Appointments at Mayo Clinic
- Children's health

What causes car sickness in children and how can I prevent it?
Car sickness is a type of motion sickness. Motion sickness occurs when the brain receives conflicting information from the inner ears, eyes, and nerves in the joints and muscles.
Imagine a young child sitting low in the back seat of a car without being able to see out the window — or an older child reading a book in the car. The child's inner ear will sense motion, but his or her eyes and body won't. The result might be an upset stomach, cold sweat, fatigue, loss of appetite or vomiting.
It's not clear why car sickness affects some children more than others. While the problem doesn't seem to affect most infants and toddlers, children ages 2 to 12 are particularly susceptible.
To prevent car sickness in children, you might try the following strategies:
- Reduce sensory input. Encourage your child to look at things outside the car rather than focusing on books, games or screens. If your child naps, traveling during nap time might help.
- Carefully plan pre-trip meals. Don't give your child a large meal immediately before or during car travel. If the trip will be long or your child needs to eat, give him or her a small, bland snack — such as dry crackers and a small drink — before it's time to go.
- Provide air ventilation. Adequate air ventilation might help prevent car sickness.
- Offer distractions. If your child is prone to car sickness, try distracting him or her during car trips by talking, listening to music or singing songs.
- Use medication. If you're planning a car trip, ask your child's doctor about using an over-the-counter antihistamine, such as dimenhydrinate (Dramamine) or diphenhydramine (Benadryl), to prevent car sickness. Both medications work best if taken about an hour before traveling. Read the product label carefully to determine the correct dose and be prepared for possible side effects, such as drowsiness. Nondrowsy antihistamines don't appear to be effective at treating motion sickness.
If your child starts to develop car sickness, stop the car as soon as possible and let your child get out and walk around or lie on his or her back for a few minutes with closed eyes. Placing a cool cloth on your child's forehead also might help.
If these tips don't help or if your child's car sickness makes travel difficult, talk to your child's doctor about other options.
Jay L. Hoecker, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Children’s health information and parenting tips to your inbox.
Sign-up to get Mayo Clinic’s trusted health content sent to your email. Receive a bonus guide on ways to manage your child’s health just for subscribing. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Our e-newsletter will keep you up-to-date on the latest health information.
Something went wrong with your subscription.
Please try again in a couple of minutes
- Concussion in children
- Brunette GW, et al., eds. Motion sickness. In: CDC Yellow Book 2020: Health Information for International Travel. Oxford University Press; 2019. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-by-air-land-sea/motion-sickness. Accessed Feb. 24, 2020.
- Motion sickness. Merck Manual Professional Version. https://www.merckmanuals.com/professional/injuries-poisoning/motion-sickness/motion-sickness#. Accessed Feb. 24, 2020.
- Priesol AJ. Motion sickness. https://www.uptodate.com/contents/search. Accessed Feb. 24, 2020.
- Altmann T, et al., eds. Head, neck, and nervous system. In: Caring for Your Baby and Young Child: Birth to Age 5. 7th ed. Bantam; 2019.
Products and Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Children’s Book: My Life Beyond Autism
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: A Practical Guide to Help Kids of All Ages Thrive
- Acetaminophen and children: Why dose matters
- Bullying Scars
- Predicting a child's adult height
- Children and gender identity
- Cold medicines for kids
- Herd immunity and coronavirus
- COVID-19 in babies and children
- COVID-19 vaccines for kids: What you need to know
- Enterovirus D68 and parechovirus: How can I protect my child?
- Flu shots for kids
- Hand-washing tips
- Iron deficiency in children
- Learning disorders: Know the signs, how to help
- BMI and waist circumference calculator
- Mayo Clinic Minute: Why and when children should be vaccinated
- Mayo Clinic Minute: Why getting vaccinated for the flu is doubly important this season
- Measles vaccine: Can I get the measles if I've already been vaccinated?
- Mental illness in children: Know the signs
- Nutrition for kids: Guidelines for a healthy diet
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Limiting screen time
- Thermometer basics
- Thermometers: Understand the options
- Vaccine guidance from Mayo Clinic
- When to Take Your Child to the E.D.
- Mayo Clinic Minute: Out of shape kids and diabetes
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Car sickness in children Can I prevent it
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Dramamine® For Kids

Dramamine® for Kids is the only medicated motion sickness relief product formulated just for children ages 2-12 from the #1 Pharmacist Recommended Brand.
● Treats symptoms on the spot ● Prevents nausea, dizziness, vomiting & queasiness ● Safe, precise dose in a fun, chewable grape flavor ● Convenient travel case
Available in an 8-count box.
To prevent motion sickness, the first dose should be taken 1/2 to 1 hour before starting activity.
To prevent or treat motion sickness, see below:
- Children 2 to under 6 years: give ½ to 1 chewable tablet every 6-8 hours; do not give more than 3 chewable tablets in 24 hours, or as directed by a doctor
- Children 6 to under 12 years: give 1 to 2 chewable tablets every 6-8 hours; do not give more than 6 chewable tablets in 24 hours, or as directed by a doctor
Other information
- Phenylketonurics: contains phenylalanine 0.375 mg per tablet
- Store at room temperature 20°-25°C (68°-77°F)
Ingredients
Active Ingredient (in each tablet)
Ingredient: Dimenhydrinate 25mg Purpose: Antiemetic
Inactive Ingredients Aspartame, citric acid, flavor, magnesium stearate, methacrylic acide copolymer, sorbitol
Do not use for children under 2 years of age unless directed by a doctor
Ask a doctor before use if the child has:
- A breathing problem such as emphysema or chronic bronchitis
Ask a doctor or a pharmacist before use if the child is taking sedatives or tranquilizers.
