS; 2017.
- 58. Ministry of Health, Nepal, New ERA, ICF. Nepal Demographic and Health Survey 2016. Ministry of Health, Kathmandu, Nepal; 2017.
- 59. National Institute of Population Studies (NIPS) [Pakistan], ICF. Pakistan Demographic and Health Survey 2017–18. Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF; 2019.
- 61. THE WORLD BANK. Low & middle income 2019 [ https://data.worldbank.org/income-level/low-and-middle-income .
- 68. Chaka EE. Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences-International Campus (TUMS-IC), Tehran, Iran. Studies.13(15):20–2.
- 73. National Institute of Population Research Training, Associates for Community Population Research, ICF International. Bangladesh Health Facility Survey 2014. NIPORT, ACPR, and ICF International Dhaka; 2016.
- 75. World Health Organization. Bangladesh health system review: Manila: WHO Regional Office for the Western Pacific; 2015.
- 76. UNDP Bangladesh. Covid-19: A reality check for Bangladesh’s healthcare system 2020 [10/08/2020]. https://www.bd.undp.org/content/bangladesh/en/home/stories/a-reality-check-for-bangladesh-s-healthcare-system.html .
- 77. Keya K, Rahman MM, Rob U, Bellows B. Barrier of distance and transportation cost to access maternity services in rural Bangladesh. Population Association of Ameria US. 2013.

National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people
- Acknowledgements
Introduction
- Overweight and obesity
- Physical activity
- Chapter 2: Antenatal care
- Immunisation
- Growth failure
- Childhood kidney disease
- Fetal alcohol spectrum disorder
- Preventing child maltreatment – Supporting families to optimise child safety and wellbeing
- Social emotional wellbeing
- Unplanned pregnancy
- Illicit drug use
- Osteoporosis
- Visual acuity
- Trachoma and trichiasis
- Chapter 7: Hearing loss
- Chapter 8: Oral and dental health
- Pneumococcal disease prevention
- Influenza prevention
- Chronic obstructive pulmonary disease
- Bronchiectasis and chronic suppurative lung disease
- Chapter 10: Acute rheumatic fever and rheumatic heart disease
- Chapter 11: Cardiovascular disease prevention
- Chapter 12: Type 2 diabetes prevention and early detection
- Chapter 13: Chronic kidney disease prevention and management
- Chapter 14: Sexual health and blood-borne viruses
- Prevention and early detection of cervical cancer
- Prevention and early detection of primary liver (hepatocellular) cancer
- Prevention and early detection of breast cancer
- Prevention and early detection of colorectal (bowel) cancer
- Early detection of prostate cancer
- Prevention of lung cancer
- Chapter 16: Family abuse and violence
- Prevention of depression
- Prevention of suicide
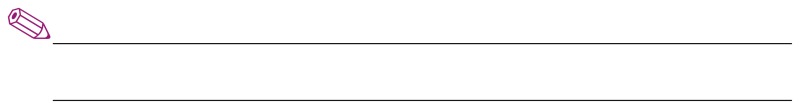
Antenatal care aims to improve health and prevent disease for both the pregnant woman and her baby. While many Aboriginal and Torres Strait Islander women have healthy babies, poor maternal health and social disadvantage contribute to higher risks of having problems during pregnancy and an adverse pregnancy outcome. 1,2 The reasons for these adverse outcomes are complex and multifactorial (Figure 1), and together with other measures of health disparity provide an imperative for all involved in caring for Aboriginal and Torres Strait Islander women to ensure they receive the highest quality antenatal care, and, in particular, care that is woman-centred, evidence-based and culturally competent. This chapter reflects recommendations for Aboriginal and Torres Strait Islander women from two modules of Australian evidence-based antenatal care guidelines 3,4 and incorporates new evidence published subsequently. For selected antenatal care topics, narrative summaries of evidence relevant to Aboriginal and Torres Strait women are presented below. These are:
- screening for genitourinary and blood-borne viral infections
- nutrition and nutritional supplementation
Antenatal care – General features
Antenatal care includes providing support, information and advice to women during pregnancy, undertaking regular clinical assessments, and screening for a range of infections and other conditions as well as following up and managing screen-detected problems. 4 The key feature of high-quality antenatal care for all women is that it is woman-centred, 4 meaning care that includes:
- focusing on each woman’s individual needs, expectations and aspirations, including her physical, psychological, emotional, spiritual, social and cultural needs
- being culturally safe
- supporting women to make informed choices and decisions involving the woman’s partner, family and community, as identified by the woman herself.
High-quality antenatal care for Aboriginal and Torres Strait Islander women includes holistic care that is consistent with the Aboriginal definition of health, being the physical, social, emotional and cultural wellbeing of both an individual and their community. 6
Aboriginal and Torres Strait Islander women are cared for by a range of health professionals during pregnancy, and the cultural competence of healthcare providers is of critical importance to women’s engagement with antenatal care and the delivery of high-quality care. Healthcare providers need an awareness of the higher levels of social and economic disadvantage experienced by many Aboriginal and Torres Strait Islander people and to prioritise doing what they can to address these social determinants of health at both individual and system levels. 7 Building trust, and respectful communication and developing effective therapeutic relationships are also key features of providing high-quality antenatal care to Aboriginal and Torres Strait Islander women. 8 In Australia, antenatal care is delivered in a range of organisational settings including hospitals, general and specialist private practices, government clinics, and Aboriginal Community Controlled Health Services. The involvement of Aboriginal and Torres Strait Islander people in the delivery of care, and in the design and management of services, will improve the quality of care for Aboriginal and Torres Islander women in all settings. 4 The ‘first visit’ is an important focus in antenatal care, as provision of advice and a range of assessment and screening activities is best undertaken early in pregnancy to maximise the benefits. It is recommended that the first antenatal care visit occurs before 10 weeks’ gestation. 4 While there is some evidence of recent improvements, Aboriginal and Torres Strait Islander women are still less likely than other Australian women to receive antenatal care early in pregnancy. 1,9 According to age-standardised national data from 2014, 53% of Aboriginal and Torres Strait Islander women attended antenatal care in the first trimester, compared to 60% of non-Indigenous women, and among Aboriginal and Torres Strait Islander women first trimester attendance was higher for women in outer regional areas (62%) compared to women living in major cities (48%) or very remote areas (51%). 1 This suggests the need for ongoing attention by the healthcare system to promoting and facilitating early engagement of pregnant Aboriginal and Torres Strait Islander women, including strengthening cultural safety and addressing local barriers identified by Aboriginal and Torres Strait Islander women. Current recommendations for antenatal care have shifted from a ‘traditional’ fixed schedule of visits towards a more flexible tailored plan of visits that is developed in consultation with each woman in early pregnancy and designed to meet her individual needs. 4 Ten antenatal care visits are recommended for a woman without complications having her first pregnancy, and seven visits for a woman having a subsequent pregnancy. 4 Antenatal care frequently involves screening that aims to improve outcomes for the pregnant woman and her baby. For all screening conducted during pregnancy, women must be provided with information and an opportunity to ask questions about the tests and potential treatments beforehand, so that they are able to provide informed consent. Screening test results need to be communicated to women whether they are positive or negative, and appropriate management and follow-up of positive results is critical if the potential benefits of screening are to be realised.
Smoking tobacco during pregnancy has a range of negative impacts on the health of women and babies. Adverse birth outcomes are more common among women who smoke during pregnancy and include an increased risk of preterm birth, low birthweight, and stillbirth. Children of women who smoked during pregnancy have higher rates of Sudden Infant Death Syndrome (SIDS), asthma, ear infections and respiratory infections. Quitting smoking before or during pregnancy can reduce these risks. At a national level, an estimated 44% of Aboriginal and Torres Strait Islander women smoked during pregnancy in 2014. 1 The prevalence of smoking during pregnancy for Aboriginal and Torres Strait Islander women is decreasing (down from 52% in 2003 10 ); however, it remains much higher than that of non-Indigenous women who are pregnant (12% in 2014). Smoking during pregnancy is more common among young women, those living in rural and remote areas, and those who experience socioeconomic disadvantage. 1 Factors associated with high smoking rates and low quit rates among Aboriginal and Torres Strait Islander populations include the normalisation of smoking within Aboriginal communities; the presence of social health determinants such as unemployment, poverty, removal from family, and incarceration; personal stressors such as violence, grief and loss; concurrent use of alcohol and cannabis; and lack of access to culturally appropriate support for quitting. 11–14 Aboriginal and Torres Strait Islander women have expressed the view that smoking during pregnancy can help them cope with stress and relieve boredom, and that quitting may be of lower priority compared to the many other personal and community problems they face. 15 Pregnancy is a particularly opportune time for an intensive focus on the delivery of smoking cessation advice and support to women, because of the potential for improving the health of both mother and baby, and because women are more likely to quit smoking during pregnancy. Aboriginal and Torres Strait Islander women have indicated their support for receiving information, advice and support for quitting from caregivers during pregnancy. 16,17 Health professionals, therefore, have an important role to play in providing information and support to women during pregnancy. There is systematic review evidence that psychosocial interventions for smoking cessation during pregnancy are effective at increasing quit rates and improving birth outcomes such as low birthweight. 18 Only one randomised controlled trial has assessed the effectiveness of a tailored smoking cessation intervention for Aboriginal and Torres Strait Islander women. 19 It did not find a significant difference in quit rates between the intervention group and those receiving usual care, suggesting that more work is needed to optimise smoking cessation strategies in pregnancy for Aboriginal and Torres Strait Islander women. All pregnant women should be asked about their smoking history and practices, and it is recommended that those who currently smoke or have recently quit be provided with information about the effects of smoking during pregnancy, advised to quit smoking and stay quit, and offered ongoing and tailored support to do so. 4 Efforts by health professionals to address smoking during pregnancy for Aboriginal women are more likely to be effective when relationships are non-judgemental, trusting and respectful, as well as empowering and supportive of women’s self-efficacy and agency. 12,20 The social context of Aboriginal and Torres Strait Islander women’s lives is very important to consider when designing and delivering smoking cessation advice and support during pregnancy; it has been suggested that addressing stressors, and building skills and coping strategies, are likely to increase the efficacy of smoking cessation efforts. 14,15 Involvement of partners and families, as well as community-wide efforts to denormalise and reduce smoking in Aboriginal communities, are also recommended as strategies to address smoking in pregnancy for Aboriginal and Torres Strait Islander women. While evidence for the effectiveness of nicotine replacement therapies (NRT) during pregnancy is currently limited, trial results suggest NRT can have positive impacts on quit rates and child development outcomes, and there is no evidence of associated harms. 21 The use of NRT during pregnancy is recommended when initial quit attempts have not been successful, with preference being for the use of an intermittent mode of delivery (such as lozenges, gum or spray) rather than continuous (such as patches). 4 The safety of oral pharmacotherapies (such as buprenorphine and varenicline) and e-cigarettes, and their effectiveness as measures to support quitting during pregnancy, is not known and therefore they are not recommended for use. 21
Screening for genitourinary and blood-borne infections
Urinary tract infections.
Asymptomatic bacteriuria is common during pregnancy, and may be more common among Aboriginal and Torres Strait Islander women. 22–24 Ascending urinary tract infection during pregnancy may lead to pyelonephritis, and an association with preterm birth and low birth weight has been suggested. 4 A Cochrane review has demonstrated that treatment with antibiotics is effective at clearing asymptomatic bacteriuria during pregnancy, and results in a reduced risk of pyelonephritis as well as providing suggestive evidence about a reduced risk of adverse pregnancy outcomes such as preterm birth and low birthweight. 25 All women should be routinely offered testing for asymptomatic bacteriuria early in pregnancy using a midstream urine culture. 4 Urine dipstick for nitrites is not a suitable test for diagnosing infection, as false positives are frequent; however, a negative dipstick result means infection is unlikely. Appropriate storage of dipsticks is essential, as high humidity and temperature can impact on their accuracy.
Chlamydia is a common sexually transmitted infection (STI) that can be asymptomatic and can lead to pelvic inflammatory disease, infertility and ectopic pregnancy. Chlamydia infection during pregnancy has been associated with higher rates of preterm birth and growth restriction, and can result in neonatal conjunctivitis and respiratory tract infections. 4 Antibiotics are effective at treating chlamydia, and there is some evidence that treatment during pregnancy reduces the incidence of preterm birth and low birth weight. 26,27 Chlamydia prevalence estimates for pregnant Aboriginal and Torres Strait Islander women vary from 2.9% to 14.4%. 30,31 Chlamydia is most common among young people, with 80% of diagnoses among Aboriginal and Torres Strait Islander people being in this group. 30 Notification rates for chlamydia are eight times higher for Aboriginal and Torres Strait Islander people living in remote regions. 30 Australian national evidence-based antenatal care guidelines recommend that chlamydia testing is routinely offered during pregnancy at the first antenatal care visit to pregnant women aged less than 25 years, and to all women who live in areas where chlamydia and other STIs have a high prevalence. 4 Pregnant women who test positive to chlamydia, and their partners, need follow-up, assessment for other STIs and treatment.
Gonorrhoea is a sexually acquired infection that can cause pelvic inflammatory disease and chronic pelvic pain in women. Gonorrhoea infection during pregnancy is associated with adverse outcomes including ectopic pregnancy, miscarriage, preterm birth and maternal sepsis during and after pregnancy. 4 Transmission at the time of birth can lead to neonatal conjunctivitis, which may cause blindness. Gonorrhoea is most commonly diagnosed in young people, and is more common for Aboriginal and Torres Strait Islander people living in outer regional and remote areas. 30 Rates of diagnosis have been declining but remain high in these regions. 30 Australian national evidence-based antenatal care guidelines recommend against screening all pregnant women for gonorrhoea, because there is a relatively low prevalence of disease and there is potential for harms associated with false positive test results, particularly in low-risk populations. 4 Screening for gonorrhoea is recommended for pregnant women who live in, or come from, areas of high prevalence (outer regional and remote areas), or who have risk factors for STIs. Pregnant women who test positive to gonorrhoea, and their partners, need follow-up, assessment for other STIs and treatment.
Trichomoniasis
Trichomoniasis is a sexually transmitted vaginitis that is commonly asymptomatic, but can cause a yellow–green vaginal discharge and vulval irritation, and may be associated with infertility and pelvic inflammatory disease. 3 The implications of trichomoniasis during pregnancy remain unclear; while an association between trichomoniasis and preterm birth and low birth weight has been demonstrated, evidence of a cause and effect relationship is currently lacking. 31 The benefits of screening asymptomatic women for trichomonas during pregnancy are uncertain, because there is no evidence that antibiotic treatment improves pregnancy outcomes, 3,31 with one trial suggesting a higher rate of preterm birth among pregnant women who were treated for asymptomatic trichomoniasis with metronidazole. 31 For this reason screening of asymptomatic, pregnant women is not recommended. 3
Bacterial vaginosis
Bacterial vaginosis (BV) is a deficiency of normal vaginal flora (Lactobacilli) and a relative overgrowth of anaerobic bacteria. BV occurs commonly and is often asymptomatic, although it can also cause a greyish vaginal discharge. 4 In epidemiological studies, BV has been associated with a higher rate of preterm birth. While antibiotics for BV have been found to be effective at eradicating BV microbiologically, they have not resulted in a reduction in the preterm birth rate. 32 For this reason, routine screening of asymptomatic pregnant women for BV is not recommended. 4,32 Symptomatic women diagnosed with BV, however, should be treated.
Group B streptococcus
Group B streptococcus (GBS) is a bacteria that commonly colonises the gastrointestinal tract, vagina and urethra, and has the potential to increase the risk of preterm birth and cause serious neonatal infection after birth. 4 For women who are colonised with GBS, intravenous antibiotics during labour can prevent more than 80% of neonatal infection. 4 Australian estimates suggest a prevalence of GBS colonisation among all pregnant women of around 20%. 4 Prevention strategies can involve two main approaches: antenatal screening for GBS in late pregnancy (at 35–37 weeks’ gestation), or an assessment of risk factors for GBS transmission during labour (including preterm birth, maternal fever and prolonged rupture of membranes). As there is currently no clear evidence supporting one strategy over the other, Australian national evidence-based antenatal care guidelines recommend either strategy can be used. 4
Syphilis is an STI with serious systemic sequelae. During pregnancy, syphilis can cause spontaneous miscarriage or stillbirth, or lead to congenital infection that is commonly fatal or results in severe and permanent impairment. Congenital syphilis can be prevented by effective treatment of maternal syphilis with antibiotics. 33 In Australia, notifications of infectious syphilis have been declining but have remained more common for Aboriginal and Torres Strait Islander peoples compared to non-Indigenous populations. 30 However, since 2010 there has been a marked increase in notifications of infectious syphilis, driven by an outbreak in northern Australia, including Western Australia, the Northern Territory and Queensland. 34 This outbreak has included a total of 22 cases of congenital syphilis being notified nationally between 2011 and 2015, with 14 of these cases being Aboriginal and Torres Strait Islander babies, 30 and several infant deaths from syphilis have occurred. 34 All pregnant women should be routinely offered testing to screen for syphilis at the first antenatal visit, and repeat screening later in pregnancy may be appropriate in regions of high prevalence. 4 The interpretation of syphilis serology can be complex. To ensure diagnosis, treatment and follow-up are consistent with evidencebased best practice, it is recommended that expert advice is sought if a pregnant woman tests positive for syphilis on an initial screen. 4
While human immunodeficiency virus (HIV) infection is uncommon in Australia, screening during pregnancy for all women at the first antenatal visit is recommended because of the serious consequences of mother-tochild transmission and the availability of treatments effective at reducing this risk. 4 These treatments include caesarean section, short courses of selected antiretroviral medications, and the avoidance of breastfeeding. HIV infection currently occurs at similar rates for Aboriginal and Torres Strait Islander and non-Indigenous population groups in Australia. 30 Women who test positive for HIV require careful and confidential follow-up, including repeat confirmatory testing, assessment and specialist management.
Hepatitis C
Hepatitis C is a blood-borne virus with the potential for causing serious long-term sequelae, including cirrhosis, hepatocellular carcinoma and liver failure through chronic infection. Hepatitis C infection is diagnosed up to four times more often among Aboriginal and Torres Strait Islander women than nonIndigenous women, and is increasing. 30 Perinatal transmission occurs for 4–6% of babies born to women who are positive to both hepatitis C antibody and hepatitis C RNA during pregnancy, and this risk is higher with increasing viral load. 4 In recent years, the increased availability of effective anti-viral therapies with fewer adverse impacts than previously available treatments has greatly improved treatment options and outcomes for people with chronic hepatitis C infection. 35 However, at the time of writing, anti-viral therapies used for treating for hepatitis C are not approved or recommended for use during pregnancy. 35 The lack of antenatal treatment options and the potential psychological harms associated with false positive results of screening tests are the main reasons that routine screening of all women for hepatitis C during pregnancy is not recommended. 4 Testing during pregnancy may be considered, however, for women with identifiable risk factors, including intravenous drug use, tattooing and body piercing, and incarceration. 4 If an initial hepatitis C antibody test is positive, a confirmatory hepatitis C RNA test is required to assess risks and guide management for the woman and baby, and both should be appropriately followed up.
Hepatitis B
Aboriginal and Torres Strait Islander populations have higher rates of diagnosis of hepatitis B infection than non-Indigenous population groups, and available evidence suggests this pattern is also true of hepatitis B surface antigen positivity during pregnancy. 30,36,37 All pregnant women should be offered screening for hepatitis B infection by testing for hepatitis B surface antigen at their first antenatal care visit, and those that test positive should be appropriately followed up. 4 Newborn children of women with current hepatitis B infection (hepatitis B surface antigen positive) can be vaccinated after delivery. Vaccination and the provision of immunoglobulin to the baby at birth is approximately 95% effective at preventing perinatal transmission. 4
Nutrition and nutritional supplementation
Good nutrition during pregnancy is important for the health of the woman, and the development and growth of the baby. Providing women with information and advice about nutritional needs during pregnancy is an important part of routine antenatal care. In providing this advice to Aboriginal and Torres Strait Islander women, it is important to consider the significance of barriers to accessing nutritious foods (eg fresh fruit, vegetables) because of costs and lack of availability in rural and remote regions (refer to Chapter 1: Lifestyle, ‘Overweight and obesity’ ).
Weight and body mass index
Overweight and obesity is becoming increasingly common in Australia, and is more common in Aboriginal and Torres Strait Islander population groups. 9 In 2014, obesity during pregnancy was documented for 33% of Aboriginal and Torres Strait Islander women compared to 20% of non-Indigenous women. 1 Being overweight (body mass index [BMI] ≥25 kg/m 2 ) or underweight (BMI <18.5 kg/m 2 ) before pregnancy are each associated with an increased risk of adverse birth outcomes. Being overweight before pregnancy or having a high weight gain during pregnancy is associated with higher rates of preterm birth, caesarean section, gestational high blood pressure or pre-eclampsia, gestational diabetes, postpartum haemorrhage, and depression, as well as a baby being more likely to be of low birthweight or large for gestational age. Being underweight before pregnancy or having a low weight gain during pregnancy is associated with an increased risk of preterm birth, low birthweight and being small for gestational age. The national evidence-based antenatal care guidelines recommend routine assessment of a woman’s weight and height, and calculation of BMI at the first antenatal care visit. 4 Weighing women at subsequent visits is recommended only when it is likely to influence clinical management. Recommended weight gain during pregnancy varies with a woman’s estimated pre-pregnancy BMI from a total of 6 kg to 18 kg ( Box 1 ). While weight loss is not an appropriate aim during pregnancy, strong evidence suggests interventions for women who are overweight based on increased physical activity and dietary counselling combined with weight monitoring can reduce inappropriate weight gain during pregnancy, as well as reduce the risks of caesarean section, macrosomia and neonatal respiratory morbidity. 38–40
Aboriginal and Torres Strait Islander populations are at greater risk of anaemia, 41 and iron deficiency is the most common cause of anaemia. Routine iron supplementation for all pregnant women is not recommended, because evidence of improved pregnancy outcomes is lacking and there may be adverse impacts. 4 However, it is recommended that all women be screened for anaemia at the first and subsequent visits during pregnancy, and that iron supplementation be used to treat iron deficiency if it is detected. 4 Management of iron deficiency anaemia during pregnancy includes dietary advice, iron supplementation and follow-up. Pregnant women can potentially benefit by being advised about iron-rich foods and that iron absorption can be aided by vitamin C– rich foods, such as fresh fruit and fruit juice, and reduced by tea and coffee. 4,42
Routine folic acid supplementation before and during pregnancy is recommended for all women as it is effective in reducing the risk of neural tube defects. 4 The incidence of this group of congenital abnormalities decreased in Australia among non-Indigenous women after folic acid supplementation during pregnancy became widespread. 43 However, Aboriginal and Torres Strait Islander women were still experiencing high rates of neural tube defects. 43,44 Following mandatory folic acid fortification of bread, which has occurred since 2009, rates of neural tube defects among Aboriginal and Torres Strait Islander women have dropped significantly and are now lower than those of other Australian women. 45
Increased thyroid activity during pregnancy results in increased maternal requirements for iodine, which is essential for neuropsychological development. While severe iodine deficiency during pregnancy is uncommon in Australia, recent evidence suggests that mild and moderate levels of iodine deficiency during pregnancy may result in negative impacts on the neurological and cognitive development of the child. 47 While mandatory iodine fortification of bread since 2009 has improved iodine levels in the general Australian population, available evidence suggests that for many women dietary intake of iodine will not be sufficient to meet needs during pregnancy and breastfeeding. 45 As a consequence, it is recommended that all pregnant women take an iodine supplement of 150 mcg daily. 4,47
Vitamin D is essential for skeletal development, and vitamin D deficiency may have a range of negative health impacts, including during pregnancy. 4,48 The prevalence of vitamin D deficiency varies geographically and between different population groups, and there have been few estimates of prevalence among Aboriginal and Torres Strait Islander populations. 49,50 Risk factors for vitamin D deficiency include limited exposure to sunlight, dark skin and a high BMI. Vitamin D supplementation for women with vitamin D deficiency increases maternal levels of vitamin D, but there is currently no evidence that it improves pregnancy outcomes. 4,48 Screening pregnant women for vitamin D deficiency is recommended only if they have risk factors, and women who are found to be vitamin D deficient should be treated with supplementation because of the potential benefits to their long-term health. 4,48
Diabetes in pregnancy includes type 1 or type 2 diabetes diagnosed before pregnancy, undiagnosed pre-existing diabetes, and gestational diabetes, where glucose intolerance develops in the second half of pregnancy. All forms of diabetes in pregnancy are associated with increased risks for both the pregnant woman and the baby, with the level of risk depending on the level of hyperglycaemia. 3,51–53 Diabetes in pregnancy is associated with an increased risk of induced labour, preterm birth, caesarean section and pre-eclampsia. Babies of mothers with diabetes in pregnancy have higher rates of stillbirth, fetal macrosomia, low APGAR (Appearance, Pulse, Grimace, Activity, Respiration) scores, neonatal hypoglycaemia, and admission to special care/neonatal intensive care units. Babies born to mothers with pre-existing diabetes also have a higher risk of congenital malformations of the spine, heart and kidneys. In addition, raised maternal glycaemic levels are associated with a child having increased adiposity in childhood and other adverse metabolic factors that may increase the risks of later cardiovascular disease and diabetes. Women with gestational diabetes also have an increased risk of developing type 2 diabetes later in life. The number of women with all types of diabetes in pregnancy is increasing. At a national level in 2014, an estimated 4% of Aboriginal and Torres Strait Islander women had diabetes in pregnancy and 13% had gestational diabetes, and each of these rates was higher than those of non-Indigenous women (3.5 times higher for diabetes and 1.6 times higher for gestational diabetes). 1 Given the high prevalence of diabetes in Aboriginal and Torres Strait Islander populations, a significant number of Aboriginal and Torres Strait Islander women are likely to have undiagnosed diabetes at the time they become pregnant. Consequently, screening all Aboriginal and Torres Strait Islander women for pre-existing diabetes is recommended at the first antenatal care visit. 3,54 Tests recommended for screening for undiagnosed diabetes are fasting plasma glucose, plasma glucose after a 75 g glucose load, or random plasma glucose. 3 The use of HbA1C levels to screen for diabetes during pregnancy has not yet been fully evaluated, but has been proposed as an alternative test to consider for early pregnancy screening if other tests such as an oral glucose tolerance test are not feasible; an HbA1C level above 6.5% suggests pre-existing diabetes. 54 Internationally, screening guidelines for gestational diabetes vary in their recommendations about whether screening should be offered to all pregnant women or only to women with risk factors for diabetes. However, given the higher risk of diabetes experienced by Aboriginal and Torres Strait Islander populations, it is recommended that all pregnant Aboriginal and Torres Strait Islander women without pre-existing diabetes are offered screening for gestational diabetes. The recommended timing for gestational diabetes screening to occur is 24–28 weeks’ gestation, and recommended tests include fasting plasma glucose, or plasma glucose one hour and two hours after a 75 g glucose load. 3,54 While diagnostic criteria for gestational diabetes continue to be debated, Australian national evidence-based antenatal care guidelines 3 and the Australasian Diabetes in Pregnancy Society 54 both recommend the use of criteria endorsed by the World Health Organization (WHO) and International Association of Diabetes and Pregnancy Study Group (refer to ‘Recommendations: Diabetes’). In discussions about screening for diabetes and gestational diabetes, women need information about the risks associated with these conditions and the effectiveness of management in reducing and mitigating these risks. 56,57 In general terms, management strategies for diabetes in pregnancy and gestational diabetes include optimising nutrition, increasing physical activity, monitoring and controlling weight gain, additional monitoring activities including of fetal growth and wellbeing, and the use of medications. Medications include insulin and, increasingly, oral hypoglycaemics for women where adequate glycaemic control is not achieved using non-pharmacological measures. Optimising control of gestational diabetes is important to reduce pregnancy-related risks for the woman and baby, and may also have longer term implications on the health of the infant into adulthood. For women with gestational diabetes, screening for diabetes after delivery is also important as it provides an opportunity for intervention to improve women’s future health. 57