When using this product:
- Marked drowsiness may occur
- Avoid alcoholic drinks
- Alcohol, sedatives, and tranquilizers may increase drowsiness
- Be careful when driving a motor vehicle or operating machinery
If pregnant or breast-feeding, ask a doctor before use.
Keep out of reach of children. In case of accidental overdose, get medical help or contact a Poison Control Center (1-800-222-1222) right away.
Comments, Questions or Concerns Call 1-800-382-7219 weekdays or visit us on Facebook
You May Also Like

Dramamine® All Day Less Drowsy

Dramamine® Original Formula

Dramamine® Non-Drowsy
- Telemedicine
- Healthcare Professionals
- Go to MyChart
- Find a Doctor
- Make an Appointment
- Cancel an Appointment
- Find a Location
- Visit ED or Urgent Care
- Get Driving Directions
- Refill a Prescription
- Contact Children's
- Pay My Bill
- Estimate My Cost
- Apply for Financial Assistance
- Request My Medical Records
- Find Patient Education
- Refer and Manage a Patient
Motion Sickness
Is this your child's symptom.
- Dizziness or nausea from spinning or rolling motions
Symptoms of Motion Sickness
- Dizziness and unsteady walking
- Nausea and vomiting are also common
- Before age 6, the main symptom is dizziness and the need to lie down.
- After age 12, the main symptom is nausea (feeling sick to the stomach).
Causes of Motion Sickness
- Symptoms are mainly triggered by motion. Sea sickness or amusement park sickness are the most common types. Fun-park rides that spin or whirl are some of the main causes. The Tilt-a-whirl is a good example of a ride to avoid. Also seen during travel by train, aircraft and even car.
- The cause is a sensitive center in the inner ear. This center helps to maintain balance.
- As a car passenger driving on winding roads, 25% of people will have symptoms. Under extreme conditions (e.g., high seas) over 90% of people have symptoms.
- Strongly genetic: If one parent has it, 50% of the children will have it.
- It is not related to emotional problems. The child cannot control it with will power.
- Motion sickness symptoms are often worse in children.
When to Call for Motion Sickness
Call doctor or seek care now.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Motion sickness symptoms last more than 8 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Motion sickness symptoms
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Federal Way
- Virtual Urgent Care
Care Advice for Motion Sickness
- Motion sickness is a common normal reaction that occurs in 25% of people.
- Caused by increased sensitivity of the inner ear.
- It is not related to emotional problems or any physical disease.
- In the future, take a special medicine ahead of time to prevent it.
- Here is some care advice that should help.
- Have your child lie down and rest. If your child goes to sleep, all the better.
- Give only sips of clear fluids. Water is best. Do this until the stomach settles down.
- Prepare for vomiting. Keep a vomiting pan handy.
- Usually, children don't vomit more than once with motion sickness.
- All symptoms of motion sickness usually go away in 4 hours after stopping the motion.
- As for the future, people usually don't outgrow motion sickness. Sometimes, it becomes less severe in adults.
- Buy some dimenhydrinate tablets (such as Dramamine) at your drug store. No prescription is needed. In the future, give it to prevent motion sickness.
- It comes in 50 mg regular and chewable tablets or in 25 mg Kids chewable tablets.
- Dosage by age: do not use under age 2.
- 2 to 5 years (12.5 mg): ½ Kids chewable
- 6 to 11 years (25 mg): 1 Kids chewable
- 12 and older (50 mg): 1 regular tablet or chewable
- Give the medicine 1 hour before traveling or going to a fun-park.
- The tablets give 6 hours of protection and are very helpful.
- Benadryl can also be used to prevent motion sickness. Use this if you do not have any Dramamine.
- If your child is over 12 years old, sit him in the front seat.
- Before age 12, have your child sit in the middle back seat. This should help him look out the front window.
- Have your child look out the front window, not the side one.
- Discourage looking at books or movies during car travel.
- Keep a window cracked to provide fresh air.
- Avoid exhaust fumes from other vehicles.
- Meals: Have your child eat light meals before trips. Some children can just tolerate crackers and water.
- Plastic Bags: Always carry a ziplock plastic bag for vomiting emergencies.
- Acupressure bands (such as Sea-Bands) are helpful for some adults.
- There is no reason they shouldn't work for some children.
- Put them on before car trips or other causes of motion sickness.
- The pressure button goes over the center of the wrist. Place ½ inch (1 cm) above the wrist crease.
- Any symptoms last over 8 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/11/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
Should your child see a doctor?
Find out by selecting your child's symptom or health condition in the list below:
Seattle Children’s complies with applicable federal and other civil rights laws and does not discriminate, exclude people or treat them differently based on race, color, religion (creed), sex, gender identity or expression, sexual orientation, national origin (ancestry), age, disability, or any other status protected by applicable federal, state or local law. Financial assistance for medically necessary services is based on family income and hospital resources and is provided to children under age 21 whose primary residence is in Washington, Alaska, Montana or Idaho.
By clicking “Accept All Cookies,” you agree to the storing of cookies on your device to enhance site navigation, analyze site usage and assist in marketing efforts. For more information, see Website Privacy .
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
- Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Motion sickness
Travel sickness.
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGP Last updated 16 Mar 2023
Meets Patient’s editorial guidelines
In this series: Health advice for travel abroad Travelling to remote locations Ears and flying Jet lag Altitude sickness
Motion sickness (travel sickness) is common, especially in children. It is caused by repeated unusual movements during travelling, which send strong (sometimes confusing) signals to the balance and position sensors in the brain.
In this article :
What causes motion sickness, how long does motion sickness last, motion sickness symptoms, how to stop motion sickness, natural treatments for motion sickness, motion sickness medicines, what can a doctor prescribe for motion sickness, what should i do if i'm actually sick, what is mal de debarquement syndrome.
Continue reading below
Motion sickness is a normal response to repeated movements, such as going over bumps or around in a circle, send lots of messages to your brain. If you are inside a vehicle, particularly if you are focused on things that are inside the vehicle with you then the signals that your eyes send to the brain may tell it that your position is not changing, whilst your balance mechanisms say otherwise.
Your balance mechanisms in your inner ears sense different signals to those that your eyes are seeing which then sends your brain mixed, confusing messages. This confusion between messages then causes people to experience motion sickness.
Is motion sickness normal?
Motion sickness is a normal response that anyone can have when experiencing real or perceived motion. Although all people can develop motion sickness if exposed to sufficiently intense motion, some people are rarely affected while other people are more susceptible and have to deal with motion sickness very often.
Triggers for motion sickness
Motion sickness can also be triggered by anxiety or strong smells, such as food or petrol. Sometimes trying to read a book or a map can trigger motion sickness. Both in children and adults, playing computer games can sometimes cause motion sickness to occur.
Motion sickness is more common in children and also in women. Fortunately, many children grow out of having motion sickness. It is not known why some people develop motion sickness more than others. Symptoms can develop in cars, trains, planes and boats and on amusement park rides, etc.
Symptoms typically go when the journey is over; however, not always. In some people they last a few hours, or even days, after the journey ends.
There are various symptoms of motion sickness including::
Feeling sick (nausea and vomiting).
Sweating and cold sweats.
Increase in saliva.
Headaches .
Feeling cold and going pale.
Feeling weak.
Some general tips to avoid motion sickness include the following.
Prepare for your journey
Don't eat a heavy meal before travelling. Light, carbohydrate-based food like cereals an hour or two before you travel is best.
On long journeys, try breaking the journey to have some fresh air, drink some cold water and, if possible, take a short walk.
For more in-depth advice on travelling generally, see the separate leaflets called Health Advice for Travel Abroad , Travelling to Remote Locations , Ears and Flying (Aeroplane Ear) , Jet Lag and Altitude Sickness .
Plan where you sit
Keep motion to a minimum. For example, sit in the front seat of a car, over the wing of a plane, or on deck in the middle of a boat.
On a boat, stay on deck and avoid the cafeteria or sitting where your can smell the engines.
Breathe fresh air
Breathe fresh air if possible. For example, open a car window.
Avoid strong smells, particularly petrol and diesel fumes. This may mean closing the window and turning on the air conditioning, or avoiding the engine area in a boat.
Use your eyes and ears differently
Close your eyes (and keep them closed for the whole journey). This reduces 'positional' signals from your eyes to your brain and reduces the confusion.
Don't try to read.
Try listening to an audio book with your eyes closed. There is some evidence that distracting your brain with audio signals can reduce your sensitivity to the motion signals.
Try to sleep - this works mainly because your eyes are closed, but it is possible that your brain is able to ignore some motion signals when you are asleep.
Do not read or watch a film.
It is advisable not to watch moving objects such as waves or other cars. Don't look at things your brain expects to stay still, like a book inside the car. Instead, look ahead, a little above the horizon, at a fixed place.
If you are the driver you are less likely to feel motion sickness. This is probably because you are constantly focused on the road ahead and attuned to the movements that you expect the vehicle to make. If you are not, or can't be, the driver, sitting in the front and watching what the driver is watching can be helpful.
Treat your tummy gently
Avoid heavy meals and do not drink alcohol before and during travelling. It may also be worth avoiding spicy or fatty food.
Try to 'tame your tummy' with sips of a cold water or a sweet, fizzy drink. Cola or ginger ale are recommended.
Try alternative treatments
Sea-Bands® are acupressure bands that you wear on your wrists to put pressure on acupressure points that Chinese medicine suggests affects motion sickness. Some people find that they are effective.
Homeopathic medicines seem to help some people, and will not make you drowsy. The usual homeopathic remedy is called 'nux vom'. Follow the instructions on the packet.
All the techniques above which aim to prevent motion sickness will also help reduce it once it has begun. Other techniques, which are useful on their own to treat motion sickness but can also be used with medicines if required, are:
Breathe deeply and slowly and, while focusing on your breathing, listening to music. This has been proved to be effective in clinical trials.
Ginger - can improve motion sickness in some people (as a biscuit or sweet, or in a drink).