- Australian Institute of Health and Welfare. Australia’s mothers and babies 2014. Perinatal statistics series no. 32. Canberra: AIHW, 2016.
- Humphrey MD, Bonello M, Chughtai A, Macaldowie A, Harris K, Chambers G. Maternal deaths in Australia 2008–12. Canberra: AIHW, 2015.
- Australian Health Ministers’ Advisory Council. Clinical practice guidelines: Antenatal care – Module II. Canberra: Department of Health, 2014.
- Australian Health Ministers’ Advisory Council. Clinical practice guidelines: Antenatal care – Module 1. Canberra: Department of Health and Ageing, 2012.
- Clarke M, Boyle J. Antenatal care for Aboriginal and Torres Strait Islander women. Aus Fam Physician 2014;43(1/2):20–24.
- National Aboriginal Health Strategy Working Party. National Aboriginal Health Strategy. Canberra, 1989.
- Wilson G. What do Aboriginal women think is good antenatal care? Consultation Report. Darwin: Cooperative Research Centre for Aboriginal Health, 2009.
- McHugh AM, Hornbuckle J. Maternal and child health model of care in the Aboriginal community controlled health sector. Perth: Aboriginal Health Council of Western Australia, 2011.
- Australian Health Ministers’ Advisory Council. Aboriginal and Torres Strait Islander health performance framework 2014 report. Canberra: Department of Health, 2015.
- Laws PG, Sullivan EA. Smoking and pregnancy. Sydney: Australian Institute of Health and Welfare National Perinatal Statistics Unit, 2006.
- Thomas DP, Briggs V, Anderson IP, Cunningham J. The social determinants of being an Indigenous non‐smoker. Aust N Z J Public Health 2008;32(2):110–16.
- Bond C, Brough M, Spurling G, Hayman N. ‘It had to be my choice’. Indigenous smoking cessation and negotiations of risk, resistance and resilience. Health Risk Soc 2012;14(6):565–81.
- Passey ME, Sanson-Fisher RW, D’Este CA, Stirling JM. Tobacco, alcohol and cannabis use during pregnancy: Clustering of risks. Drug Alcohol Depend 2014;134:44–50.
- Passey ME, D’Este CA, Stirling JM, Sanson‐Fisher RW. Factors associated with antenatal smoking among Aboriginal and Torres Strait Islander women in two jurisdictions. Drug Alcohol Rev 2012;31(5):608–16.
- Gould GS, Munn J, Watters T, McEwen A, Clough AR. Knowledge and views about maternal tobacco smoking and barriers for cessation in Aboriginal and Torres Strait Islanders: A systematic review and meta-ethnography. Nicotine Tob Res 2013;15(5):863–74.
- Passey ME, Sanson-Fisher RW. Provision of antenatal smoking cessation support: A survey with pregnant Aboriginal and Torres Strait Islander women. Nicotine Tob Res 2015;17(6):746–49.
- Passey ME, Sanson-Fisher RW, Stirling JM. Supporting pregnant Aboriginal and Torres Strait Islander women to quit smoking: Views of antenatal care providers and pregnant Indigenous women. Maternal Child Health J 2014;18(10):2293–99.
- Chamberlain C, O’Mara‐Eves A, Porter J, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev 2017;2:CD001055.
- Eades SJ, Sanson-Fisher RW, Wenitong M, et al. An intensive smoking intervention for pregnant Aboriginal and Torres Strait Islander women: A randomised controlled trial. Med J Aust 2012;197(1):42.
- Gould GS, Bittoun R, Clarke MJ. Guidance for culturally competent approaches to smoking cessation for Aboriginal and Torres Strait Islander pregnant women. Nicotine Tob Res 2016;18(1):104.
- Coleman T, Chamberlain C, Davey MA, Cooper SE, Leonardi‐Bee J. Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2015;(12):CD010078.
- Bookallil M, Chalmers E, Andrew B. Challenges in preventing pyelonephritis in pregnant women in Indigenous communities. Rural Remote Health 2005;5(3):395.
- Panaretto KS, Lee HM, Mitchell MR, et al. Prevalence of STIs in pregnant urban Aboriginal and Torres Strait Islander women in northern Australia. Aust N Z J Obstet Gynaecol 2006;46(3):217–24.
- Hunt J. Pregnancy care and problems for women giving birth at Royal Darwin Hospital. Melbourne: Centre for the Study of Mothers’ and Children’s Health, La Trobe University, 2004.
- Smaill FM, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev 2015;(8):CD000490.
- Ryan GM Jr, Abdella TN, McNeeley SG, Baselski VS, Drummond DE. Chlamydia trachomatis infection in pregnancy and effect of treatment on outcome. Am J Obstet Gynecol 1990;162(1):34–39.
- McMillan JA, Weiner LB, Lamberson HV, et al. Efficacy of maternal screening and therapy in the prevention of chlamydia infection of the newborn. Infection 1985;13(6):263–66.
- Lewis D, Newton DC, Guy RJ, et al. The prevalence of chlamydia trachomatis infection in Australia: A systematic review and metaanalysis. BMC Infect Dis 2012;12(1):113.
- Graham S, Smith LW, Fairley CK, Hocking J. Prevalence of chlamydia, gonorrhoea, syphilis and trichomonas in Aboriginal and Torres Strait Islander Australians: A systematic review and meta-analysis. Sex Health 2016;13(2):99–113.
- The Kirby Institute. Bloodborne viral and sexually transmissible infections in Aboriginal and Torres Strait Islander people: Surveillance and evaluation report 2015. Sydney: The Kirby Institute, 2016.
- Gülmezoglu AM, Azhar M. Interventions for trichomoniasis in pregnancy. Cochrane Database Syst Rev 2011;(5):CD000220.
- Brocklehurst P, Gordon A, Heatley E, Milan SJ. Antibiotics for treating bacterial vaginosis in pregnancy. Cochrane Database Syst Rev 2013;(1):CD000262.
- Walker GJ. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst Rev 2001;(3):CD001143.
- Bright A, Dups J. Infectious and congenital syphilis notifications associated with an ongoing outbreak in northern Australia. Commun Dis Intell Q Rep 2016;40(1):E7–10.
- Thompson A. Australian recommendations for the management of hepatitis C virus infection: A consensus statement. Med J Aust 2016;204(7):268–72.
- Graham S, Guy RJ, Cowie B, et al. Chronic hepatitis B prevalence among Aboriginal and Torres Strait Islander Australians since universal vaccination: A systematic review and meta-analysis. BMC Infect Dis 2013;13(1):403.
- Schultz R. Hepatitis B screening among women birthing in Alice Springs Hospital, and immunisation of infants at risk. Northern Territory Disease Control Bulletin 2007;14(2):1–5.
- Campbell F, Johnson M, Messina J, Guillaume L, Goyder E. Behavioural interventions for weight management in pregnancy: A systematic review of quantitative and qualitative data. BMC Public Health 2011;11(1):491.
- National Health and Medical Research Council. Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. Melbourne: NHMRC, 2013.
- Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev 2015;(6):CD007145.
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander health survey: Biomedical results, 2012–13. Canberra: ABS, 2014.
- National Blood Authority. Patient blood management guidelines: Module 5 – Obstetrics and maternity. Canberra: NBA, 2015.
- Bower C, D’Antoine H, Stanley FJ. Neural tube defects in Australia: Trends in encephaloceles and other neural tube defects before and after promotion of folic acid supplementation and voluntary food fortification. Birth Defects Res A Clin Mol Teratol 2009;85(4):269–73.
- Macaldowie A. Neural tube defects in Australia: Prevalence before mandatory folic acid fortification. Canberra: AIHW, 2011.
- Australian Institute of Health and Welfare. Monitoring the health impacts of mandatory folic acid and iodine fortification. Canberra: AIHW, 2016.
- National Health and Medical Research Council. Iodine supplementation during pregnancy and lactation – A literature review. Canberra: NHMRC, 2009.
- National Health and Medical Research Council. Iodine supplementation: Public statement. Canberra: NHMRC, 2010.
- Paxton GA, Teale GR, Nowson CA, et al. Vitamin D and health in pregnancy, infants, children and adolescents in Australia and New Zealand: A position statement. Med J Aust 2013;198(3):142–43.
- Benson J, Wilson A, Stocks N, Moulding N. Muscle pain as an indicator of vitamin D deficiency in an urban Australian Aboriginal population. Med J Aust 2006;185(2):76–77.
- Vanlint SJ, Morris HA, Newbury JW, Crockett AJ. Vitamin D insufficiency in Aboriginal Australians. Med J Aust 2011;194(3):131–34.
- Lowe LP, Metzger BE, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcome (HAPO) study. Diabetes Care 2012;35(3):574–80.
- Contreras M, Sacks DA, Bowling FG, et al. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. Int J Gynaecol Obstet 2002;78(1):69–77.
- McElduff A, Cheung NW, McIntyre HD, et al. The Australasian Diabetes in Pregnancy Society consensus guidelines for the management of type 1 and type 2 diabetes in relation to pregnancy. Med J Aust 2005;183(7):373–77.
- Nankervis A, McIntyre H, Moses R, et al. ADIPS consensus guidelines for the testing and diagnosis of hyperglycaemia in pregnancy in Australia and New Zealand. Sydney: Australasian Diabetes in Pregnancy Society, 2014.
- Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005;352(24):2477–86.
- Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 2009;361(14):1339–48.
- Chamberlain C, McLean A, Oats J, et al. Low rates of postpartum glucose screening among indigenous and non-indigenous women in Australia with gestational diabetes. Maternal Child Health J 2015;19(3):651–63.
- Cancer Council Australia Cervical Cancer Screening Guidelines Working Party. National Cervical Screening Program: Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding. Sydney: Cancer Council Australia, 2016.
- Woolcock J, Grivell R. Noninvasive prenatal testing. Aust Fam Physician 2014;43(7):432–34.
- beyondblue. Clinical practice guidelines for depression and related disorders – anxiety, bipolar disorder and puerperal psychosis – in the perinatal period: A guideline for primary care health professionals. Melbourne: beyondblue, 2011.
- Australian Technical Advisory Group on Immunisation. The Australian immunisation handbook. 10th edn. Canberra: Department of Health, 2017.
- The Royal Australian and New Zealand College of Obtetricians and Gynaecologists. Measurement of cervical length for prediction of preterm birth. Sydney: RANZCOG; 2017 . [Accessed 10 November 2017].
National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people (PDF 9.8 MB)
Evidence base to a preventive health assessment in Aboriginal and Torres Strait Islander people (PDF 9.4 MB)
National Guide Lifecycle chart (child) (PDF 555 KB)
National Guide Lifecycle chart (young) (PDF 1 MB)
National Guide Lifecycle chart (adult) (PDF 1 MB)