There are several motion sickness medicines available which can reduce, or prevent, symptoms of motion sickness. You can buy them from pharmacies or, in some cases, get them on prescription. They work by interfering with the nerve signals described above.
Medicines are best taken before the journey. They may still help even if you take them after symptoms have begun, although once you feel sick you won't absorb medicines from the stomach very well. So, at this point, tablets that you put against your gums, or skin patches, are more likely to be effective.
Hyoscine is usually the most effective medicine for motion sickness . It is also known as scopolamine. It works by preventing the confusing nerve messages going to your brain.
There are several brands of medicines which contain hyoscine - they also come in a soluble form for children. You should take a dose 30-60 minutes before a journey; the effect can last up to 72 hours. Hyoscine comes as a patch for people aged 10 years or over. (This is only available on prescription - see below.) Side-effects of hyoscine include dry mouth , drowsiness and blurred vision.
Side-effects of motion sickness medicines
Some medicines used for motion sickness may cause drowsiness. Some people are extremely sensitive to this and may find that they are so drowsy that they can't function properly at all. For others the effects may be milder but can still impair your reactions and alertness. It is therefore advisable not to drive and not to operate heavy machinery if you have taken them. In addition, some medicines may interfere with alcohol or other medication; your doctor or the pharmacist can advise you about this.
Antihistamines
Antihistamines can also be useful , although they are not quite as effective as hyoscine. However, they usually cause fewer side-effects. Several types of antihistamine are sold for motion sickness. All can cause drowsiness, although some are more prone to cause it than others; for example, promethazine , which may be of use for young children on long journeys, particularly tends to cause drowsiness. Older children or adults may prefer one that is less likely to cause drowsiness - for example, cinnarizine or cyclizine.
Remember, if you give children medicines which cause drowsiness they can sometimes be irritable when the medicines wear off.
See the separate article called How to manage motion sickness .
There are a number of anti-sickness medicines which can only be prescribed by your doctor. Not all of them always work well for motion sickness, and finding something that works may be a case of trial and error. All of them work best taken up to an hour before your journey, and work less well if used when you already feel sick. See also the separate leaflet called Nausea (Causes, Symptoms, and Treatment) for more detailed information about these medicines .
Hyoscine patch
Hyoscine, or scopolamine, patches are suitable for adults and for children over 10 years old. The medicine is absorbed through your skin, although this method of medicine delivery is slow so the patch works best if applied well before your journey.
You should stick the patch on to the skin behind the ear 5-6 hours before travelling (often this will mean late on the previous night) and remove it at the end of the journey.
Prochlorperazine
Prochlorperazine is a prescription-only medicine which works by changing the actions of the chemicals that control the tendency to be sick (vomit), in your brain. One form of prochlorperazine is Buccastem®, which is absorbed through your gums and does not need to be swallowed. Buccastem® tastes rather bitter but it can be effective for sickness when you are already feeling sick, as it doesn't have to be absorbed by the stomach.
Metoclopramide
Metoclopramide is a tablet used to speed up the emptying of your tummy. Slow emptying of the tummy is something that happens when you develop nausea and vomiting, so metoclopramide can help prevent this. It prevents nausea and vomiting quite effectively in some people. It can occasionally have unpleasant side-effects, particularly in children (in whom it is not recommended). Metoclopramide is often helpful for those who tend to have gastric reflux, those who have slow tummy emptying because of previous surgery, and those who have type 1 diabetes. Your GP will advise whether metoclopramide is suitable for you.
Domperidone
Domperidone , like metoclopramide, is sometimes used for sickness caused by slow tummy emptying. It is not usually recommended for motion sickness but is occasionally used if other treatments don't help. Domperidone is not a legal medicine in some countries, including the USA.
Ondansetron
Ondansetron is a powerful antisickness medicine which is most commonly used for sickness caused by chemotherapy, and occasionally used for morning sickness in pregnancy. It is not usually effective for motion sickness. This, and its relatively high cost means that it is not prescribed for motion sickness alone. However, for those undergoing chemotherapy, and for those who have morning sickness aggravated by travel, ondansetron may be helpful.
If you're actually sick you may find that this relieves your symptoms a little, although not always for very long. If you've been sick:
Try a cool flannel on your forehead, try to get fresh air on your face and do your best to find a way to rinse your mouth to get rid of the taste.
Don't drink anything for ten to twenty minutes (or it may come straight back), although (very) tiny sips of very cold water, coke or ginger ale may help.
After this, go back to taking all the prevention measures above.
Once you reach your destination you may continue to feel unwell. Sleep if you can, sip cold iced water, and - when you feel ready - try some small carbohydrate snacks. Avoid watching TV (more moving objects to watch!) until you feel a little better.
The sensation called 'mal de debarquement' (French for sickness on disembarking) refers to the sensation you sometimes get after travel on a boat, train or plane, when you feel for a while as though the ground is rocking beneath your feet. It is probably caused by the overstimulation of the balance organs during your journey. It usually lasts only an hour or two, but in some people it can last for several days, particularly after a long sea journey. It does not usually require any treatment.
Persistent mal de debarquement syndrome is an uncommon condition in which these symptoms may persist for months or years.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Spinks A, Wasiak J ; Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database Syst Rev. 2011 Jun 15;(6):CD002851.