- Vishal's account
- Prenatal Care
Your Antenatal Check Up Schedule

How Many Antenatal Appointments Will You Have?
What happens at prenatal appointments, week-wise antenatal visit schedule.
Congratulations on your pregnancy! Now that you are expecting, you must be looking forward to a hassle-free pregnancy and childbirth. But to ensure that everything goes well, you need to find the right doctor and midwife for you because their advice will make your pregnancy journey so much better! As soon as you come to know that you’re pregnant, you should see an OB-GYN and schedule the appointments. Health check-ups or appointments during pregnancy are called antenatal check-ups and since you’ll be seeing your doctor a lot now, you will obviously want to know what happens at these antenatal check-ups! Read this article to find out!
If it’s your first pregnancy and you have a healthy pregnancy , with no medical issues or complications, then you may be required to visit your doctor 8 to 10 times on an average. However, if this is not your first pregnancy and you are not facing any medical issues, then you may have approximately 7 to 9 antenatal visits. The number of visits may vary according to any health conditions or complications that you may be facing during your pregnancy. In case, you have a high-risk pregnancy, then your doctor may keep a close check on your pregnancy, and you may be required to go for frequent antenatal visits.
Your doctor or midwife may offer you the antenatal care according to the stage of pregnancy you are in, any health risks that you or your baby may be facing or any other complication, if any, you may have during your pregnancy. You may have to undergo various tests, scans and check-ups, which include the following:
- Your obstetrician may ask you about your medical history, which may include your previous pregnancies, miscarriages if any, or any other medical condition you may have.
- You could be asked about any medications that you may be taking.
- Your mental health may be checked to see if you are not suffering from any form of anxiety , depression etc.
- Your doctor may tell you about your estimated date of delivery.
- Your doctor may ask you to undergo some urine and blood tests .
- Your weight and blood pressure will be monitored too.
- You may be suggested some dietary and lifestyle changes.
- Your doctor may like to discuss your birth plan with you.
- Your doctor may conduct ultrasound scans to monitor your baby’s growth and development.
- You may be asked about any physical or emotional symptoms that you are concerned about.
- You may be asked to discuss any pregnancy-related concerns or queries that you may have.
We shall now discuss week-wise prenatal appointment schedule or prenatal care schedule that you may have to keep up with.
1. Week 8 to 12
This may be your first antenatal visit, and this should ideally happen before 10 weeks of pregnancy . In this visit you may be asked the following details:
- Your lifestyle and diet
- Your medical history
- Any health issues that you may be facing
- Your birth plan
- Whether or not you are a working woman
- Whether you plan to breastfeed or not
Here’s some information that your doctor or midwife may share with you:
- When you will be going for the ultrasound scans
- What supplements you may be required to take
- What tests and scans you may have to undergo, and your doctor will share the information of their pros and cons
- You will be handed over a copy of your report after your visit
2. Week 10 to 14
During this visit, your doctor could conduct your first ultrasound scan. During this visit, you may come to know your expected date of delivery or EDD and also know how well your baby is growing inside you. You may also come to know if you are carrying one or more babies. Also, your doctor can try and find out if your baby may be suffering from any kind of genetic abnormalities such as Down’s syndrome and other such complications.
Your blood and urine tests results will be discussed by your doctor. In case iron deficiency is diagnosed, you may be prescribed iron supplements to tackle it. Also, your urine may be tested for the presence of protein. Your weight and blood pressure will be measured too. You may also be told about your anomaly ultrasound scan that may be conducted in your next visit. At this stage, if you face any sort of discomfort or concerns, ensure that you communicate with your doctor so she can advise you on the steps to take.
4. Week 18 to 21
It is during this visit that your doctor may want to conduct the anomaly scan. This scan is performed to see how your baby is developing inside your womb and to also to check whether or not there may be any kind of physical abnormalities present in the foetus. In countries where it is legal, parents may also be told about the sex of their baby. Also, if you may not have had your screening for Hepatitis B , Syphilis or HIV , it may be conducted now.
You will probably have to go for this visit in case you are a first-time mommy-to-be. Your blood pressure may be checked, and your urine may again be examined for the presence of protein as a precaution. Your doctor may measure the size of the baby bump by doing so from the top of your bump to the pelvic bone—this is done to see how your baby is developing.