- Lackner JR ; Motion sickness: more than nausea and vomiting. Exp Brain Res. 2014 Aug;232(8):2493-510. doi: 10.1007/s00221-014-4008-8. Epub 2014 Jun 25.
- Leung AK, Hon KL ; Motion sickness: an overview. Drugs Context. 2019 Dec 13;8:2019-9-4. doi: 10.7573/dic.2019-9-4. eCollection 2019.
- Zhang LL, Wang JQ, Qi RR, et al ; Motion Sickness: Current Knowledge and Recent Advance. CNS Neurosci Ther. 2016 Jan;22(1):15-24. doi: 10.1111/cns.12468. Epub 2015 Oct 9.
- Van Ombergen A, Van Rompaey V, Maes LK, et al ; Mal de debarquement syndrome: a systematic review. J Neurol. 2016 May;263(5):843-854. doi: 10.1007/s00415-015-7962-6. Epub 2015 Nov 11.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 14 Mar 2028
16 mar 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
Steals & Deals: Up to 77% off wireless earbuds, packing cubes, more travel essentials
- TODAY Plaza
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
Best motion sickness treatments for kids in 2019

The first time your kid pukes in the car, you might be totally caught off guard. What just happened? All you were trying to do was take a little ride to see grandma and grandpa and now here you are, pulled over at a random gas station, desperately hoping that you have enough wipes, brought a change of clothes and can get the smell out.
Yes, I've experienced it.
As a mom whose kid has gotten both car and plane sick (yes, fellow passengers, your worst nightmare come true), motion sickness is nothing new. Yet every time it happens, it’s the worst.
Kids are prone to car sickness starting around two years of age, says Dr. Kevin Dahlman, a pediatrician and medical director of Aurora Children’s Health in Whitefish Bay, Wisconsin. Nausea, dizziness and vomiting can happen when the brain receives conflicting messages: “Your inner ear, which manages balance, and eyes, which perceive motion, don’t match with how you’re feeling,” he said.
When your kid is sitting in a car seat , they’re often not focused on what’s going on outside. That disconnect triggers the symptoms.
Of course, many lucky kids never experience car sickness. But, if yours do, here’s what you need to prevent car sickness, manage symptoms, and (unfortunately), clean up if it happens, according to a pediatrician.
Top motion sickness treatments
- 1. Dramamine Motion Sickness Relief for Kids, $4, Amazon
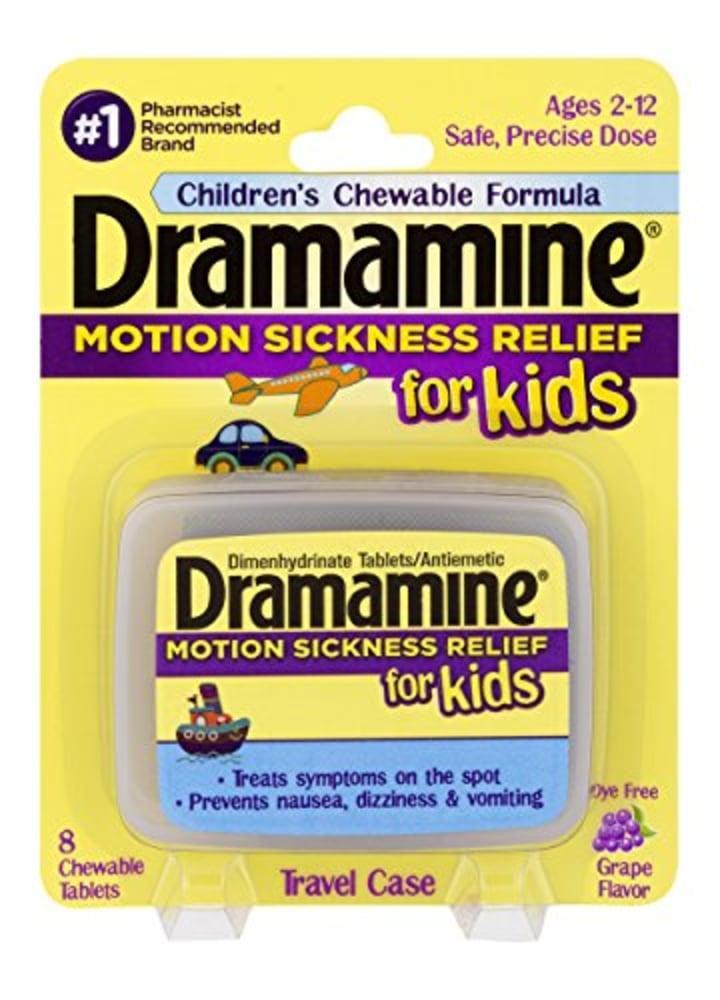
Dramamine Motion Sickness Relief for Kids
Starting at age 2, your kid can take dimenhydrinate, an antihistamine that prevents nausea and vomiting. You probably know it best as Dramamine. While you can give them the adult version (read the label; they may take a half tablet if they’re young), the benefit to the kid’s formula is that it’s a chewable, grape-flavored tablet, which can make them more likely to take it without fuss. Plus, the handy travel case makes it easy to pop in your purse.