Your obstetrician may conduct a blood test to check your iron levels and also to check your antibodies. If your levels aren’t within the favourable range, your doctor may suggest an appropriate dosage of supplements. From here on your doctor will also measure your baby bump every time to see how well your baby may be developing. Routine blood and urine work may follow. In case you have been found out to be rhesus negative blood type, and there may be a likelihood that your baby may be rhesus positive, your doctor may give you an anti-D injection to kill any antibodies that your body may develop.
During this visit, you can expect our urine may be checked for protein once again, and your blood pressure may be checked too. Your doctor could also discuss the test results of any previous visits. Your midwife may measure the size of your uterus to monitor the growth of your baby.
This is the time when you may be told about labour pains , how to differentiate between active and false labour , how to cope up with the labour and also how do you plan for your labour. Your doctor may also discuss normal and caesarean delivery . If there are any changes that you may have to undergo a C-section, your doctor will discuss the same with you. However, it may be too soon to decide at this stage about the kind of delivery that you may have. If you are rhesus negative, then you may be given your second shot of anti-D injection during this time.
You are close to your delivery, and thus your doctor or midwife may like to share the following information with you:
- How to breastfeed your baby
- Any screening tests that may be required for your newborn baby
- How you may take care of your health after delivery
- You may also be told about postpartum depression or baby blues
Apart from discussing the above issues, your doctor or midwife will check the position of your baby. Your baby bump may be measured too. Your urine and blood pressure will again be checked again. Your baby bump or uterus may be measured as well.
Your uterus may be measured to check the progress of your baby along with testing your urine for protein and checking your blood pressure too. At this stage, your doctor may like to discuss your options, in case your pregnancy goes beyond 41 weeks of pregnancy . You may feel all jittery and worried as you near your delivery, however, you should feel free to discuss any of your doubts and worries with your midwife or your doctor.
11. Week 40
This visit will be required in case it is your first-time pregnancy otherwise you may give this a miss. The routine urine tests, blood pressure check-up and the measurement of the uterus may take place. You may be given more information in case your pregnancy may be expected to go beyond 41 weeks.
12. Week 41
Though most women may go through labour during this time, however, sometimes women can experience no signs of labour till this time. In such cases, your doctor may offer you a membrane swipe. In case of first-time pregnancy, you may have had a membrane swipe once before at around 40 weeks antenatal visit. However, your doctor will ask you before conducting a membrane swipe again, and it may be totally your call. Apart from this, standard urine and blood work will be conducted. In the case of membrane sweep not being successful, your doctor may suggest you go for an induction. However, the decision always lies with you. If you do not wish to go ahead with labour induction, you may be offered regular monitoring by your doctor and midwife till you may go into labour.
Your doctor and midwife monitor your pregnancy to detect any risk factors that may affect your baby or you during your pregnancy journey. However, if you are facing any medical complications such as diabetes , hypertension or others, then your pregnancy may be closely monitored by your doctor and midwife.
Common Trimester Wise Tests during Pregnancy
- RELATED ARTICLES
- MORE FROM AUTHOR

40 Weeks Pregnant and No Signs of Labor - Should You Worry?

Cervical Cancer During Pregnancy

Using Nasal Decongestant Spray during Pregnancy - Is It Safe?
Period During Pregnancy - Myths Busted

Awesome Disney Themed Baby Shower Ideas

6 Weeks Ultrasound: Procedure, Abnormalities and more
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.
Father's Day Coloring Pages - Free Printables For Kids
Happy father's day animated gifs worth sharing.

Spiderman Coloring Pages - Free Printable Pages For Kids

Hamster Coloring Pages - Free Printable Pages For Kids
Doctor Visits
Find and Access Preventive Services

Take Action
Preventive services include health care like screening tests, checkups, and vaccines. Unlike the care you get when you’re sick or managing a long-term condition, preventive care can help stop you from getting sick in the first place — or it can find health problems before they get worse, even before you have symptoms.
Why do I need preventive care?
There are lots of great reasons to get preventive care. It can:
- Save your life. Screening tests and checkups can find health problems early, when they may be easier to treat. This includes serious diseases like cancer.
- Prevent disease . Some preventive services can keep health problems from developing. This includes vaccines and screenings for certain cancers, like cervical cancer.
- Help you save money . Finding and treating health problems early can help you avoid costly medical bills down the road. Plus, most insurance plans cover preventive services, and there are free or low-cost options if you don’t have insurance.
- Offer peace of mind. Regular checkups are a chance for you to share concerns and ask questions about your health — and to get support from a doctor or other health care professional.
How to Get Preventive Care
Make an appointment with your doctor..
Talking with your doctor or nurse is a great first step to getting preventive care. They can tell you which screenings, vaccines, or other services you need — and answer any questions you may have. Together, you can make a plan to protect your health.
Looking for a new doctor or nurse? Use these tips to find the right fit .
Find free or low-cost preventive care.
Most health insurance plans cover preventive services at no cost to you — usually without a copay or deductible.
But even if you don’t have health insurance, you can still get free or low-cost preventive care. Try these tips:
- Visit a community health center or clinic. Community health centers and clinics can offer affordable — or even free — preventive care. Find a health center near you .
- Contact your local health department. Many health departments offer free health services, like flu vaccines, to people in the community. Your health department can also give advice on where to find additional free or low-cost health care services in your area. Use this interactive map to find your local health department.
- Look for volunteer clinics. Some communities offer free clinics run by volunteers for people who don’t have health insurance. Find a volunteer clinic near you.
- Ask your local hospital about free screenings. Many hospitals offer free screening events. Contact your hospital’s customer service or community outreach department to learn what options are available.
If you’re getting health care through the Indian Health Service (IHS), use this tool to find preventive care near you. And if you’re a Veteran, you can get care at a VA location in your area.
Look for free screening and testing programs for specific diseases.
There are also some free or low-cost programs to help you get screened or tested for specific diseases. For example:
- Screening for breast and cervical cancer: National Breast and Cervical Cancer Early Detection Program (NBCCEDP)
- Testing for HIV, STIs (sexually transmitted infections), and hepatitis: Get Tested search tool
Learn about insurance coverage for preventive services.
If you have private health insurance:.
Private health insurance means you’re getting your insurance through an employer or the Health Insurance Marketplace. Under the Affordable Care Act, private health insurance plans must cover many preventive services. Depending on your insurance plan and other factors like your age, you may be able to get these and other preventive services at no cost to you:
- Blood pressure , diabetes , and cholesterol tests
- Many cancer screenings, including mammograms and colonoscopies
- Counseling on topics like quitting smoking , losing weight , eating healthy , treating depression , and drinking less alcohol
- Vaccines to protect against diseases like the flu, whooping cough, measles, and meningitis
- Counseling, screening, and vaccines to help you have a healthy pregnancy
- Regular well-baby and well-child visits
Keep in mind that you may be charged a portion of the cost if a preventive service isn’t the main reason for your doctor’s visit or if you’re seeing an out-of-network provider. To avoid unexpected medical bills, ask your doctor before your appointment what services will be covered — or check with your insurance company.
To learn more, check out these resources about:
- Free preventive care covered by the Affordable Care Act
- How the Affordable Care Act protects you
- Understanding your health insurance and how to use it [PDF - 698 KB]
If you have Medicaid:
Medicaid covers certain preventive services at no cost, like vaccines and recommended screenings and tests. It also covers counseling to help you manage long-term health conditions and support healthy changes, like quitting smoking. You can:
- Find out more about getting preventive care through Medicaid
- Contact your state’s Medicaid agency for detailed information
If you have Medicare:
Medicare also covers certain preventive services at no cost. To learn about Medicare and preventive care:
- Browse this list of covered services
- Use this tool to see what Medicare covers
If you’re uninsured, explore options for getting health insurance.
There are different options for getting health insurance coverage — and it may be more affordable than you think. To get started, you can:
- Check to see if you’re eligible for Medicaid. The Medicaid program provides health insurance for families with low incomes, pregnant people, people with disabilities, and people in certain other groups. Find Medicaid coverage in your state.
- Enroll your children in CHIP. The Children’s Health Insurance Program (CHIP) covers children in families that earn too much money to qualify for Medicaid but not enough to afford private health insurance. Learn more about CHIP.
- Explore the Health Insurance Marketplace. The Marketplace offers health insurance plans for anyone who needs it. How much you’ll pay for coverage depends on how much money your family earns. Read this quick guide to Marketplace coverage or find local help.
Content last updated June 7, 2024
Reviewer Information
This information on preventive services was adapted from materials from the U.S. Department of Health and Human Services and the Centers for Medicare & Medicaid Services.
Reviewed by: U.S. Department of Health and Human Services’ Office of Disease Prevention and Health Promotion Review Team.
You may also be interested in:

Get Screened

Take Charge of Your Health Care

Get Your Medicare Wellness Visit Every Year
The office of disease prevention and health promotion (odphp) cannot attest to the accuracy of a non-federal website..
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Appointments at Mayo Clinic
- Pregnancy week by week
- Healthy pregnancy
- First trimester
- Second trimester
- Third trimester
- Pregnancy problems
The first few months of pregnancy — the first trimester — are marked by rapid changes.
During the first trimester, physical changes may include breast tenderness, fatigue and nausea. Emotions might range from excitement to anxiety. For the fetus, the first trimester is a time of rapid growth and development. The brain, spinal cord and other organs are forming. The heart begins to beat. Fingers and toes begin to take shape.
When you find out you're pregnant, make an appointment with your health care provider to begin prenatal care. You'll learn what to expect during the first trimester and beyond.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Bastian LA, et al. Clinical manifestations and diagnosis of early pregnancy. https://www.uptodate.com/contents/search. Accessed Oct. 18, 2022.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed Oct. 18, 2022.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed Oct. 18, 2022.
- Chasen ST. Twin pregnancy: Routine prenatal care. https://www.uptodate.com/contents/search. Accessed Oct. 18, 2022.
- Lockwood CJ, et al. Prenatal care: Patient education, health promotion, and safety of commonly used drugs. https://www.uptodate.com/contents/search. Accessed Oct. 18, 2022.
- Stages of pregnancy. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/stages-pregnancy. Accessed Oct. 18, 2022.
Products and Services
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- Available Compression Products from Mayo Clinic Store
- Assortment of Compression Products at Mayo Clinic Store
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 1st trimester pregnancy
- Second trimester pregnancy
- 3rd trimester pregnancy
- Air travel during pregnancy
- Allergy medications during pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Antidepressants and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Pregnancy bed rest
- Can birth control pills cause birth defects?
- Blighted ovum: What causes it?
- Cervical length
- Chickenpox and pregnancy
- Depression during pregnancy
- Miscarriage and stress
- Epilepsy and pregnancy
- Falling during pregnancy: Reason to worry?
- Fetal development 2nd trimester
- Fetal development: The 1st trimester
- Fetal development: The 3rd trimester
- Fetal presentation before birth
- Fetal ultrasound
- Flu shot in pregnancy
- Fundal height and fetal growth
- Headaches during pregnancy: What's the best treatment?
- Heart conditions and pregnancy
- Hemorrhoids during pregnancy
- High blood pressure and pregnancy
- High-risk pregnancy
- How do ankylosing spondylitis and pregnancy affect each other?
- Implantation bleeding
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Low amniotic fluid
- Nausea during pregnancy
- New Test for Preeclampsia
- Overdue pregnancy
- Pregnancy acne
- Pregnancy and atrial fibrillation
- Pregnancy and fish
- Pregnancy and obesity
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Pregnancy and COVID-19
- Prenatal care: 1st trimester
- Prenatal care: 2nd trimester visits
- Prenatal care: 3rd trimester
- Prenatal testing
- Prenatal vitamins and pregnancy
- Rheumatoid arthritis: Does pregnancy affect symptoms?
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Vulvar varicosities during pregnancy: What can you do?
- Working during pregnancy
- X-ray during pregnancy
- Yeast infection during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.

Ver esta página en español | 閱讀此頁面的繁體中文版本 | 阅读本页的简体中文版本
Go to: Find a Provider | Payment and Support | Access for Immigrants | Health Privacy | Avoid Fake Clinics | Options Counseling | Types of Abortion
Abortion Access Hub
The New York City Abortion Access Hub provides confidential help finding an abortion provider in New York City, scheduling an appointment, getting financial assistance, and finding transportation and lodging. This help is available regardless of immigration status. You do not need to live in New York City to contact the Abortion Access Hub or receive a referral.
- Phone: 1-877-NYC-AHUB (1-877-692-2482)
- Hours: Monday through Friday, 8 a.m. to 8 p.m.
The Hub does not collect or record any of your identifying information, and your phone number will be hidden.
What To Expect
When you contact the Abortion Access Hub, you will be connected to a staff member who will ask you simple questions to assess how far along your pregnancy is, what type of abortion service you prefer, what borough you would like services in, and when.
When you call, you will also be asked if you have health insurance and if you need financial assistance, or help finding lodging and transportation. The Hub can make an appointment for you. Interpretation services are available.
When you use the live chat, you will be asked if you have health insurance. Based on your responses, you will be given a list of providers to call so that you can make your appointment. Chat is only available in English and Spanish.
Abortion is a safe, common health care service to end a pregnancy. In the U.S., one in four women will have an abortion by the age of 45 . Some states have more restrictive abortion laws.
You can get an abortion regardless of your immigration status, even if you do not have insurance.
In New York, you can get an abortion for any reason up to 24 weeks of pregnancy, or later if your health is at risk or your pregnancy will not survive. If you need an abortion and are uncertain about how far along in the pregnancy you might be, you may call or visit an abortion provider to determine if you are eligible.
Other states can also provide abortion services later in a pregnancy for any reason.
If you are a teenager, you can get sexual health services, including abortion care, at a clinic without your parents' permission or knowledge.
You have a right to receive abortions or other medical care in your preferred language, including through the use of interpreter services.
Any person who can get pregnant — including transgender men, non-binary people and people of any gender who have a uterus — can have an abortion.
The decision to have an abortion is a personal one. No one should pressure you to have or not have an abortion.
- Abortion in New York State: Know Your Rights
- The New York Attorney General’s Office offers residents and visitors with free legal information and resources about accessing abortion through a free hotline at 212-899-5567.
- If/When/How's Repro Legal Helpline offers people who are seeking abortion care or recently had an abortion free, confidential legal advice and information at 844-868-2812.
Find a Provider
You can get an abortion at many health centers in New York City.
To find abortion providers:
- In New York City, call the NYC Abortion Access Hub at 1-877-NYC-AHUB (1-877-692-2482)
- In New York City, as well as throughout the U.S., visit National Abortion Federation , ineedana.com or Abortion Finder
If you are looking for abortion services after 24 weeks, visit the Later Abortion Initiative .
Payment and Support Resources
Whether you have health insurance or no insurance, there are options to help you pay for abortion services.
Health Insurance
If you are a New York State resident and have Medicaid, you can go to any medical provider that accepts Medicaid and offers the services you need. If you have other types of health insurance, contact your health insurer to find out what your plan covers, whether a prior authorization is needed or if there are specific providers your plan covers.
The NYC Abortion Access Hub may also be able to connect you to an abortion provider that accepts your insurance.
If you plan to travel from another state to New York for abortion care and have insurance including Medicaid, contact your plan to see if they will cover out-of-network services and travel expenses. If they do not, you can find support resources below . Abortion Access Hub Navigators may also be able to connect you to an abortion provider that can offer financial help.
No Insurance
If you are pregnant and live in New York, you may have health insurance options. New York State Medicaid will pay for the care you receive while pregnant, including abortion care. Pregnant New Yorkers can qualify for Medicaid at higher income levels and regardless of immigration status. To learn more or get connected to an enrollment counselor to schedule an in-person or phone appointment, visit the Health Insurance page , text “CoveredNYC” (“SeguroNYC” in Spanish) to 55676, or fill out the Health Insurance Enrollment Assistance Inquiry form .
Some medical offices can check if you qualify for Medicaid at the time of your appointment. If you qualify, they can also enroll you, with coverage starting the same day. Before your appointment, ask your medical office if they are a Medicaid enrollment site. Be sure to ask if they require a photo ID or other documents. The NYC Abortion Access Hub can also connect you to an abortion provider that can enroll you in Medicaid if you live in New York.
Help with Paying for Abortion
If you do not qualify for insurance, your insurance does not cover abortion services or your insurance has high out-of-pocket costs, contact the organizations below. You do not need to be a New York resident to use these resources:
- National Abortion Federation , or call its hotline at 800-772-9100
- New York Abortion Access Fund , or call its hotline at 212-252-4757
- National Network of Abortion Funds
- AbortionFinder.Org
These organizations will not ask about your immigration status.
For help with travel or lodging costs, you can connect with practical support organizations. These organizations generally require that you have an appointment to receive care at one of their partner clinics.
- Brigid Alliance provides help with travel, food, lodging, child care and other logistical support. Brigid prioritizes clients beyond 15 weeks of pregnancy.
The NYC Abortion Access Hub can connect you to an abortion provider in NYC that can help you identify funds and practical support for your abortion care.
Access for Immigrants
In New York state, you can receive an abortion regardless of your immigration status, even if you do not have insurance. Getting an abortion in New York will not affect your immigration status. Immigrants can travel state to state for health services, including abortion. However, border patrol checkpoints require lawful status to pass through.
Pregnant non-citizens who live in New York are eligible for Medicaid regardless of immigration status if they meet income requirements.
Abortion funds can help pay for abortions even if you do not have insurance, and they do not ask for immigration status.
Hospitals and other medical facilities are considered protected areas where immigration enforcement officials do not engage in enforcement activities, except in very limited circumstances.
Protect Your Health Privacy
The U.S. Department of Health and Human Services released new federal guidance in June to help protect your geolocation and other personal data on period trackers and other health information apps.
If you believe that a company or organization is violating people's health privacy rights, you can file a complaint online .
- HHS: Protecting the Privacy and Security of Your Health Information When Using Your Personal Cell Phone or Tablet
Avoid Fake Clinics
There are anti-abortion facilities — sometimes called crisis pregnancy centers or pregnancy resource centers — that try to stop people from getting abortions.
Fake clinics that try to stop people from getting abortions will often show up in results of online searches for "abortion clinic" or "abortion pill". Use the resources on this page to avoid those places and find an abortion provider who respects your right to seek abortion services.
These fake clinics often:
- Imitate health clinics by using names, banners and signs that are similar to real clinics.
- Are located near health clinics that provide abortions.
- Are funded by organizations that are opposed to abortion.
- Provide false information about abortion to pregnant people.
- Try to mislead people about how many weeks they have been pregnant.
- Claim to offer free counseling, pregnancy tests and ultrasounds.
Fake clinics may offer low-cost resources, such as pregnancy tests, ultrasounds or baby clothes, but they do not provide abortions. Also, they rarely offer any other medical care. Since they are not licensed health care providers, these facilities are not required by law to keep your personal information private.
New York City law requires these facilities to post a sign in English and Spanish that states they do not have a medical provider on site and do not provide abortion care. If you encounter a fake clinic without this sign posted in English and Spanish, you can file a complaint online or by calling 311 .
Learn more about fake clinics in NYC:
- Pro-Truth NY Fake Clinic Map
- NIRH Research Report: Crisis Pregnancy Centers (PDF)
Options Counseling
If you are pregnant and unsure what to do or how to feel, you have options and can seek support as you make decisions. Free, non-judgmental counseling options include:
- All Options offers judgement-free counseling and guidance to help you make the right decisions for yourself.
- NYC Well provides mental health support, if making these decisions causes stress.
Types of Abortions
There are two types of abortions — medication and procedural.
Your provider may recommend a certain abortion type based on your preference, your medical history and the number of weeks since your last menstrual period.
This option, also called a medical abortion, involves taking two medicines — mifepristone and misoprostol.
- Process: You take mifepristone on the first day and misoprostol on the second day. The pills on the second day cause cramping and vaginal bleeding, similar to a heavy period.
- Timing: You can get abortion pills at up to 11 weeks of pregnancy, but the earlier you take them the more effective they are.
- Effectiveness: This method is 91% to 98% effective at ending a pregnancy.
- Side effects: These are usually mild and last between a couple of days and two weeks. They can include cramping, spot bleeding and nausea/vomiting. If you are having more severe side effects, call your provider immediately.
Oral Medicine by Mail
Ask your provider if they offer telehealth and can mail the abortion medication to you.
The FDA recently announced people can get medication for abortion by mail. Previously, people were only able to get it in-person from a health care provider. Contact a provider to find out if this option would work for you.
This option, also called “in-clinic abortion”, is an outpatient procedure, which means you can go home after it is over.
- Process: The type of procedure used is based on how long you have been pregnant. The most common type involves widening the cervix and using gentle suction to remove pregnancy tissue. You may experience some cramping. This procedure is quick and usually takes less than 10 minutes, but you should expect to spend several hours at the provider’s office. If the pregnancy is more than 16 weeks, the procedure may take place over two consecutive days.
- Timing: Depending on the specific procedure, you can receive a procedural abortion from five weeks since your last period.
- Effectiveness: This method is more than 99% effective at ending a pregnancy.
- Side effects: These are usually mild and last up to two weeks. They may include cramping, bleeding, spot bleeding and vaginal discharge. If you are having more severe side effects, call your provider immediately.
Additional Resources
- Charley, the Abortion Chatbot
- Report on Language Access Needs for Abortion Services (PDF)
- Abortion Hub Info Sheet (PDF) Other Languages: Español | Русский | 繁體中文 | 简体中文 | Kreyòl ayisyen | 한국어 | বাংলা | Italiano | Polski | العربية | Français | ײִדיש | اردو
- Abortion Hub Poster (PDF) Other Languages: Español | Русский | 繁體中文 | 简体中文 | Kreyòl ayisyen | 한국어 | বাংলা | Italiano | Polski | العربية | Français | ײִדיש | اردو
- Abortion Hub Card (PDF) Other Languages: Español | Русский | 繁體中文 | 简体中文 | Kreyòl ayisyen | 한국어 | বাংলা | Italiano | Polski | العربية | Français | ײִדיש | اردو
- Abortion Hub Materials Order Form (PDF)
- New York State: Reproductive Rights Hotline
- Planned Parenthood: Abortion Services
- The Center For Reproductive Health Education In Family Medicine: Comparison of Early Abortion Options (PDF)
- The Doula Project: Self-Care for Before, During and After Your Abortion (PDF)
- Shout Your Abortion : Destigmatization and advocacy
- Exhale: A Pro-Choice, After-Abortion Chatline , or text their chat line at 617-749-2948.
More Information
- Sexual and Reproductive Justice Framework
- Sexual Health
- Sexual Consent
- Sexual Health Clinics
- NYC Teens Connection
- Birth Control
Security Alert May 17, 2024
Worldwide caution, update may 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Get a Passport
Renew or Replace a Passport
Get My Passport Fast
Prepare to Apply
Passport Help
Legal Matters
Get a Passport Homepage
Share this page:
Apply for your First Adult Passport
Apply for a Child Under 16
Apply as a 16 or 17 Year Old
Get My Application Status
Get a Passport Card
Respond to a Letter or Email
- Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person.
- If one or both parents or guardians cannot apply with their child, you will need to show us more documents.
- You cannot renew your child's passport using Form DS-82.
- Passports for children under age 16 are only valid for 5 years.
Steps to Apply
1. fill out form ds-11 and print it.
Use our Form Filler tool to fill out your child's form on a desktop or laptop computer and then print it. If you are experiencing technical issues with the Form Filler, download a PDF .