- 2. Children’s Benadryl, $5, Amazon
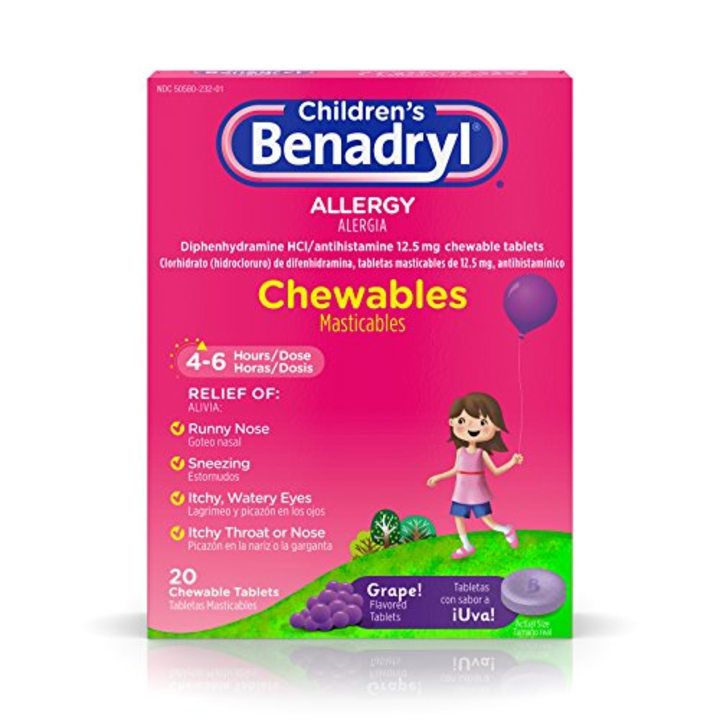
Children's Benadryl Allergy Chewables
You probably think of this antihistamine as suitable for allergies, but diphenhydramine is another option and safe for kids over the age of 2, said Dahlman. Meds are best used when you’re going to be in the car for an hour or two, he said. Have them take the medication an hour before travel. Warning: It will likely make them sleepy, which can be an added benefit — if they’re snoozing they’re not throwing up — but you also don’t want them to arrive at the destination drowsy.
- 3. The Ginger People Gin Gins Original Chewy Ginger Candy, $2, Thrive Market
The Ginger People Gin Gins Original Chewy Ginger Candy
Ginger is a natural remedy to settle an upset stomach . This ginger comes in the form of a candy, which can be a benefit when you’re trying to give it to your kid. These chews are also individually packaged, so they’re easy to grab on the go.
- 4. The Ginger People Ginger Rescue Chewable Ginger in Mighty Mango, $4, Thrive Market
The Ginger People Ginger Rescue Chewable Ginger, Mighty Mango
Another option when your kid's tummy feels off, the mango-flavored chewable doesn't taste as much of ginger.
- 5. Sea-Band Wristband, Child, $6, Amazon

Sea-Band Wristband, Child, Colors May Vary, 1 Pair, Anti-Nausea Acupressure Motion or Morning Sickness
“Some studies show acupressure bands can decrease symptoms of motion sickness, while others say there is no difference,” said Dahlman. That said, there’s no risk in trying them, and you may get good results, he added.
- 6. Travel Scavenger Hunt Card Game, $7, Amazon


Travel Scavenger Hunt Card Game
If your kid is prone to puking, Dahlman recommends that they look out the window. “When you focus on the outside, you’re better at perceiving motion, and it’s distracting, too,” he said. So, encourage a scavenger hunt game. Make it up yourself by having them pick out things they see that are “red” or “begin with the letter C,” or use a card game to help build excitement.
- 7. Regal Games Original Travel Bingo, $8, Amazon

Regal Games Original Travel Bingo 4 Pack
Getting the whole family involved can also be the distraction your kid needs to avoid nausea. (Just know where yours falls; some get sick by looking at words, while others need something to do.) This throwback game gets the whole family in on the action.
- 8. Bumkins Kids Long Sleeve Smock, $15, Amazon

Bumkins Kids Long Sleeve Smock
If you have a perennial puker on your hands, a long-sleeved “bib” is a must. (Yes, it’s horrifying that you need one, but here we are.) This art smock fits kids three to five, has a pocket at the bottom to catch anything, and is easy to remove and clean.
- 9. Disposable Barf Bags, $16, Amazon
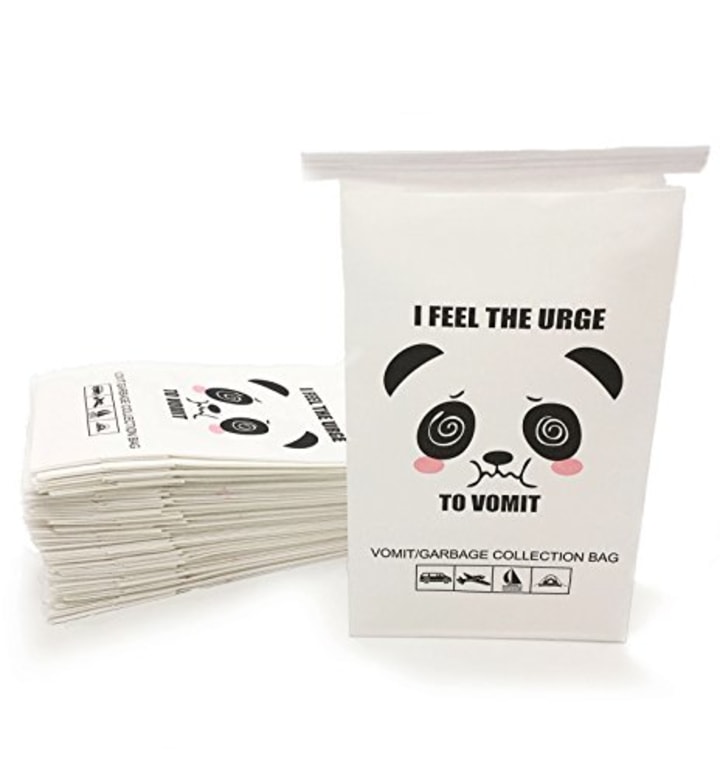
50 Pack Disposable Barf Bags
When your kid is a bit older, they can tell you when they’re not feeling great. Or, they'll show signs like cold sweats or paleness, said Dahlman. At that point, you can help them out by passing one of these back. If you’re going to carry a barf bag, might as well make it a cute and funny one.