Tips to complete your child's form :
- Do not sign your child's form until asked to do so by a passport acceptance agent or employee.
- You can apply for a passport book , a passport card , or both documents.
- You may ask for a larger passport book with more visa pages, at no extra cost, by checking the 'large book' box at the top of the DS-11.
2. Get Evidence of U.S. Citizenship (and a photocopy)
Your evidence must be an original or replacement copy. The document must have the official seal or stamp of the office which issued it. You must submit one of the following documents for your child:
- Issued by the city, county, or state of birth
- Lists applicant's full name, date of birth, and place of birth
- Lists the parent(s)' full names
- Has the date filed with registrar's office (must be within one year of birth)
- Has the registrar's signature
- Has the seal or stamp of the city, county, or state which issued it
- Consular Report of Birth Abroad or Certification of Birth
- Certificate of Citizenship
- Please note you must also provide a document, such as a birth certificate, that lists the parent(s) or legal guardian(s) of the child. Full validity means the document is or was valid for 10 years for adults and 5 years for children under 16.
If you cannot submit one of these documents, go to our Citizenship Evidence page for more information.
Paper only : You cannot submit digital evidence of U.S. citizenship such as a mobile or electronic birth certificate. You must submit physical evidence of U.S. citizenship and a photocopy of the document.
Returning your child's document : We will return your child's document in a separate mailing up to 8 weeks after you receive the new passport.
Tips for making a photocopy :
- Black and white (no color)
- Use 8.5 inch by 11 inch paper
- Use a single side of the paper
If you do not submit a photocopy, you must submit a second copy of your citizenship evidence. We will keep this copy for our records.

3. Show Your Relationship to Your Child
You must submit a document that lists the parent(s) or legal guardian(s) of the child. Examples include:
- U.S. birth certificate (also evidence of U.S. citizenship)
- Foreign birth certificate
- Adoption decree
- Divorce or custody decree
- A court order
Some documents, like a U.S. birth certificate, show both U.S. citizenship and parental relationship. These documents must be originals or certified copies (not photocopies).
You and your child may have different last names, as long as the document showing your relationship to your child lists your full name.
If your name is different than the one on the document showing your relationship to your child, submit proof of your legal name change.
4. Get a Photo ID (and a photocopy)
Both parents or guardians must bring a physical, photo ID and a photocopy of it. If your photo ID is from a different state than the state in which you are applying, bring a second photo ID.
You must show at least one of these photo IDs:
- Valid or expired, undamaged U.S. passport book or passport card
- In-state, fully valid driver's license or enhanced driver's license with photo
- Certificate of Naturalization
- Certificate of Citizenship
- Government employee ID (city, county, state, or federal)
- U.S. military or military dependent ID
- Current (valid) foreign passport
- Matricula Consular (Mexican Consular ID) used by a parent of a U.S. citizen child applicant
- U.S. Permanent Resident Card (Green Card) used by a parent of a U.S. citizen child applicant
- Trusted Traveler IDs (including valid Global Entry, FAST, SENTRI, and NEXUS cards)
- Enhanced Tribal Cards and Native American tribal photo IDs
- In-state, fully-valid learner's permit with photo
- In-state, fully-valid non-driver ID with photo
- Temporary driver's license with photo
If you do not have one of these photo IDs, go to our Identification page for more information.
5. Show More Documents (if both parents or guardians cannot apply)
- Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person.
- If one or both parents or guardians cannot apply in person with their child, you will need to show more documents.
Important : Submit Form DS-3053 and other notarized statements within three months of signing them.
6. Provide a Photo
You must provide one photo with your child's application. Go to our Passport Photo page for photo requirements and to see examples of photos.
- Do not attach or staple your child's photo to the form. The acceptance agent or passport employee will review the photo and staple it to your form.
- Some passport acceptance facilities
- A company which offers photo services
- Home. Ask your friend or family member to take your child's photo. Print it on glossy or matte photo quality paper.
7. Calculate Fees
When applying using Form DS-11, you will pay two separate fees - an application fee and an execution (acceptance) fee. You will pay the application fee to the U.S. Department of State, and the execution (acceptance) fee to the facility which takes your application.
- Add $60 to your application fee if you want expedited service .
- Add $19.53 to your application fee if you want us to ship your completed passport in 1-2 days after we issue it.
Child Applicants :
For more information on how to pay and a full list of fees, go to our Passport Fees page.
*How to fill out your check and pay the application fee to the U.S. Department of State. Please note you must pay a separate execution (acceptance) fee.
Families may write one check or money order to the U.S. Department of State if they are applying at the same time. The check or money order must include the name and date of birth of each applicant.
8. Find Location to Apply
In the United States:
- Traveling in more than 3 weeks? Go to a passport acceptance facility such as a post office, library, or local government office. Check with the facility to see if you need to make an appointment.
- Traveling in less than 3 weeks? Make an appointment to apply at a passport agency or center.
In another country:
- Contact your U.S. embassy or consulate .
9. Track Your Application Status
You can subscribe to email updates about your application status, and learn more about each status update .
It may take 2 weeks from the day you apply until your child's application status is “In Process.”
Frequently Asked Questions
How will you send my child's passport and supporting documents.
You will get multiple mailings. The number of mailings depends on what document(s) you asked for.
Passport Book : You may get your new passport and citizenship documents in two mailings. You may wait 8 weeks after getting your passport before you get a second mailing with your citizenship documents. We will return the passport book using a trackable delivery service.
Passport Card : You may get your new passport card and your citizenship documents in two mailings. You may wait 8 weeks after getting your passport before you get a second mailing with your citizenship documents. We only send the passport card via First Class Mail. We do not send cards using 1-2 day delivery services.
Both a Passport Book and Card : You may get three separate mailings:
- New passport book
- New passport card
- Citizenship documents
Contacting Us : If you have been waiting more than 8 weeks for your documents, call us at 1-877-487-2778 to report that you have not received your documents.
If you want us to reimburse you for a lost supporting document, you must contact us within 90 days of the date which we mailed your passport. You will also need to provide a receipt to show the cost of replacing the document.
Can I pay for faster delivery and return shipping?
Yes. You may choose one or both of the following shipment options:
- Delivering application to us : Pay for Priority Mail Express for faster shipping. The price for this service varies depending on the area of the country.
- Returning the passport to you : Pay $19.53 for 1-2 day delivery. This means you will receive your passport 1-2 days after we send it. Include this fee with your check or money order payable to the U.S. Department of State. Do not submit a return envelope to us with postage pre-paid.
You may receive your passport and supporting documents in separate mailings. If you are renewing a passport card, we will send it to you via First Class Mail. We do not use 1-2 day delivery services if you only applied for a passport card.
What countries require Form DS-3053 "Statement of Consent" to be notarized at an embassy or consulate?
In certain countries, a DS-3053 must be notarized at a U.S. embassy or consulate and cannot be notarized by a local notary public. Currently, these countries include:
Special Passport Fairs
Find a Special Passport Fair near you!
We're holding special passport fairs all across the United States to help you get your passport more easily. New events are added to our site every week.
Most events are for first-time applicants and children, (who use Form DS-11). If you can use Form DS-82, you can renew by mail at your convenience!
Processing Times
Routine: 6-8 weeks*
Expedited: 2-3 weeks and an extra $60*
*Consider the total time it will take to get a passport when you are booking travel. Processing times only include the time your application is at a passport agency or center.
- It may take up to 2 weeks for applications to arrive at a passport agency or center. It may take up to 2 weeks for you to receive a completed passport after we print it.
- Processing times + mailing times = total time to get a passport
Urgent Travel: See our Get my Passport Fast page.
How to Apply for your Child's Passport
Watch this video to learn how to apply in person for your child's U.S. passport!
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

Sexually Transmitted Infections Treatment Guidelines, 2021
CDC’s Sexually Transmitted Infections (STI) Treatment Guidelines, 2021 provides current evidence-based prevention, diagnostic and treatment recommendations that replace the 2015 guidance. The recommendations are intended to be a source for clinical guidance. Healthcare providers should always assess patients based on their clinical circumstances and local burden.
Now available for Apple and Android devices.
View the full STI Treatment Guidelines.
Access print-friendly versions of the wall chart, pocket guide, and guidelines.
Explore STD trainings, technical assistance, clinical consultation services, and more.

View tables of screening recommendations by disease or by population.
- Suspected Gonorrhea Treatment Failure Consultation Form
- Mycoplasma genitalium Treatment Failure Registry
- Customizable Announcement
- Screening Recommendations
- Tables of Evidence
- Dear Colleague Letter
- A Guide to Taking a Sexual History
- Expedited Partner Therapy
- Availability of STI Testing & Treatment Products
- Prenatal Syphilis Screening Laws
- National STD Curriculum
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
quality care throughout the pregnancy, childbirth and the postnatal period. Within the continuum of reproductive health care, antenatal care (ANC) provides a platform for important health-care functions, including health promotion, screening and diagnosis, and disease prevention. It has been established that by implementing timely
An important element in this continuum of care is effective antenatal care. The goal of the antenatal care package is to prepare for birth and parenthood as well as prevent, detect, alleviate, or manage the three types of health problems during pregnancy that affect mothers and babies: Antenatal care also provides women and their families with ...
Eight or more contacts for antenatal care can reduce perinatal deaths by up to 8 per 1000 births when compared to 4 visits. A woman's 'contact' with her antenatal care provider should be more than a simple 'visit' but rather the provision of care and support throughout pregnancy. The guideline uses the term 'contact' as it implies ...
Background. Approximately 303,000 women and adolescent girls died from pregnancy and childbirth-related complications in 2015.1 That same year, 2.6 million babies were stillborn. Almost all of the maternal deaths (99%) and child deaths (98%) occurred in low- and middle-income countries.
ANC Visit schedule: Pregnancy should be detected by clinical examination / urinary pregnancy test / Ultra sound • Registration: o As early as pregnancy is suspected / diagnosed • At least 4 antenatal visits during all three (3) trimesters Visit Time line 1st ANC In first trimester i.e. first 12 weeks 2nd ANC Between 14 - 26 weeks
Antenatal care (also termed prenatal care) is one of the most common preventive health services in the United States, accessed by about 4 million women annually.1 Antenatal care aims to improve the health and wellbeing of pregnant patients and their babies through (1) medical screening and treatment; (2) anticipatory guidance; and (3) psychosocial support.2, 3 The World Health Organization's ...
Overview . This comprehensive WHO guideline provides global, evidence-informed recommendations on routine antenatal care. The guidance aims to capture the complex nature of the issues surrounding ANC health care practices and delivery and to prioritize person-centred health and well-being, not only the prevention of death and morbidity, in accordance with a human rights-based approach.
The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine plan a new evidence-based joint consensus statement to address the preferred visit schedule and the use of televisits for routine antenatal care. This systematic review will support the consensus statement. We searched PubMed ®, Cochrane ...
Antenatal care (ANC) is the care of the woman during pregnancy. The primary aim of ANC is to promote and protect the health of women and their unborn babies during ... Another visit around six weeks postpartum is also highly recommended The care providers Postpartum care starts right after the delivery. If the delivery occurs in a health ...
Guideline. Antenatal Care Schedule: hospital-led care. 1. Purpose. This guideline outlines the antenatal care schedule and care strategies for women receiving antenatal care at the Women's. A summary is provided for the clinical and educational content to be covered at each visit. See the Shared Maternity Care schedules for women accessing ...
2016 WHO Antenatal Care Guidelines: Malaria in Pregnancy Frequently Asked Questions (FAQ) 1 ... include the more familiar model of clinic-based ANC visits, as well as ANC care and/or counseling sessions for pregnant women at the household and community levels. ... # This schedule is a suggested adaptation of the WHO ANC schedule for countries ...
Expert consensus and past meta-analyses have favored fewer antenatal care visits given similar maternal and neonatal outcomes. In 1989, the U.S. Public Health Service suggested a reduction in the ...
As per 4 schedule visits by the WHO FANC model and the country guideline 8%(203) and 20%(543) women respectively received the first 2 timely ANC by a MTP; where only 1%(32) and 3%(72) received the first 3 visits timely and 0.6%(17) and 1%(29) received all the four timely visits. ... Early antenatal care visit: a systematic analysis of regional ...
9 months. 36-38 weeks. All pregnant women should have 4 routine antenatal visits. First antenatal contact should be as early in pregnancy as possible. During the last visit, inform the woman to return if she does not deliver within 2 weeks after the expected date of delivery.
Group antenatal care E.3: Group antenatal care provided by qualifi ed health-care professionals may be off ered as an alternative to individual antenatal care for pregnant women in the context of rigorous research, depending on a woman's preferences and provided that the infrastructure and resources for delivery of group antenatal care are
As per 4 schedule visits by the WHO FANC model and the country guideline 8%(203) and 20%(543) women respectively received the first 2 timely ANC by a MTP; where only 1%(32) and 3%(72) received the first 3 visits timely and 0.6%(17) and 1%(29) received all the four timely visits. ... Petzold M, Chou D, Say L. Early antenatal care visit: a ...
Balk EM, Konnyu KJ, Cao W, Reddy Bhuma M, Danilack VA, Adam GP, Matteson KA, Peahl AF. Schedule of Visits and Televisits for Routine Antenatal Care: A Systematic Review. Comparative Effectiveness Review No. 257. (Prepared by the Brown Evidence-based Practice Center under Contract No. 75Q80120D00001.) AHRQ Publication No. 22-EHC031.
Antenatal care schedule . Page 8 of 20 Obstetrics & Gynaecology . Family and . Fetal morphology ultrasound • Offer a fetal morphology ultrasound to all women. Anatomy scans may be booked at the KEMH Diagnostic Imaging Department, however whenever practical refer the woman to her GP to arrange an ultrasound at another metropolitan service.
Discuss and plan the schedule of antenatal visits with the pregnant woman based on her individual needs. For an uncomplicated pregnancy, 10 visits are recommended for women having their first pregnancy, and seven visits for women having subsequent pregnancies. At first antenatal visit. IB. Module 1, section 6.
We shall now discuss week-wise prenatal appointment schedule or prenatal care schedule that you may have to keep up with. 1. Week 8 to 12. This may be your first antenatal visit, and this should ideally happen before 10 weeks of pregnancy. In this visit you may be asked the following details: Your lifestyle and diet.
Dizziness. Weakness. Extreme tiredness. Nervousness or worry that makes it hard for you to do your daily activities. Overwhelming feelings of sadness or sadness that lasts. Thoughts of harming yourself or your baby. Having a high-risk pregnancy may be stressful and cause you to worry about your baby's health.
Recommended vaccination for adults with an additional risk factor or another indication. Recommended vaccination based on shared clinical decision-making. No recommendation/Not applicable. adult vaccine schedule. Vaccine. 19-26 years. 27-49 years. 50-64 years. ≥65 years.
The number of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times during pregnancy is expressed as a percentage of women aged 15-49 with a live birth in the same period (number of women aged 15-49 attended at least four times during pregnancy by any provider for reasons related to the pregnancy/total number of women aged 15-49 with a live ...
The abortion pill is very effective. If you're taking mifepristone and misoprostol, it depends on how far along the pregnancy is, and how many doses of medicine you take: At 8 weeks pregnant or less, it works about 94-98% of the time. At 8-9 weeks pregnant, it works about 94-96% of the time. At 9-10 weeks pregnant, it works about 91-93% of ...
It can: Save your life. Screening tests and checkups can find health problems early, when they may be easier to treat. This includes serious diseases like cancer. Prevent disease. Some preventive services can keep health problems from developing. This includes vaccines and screenings for certain cancers, like cervical cancer. Help you save money.
Vigilant antenatal care Monitor urinary protein MO visits at 28, 32, and 36 weeks minimum Timely referral to O&G Clinic, if clinically indicated If there is a previous associated history of placenta abruption, poor neonatal outcome or IUFD: Refer to O&G Clinic, after booking If shared care, O&G to provide clear
The first few months of pregnancy — the first trimester — are marked by rapid changes. During the first trimester, physical changes may include breast tenderness, fatigue and nausea. Emotions might range from excitement to anxiety. For the fetus, the first trimester is a time of rapid growth and development.
You can get an abortion at many health centers in New York City. To find abortion providers: In New York City, call the NYC Abortion Access Hub at 1-877-NYC-AHUB (1-877-692-2482) In New York City, as well as throughout the U.S., visit National Abortion Federation, ineedana.com or Abortion Finder. If you are looking for abortion services after ...
Apply for a Child Under 16. Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person. If one or both parents or guardians cannot apply with their child, you will need to show us more documents. You cannot renew your child's passport using Form DS-82.
Print. CDC's Sexually Transmitted Infections (STI) Treatment Guidelines, 2021 provides current evidence-based prevention, diagnostic and treatment recommendations that replace the 2015 guidance. The recommendations are intended to be a source for clinical guidance. Healthcare providers should always assess patients based on their clinical ...