And, before you go: one word on vomit cleanup. The post-puke smell is almost impossible to get out, and it’s tempting to try to use whatever you can to clean a car seat. However, harsh cleansers can compromise car seat material. Always read your car manufacturer’s recommendations for cleaning; often, they suggest a mild soap on the cover and recommend skipping using soap on the straps at all.
Want more parenting tips? Check out:
- The best toy to keep kids entertained on planes and in restaurants
- 10 tricks to get your baby to sleep
- The leakproof water bottle every kid needs
- Second Opinion
Why Children Get Carsick—And What to Do
Motion sickness is common, especially in children. But what causes it is only partly understood. Experts don't know why some children have it and others don’t.
The most common form of motion sickness for many children is carsickness. But getting carsick isn’t really about the car. It’s about the brain’s ability to understand a message based on what it senses. Normally, the eyes, ears, and joints all send signals to the brain. And these signals are all alike. If you’re traveling in a car, most body parts tell the brain: “We’re moving forward.”
But a child's brain gets different messages if the child is sitting too low to see through the window to the horizon. Or if the child is looking down and reading at the same time. The part of the ear that controls balance and motion says, “We’re moving.” But the message from the eyes says, “We’re sitting still and looking at a book!”
This leads to a sensory mismatch that overloads and confuses the brain. The result is upset stomach (nausea). This can be a problem when children are not looking out the windshield.
If your children are too young to express themselves, they may be carsick if they:
Become bad-tempered
Yawn frequently
Are sweaty and pale
Get restless
Here are some tips to prevent carsickness:
Stop often and at the first sign of symptoms. Before leaving home, give children some crackers or other light snack. Don't smoke or carry any strong-smelling food in the car.
Have your kids sit higher up. Elevate your children with approved child safety seats or booster seats so that they can see the horizon through the windshield. But remember, that children younger than age 2 need to be in rear-facing car seats unless they have reached the highest weight or height allowed by the car seat maker.
Entertain young children. Keep kids busy with activities that stop them from looking down. Instead of using books, try playing music for them to listen to.
If your children get carsick, stop as soon as possible. Have them lie down on their back until the dizziness stops. Put a cool cloth on their forehead. If they have vomited, offer them cold water and a light snack when the nausea passes.
If carsickness is a regular problem, talk with your healthcare provider. He or she may suggest an over-the-counter travel sickness medicine for children older than age 2. Use the correct amount based on your children’s age. Some of these medicines cause sleepiness or even agitation. Always get advice from your healthcare provider and be careful when using them. Don't use a motion sickness patch. It has too high a dosage for children.
- Find Locations
- Cleft and Craniofacial Center
- Pediatric Cardiology
Related Topics
Health Tip: Dealing With Motion Sickness
Dimenhydrinate chewable tablets
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH
Schedule an appointment today

- Babies & Children
- Bones, Joints & Muscles
- Brain & Nerves
- Diet & Nutrition
- Ear, Nose & Throat
- Eyes & Vision
- Family Medicine
- Heart & Vascular
- Integrative Medicine
- Lungs & Breathing
- Men’s Health
- Mental Health
- Neurology & Neurosurgery
- Older Adults & Aging
- Orthopedics
- Skin, Hair & Nails
- Spine & Back
- Sports Medicine & Exercise
- Travel Medicine
- Urinary & Kidney
- Weight Loss & Management
- Women's Health
- Patient Stories
- Infographics
How to Prevent and Treat Car Sickness in Kids
January 30, 2023

Car sickness is a common problem in young children—but don’t blame it on the car. It’s actually a form of motion sickness, a broader condition in which movement brings on symptoms such as dizziness and nausea. This problem may occur not only in cars, but also on boats, planes, trains and amusement park rides.
Why do some little ones feel sick more easily than others? Douglas Hackenberg, MD at University Hospitals Rainbow Children’s Medical Group, explains that the issue may be due to increased sensitivity in part of the inner ear that plays a key role in balance, as well as the brain receiving signals from eye, ears and other sensations.
Taking Preventive Steps
“Young children ages 2 to 12 are especially prone to motion sickness,” says Dr. Hackenberg. “If it isn’t managed, it can make traveling stressful for everyone. But by planning ahead, you can usually keep it in check”. He suggests trying these tips:
- Use anti-motion sickness medicine. Dimenhydrinate (such as Dramamine) is sold in chewable tablets for kids ages 2 and older. It’s available without a prescription. This medicine should be given an hour before traveling, and one dose helps prevent symptoms for about six hours.
- Consider child-sized acupressure wristband s (such as Sea-Bands) for additional help. Putting a band around each of your child’s wrists before beginning your trip may help relieve nausea by stimulating pressure points.
- Bring the right entertainment along. Looking at a book or device screen may trigger symptoms. Listening to music or an audio story is a better option.
- Focusing on objects outside of the car. Sometimes fresh air and focusing attention outside of the vehicle can provide enough additional information to the brain to ease the cycle of motion sickness.
Caring for Motion Sickness
Many people associate motion sickness with throwing up. But in children younger than age 6, the main symptoms are dizziness and wanting to lie down. Other potential symptoms include unsteady walking, nausea and vomiting.
If symptoms of motion sickness have already begun, offer only sips of water until your child’s tummy settles down. Keep a vomit pan or bag handy, just in case. Encourage rest – your little one may even doze off.
“The good news is that motion sickness usually goes away within four hours after the motion stops,” says Dr. Hackenberg. “If the symptoms last for more than eight hours however, you should call your child’s pediatrician for advice.”
If your child feels dizzy or unsteady, and it doesn’t seem linked to movement, talk with your child’s pediatrician. This may be a sign of something else, such as vertigo (an abnormal spinning sensation) or other issues with the body’s balance system.
Related Links
University Hospitals Rainbow Babies & Children’s has the region’s largest coordinated network of pediatric primary care providers, committed to delivering the very best care to children of all ages, including routine immunizations. Find a UH Rainbow pediatric practice near you.
Tags: Donald Hackenberg MD FAAP , Motion sickness
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Motion sickness
Help your child avoid motion sickness in the car by breathing fresh air, looking at a spot on the horizon, and maybe eating a little snack before you go. If you're in a plane, train, or boat, have her face forward.

Why does my child get sick when riding in the car?
What causes motion sickness, what can i do to help my child's motion sickness, are there drugs my child can take before a long trip to prevent motion sickness.
It sounds like your child has motion sickness. It's most common in children ages 2 to 12 years old, but it can happen at any age. Some kids are more prone to motion sickness than others – maybe because they're more sensitive to the brain's response to motion.
Motion sickness can also strike during a boat, train, or plane ride, especially if it's your child's first time or the motion is dramatic (turbulent air or rough water). It can even be triggered by swinging on a swing .
The good news is that the tendency to get carsick, get seasick, and feel motion sickness usually diminishes as kids get older.
The problem happens when your child's brain receives different messages from the parts of her body that sense motion – like the eyes, inner ears, nerves, and joints.
For example, if she's looking at a toy or a picture book in a moving car, her eyes are sending a signal to her brain that she's not in motion. But other parts of her body can feel that she's in motion, so they send the opposite message. These conflicting signals cause her to feel nauseated.
The same thing can happen on a plane during turbulence or in a boat riding the ocean swells. Stress and excitement can make the symptoms worse, too.
Be patient with your child, who is feeling quite miserable, and try these tips:
- Be alert to the early signs of motion sickness – a cold sweat and loss of appetite typically show up before a child starts vomiting – and stop the activity if possible. For example, pull off the road for a short break if you're driving. If you can stop, lay him down and place a cool cloth on his forehead. His symptoms will likely subside within 15 minutes or so.
- If your child is old enough to face forward in the car , have him look ahead at a spot on the horizon. An object in the distance will give visual input that you're moving relative to that point. This will help resolve some of the mixed messages being sent to his brain.
- Provide some cool air. In the car, set the fan or air conditioner to blow lightly on your child or crack the window for a breeze. On a boat, take him out on deck.
- For a smoother ride in a large car with two rows of backseats, secure him in the middle row rather than the rearmost row (and for safety's sake, never in the front). In other forms of transportation, choose the forward cars of a train; the upper deck of a boat, toward the middle; and by the front edge of the wings of a plane. Position him where he can look out the window whenever possible.
- Distract him. Motion sickness can sometimes be a state of mind, so try singing or chatting. Don't have him look at books or play with toys, though, because these will make him more disoriented.
- Feed your child. Your instinct may tell you to do the opposite, but provide a light snack before the trip. Why? Hunger can sometimes make nausea worse. (There's some debate on this one, so note whether eating a little snack helps or hinders your child's trip. Then you'll know how to prepare next time.)
- Try to schedule the trip during naptime, because he's much less likely to become sick to his stomach if he's asleep during the motion. If he's beyond napping age, encourage him to sleep if he's tired.
- Keep activity to a minimum. Try to keep your child as calm as you can, with his head as motionless as possible.
- You might also try a motion-sickness bracelet, which is thought to quell nausea by stimulating acupressure points on the wrist. While the scientific evidence supporting its effectiveness is still lacking, some families report relief. And if you tell your child that this special bracelet is made to keep him from feeling sick in the car or on the plane – well, it just might do the trick. (Be sure to check the label to make sure the band is appropriate for your child's age.)
If your child ends up vomiting despite your best efforts, have him drink liquids to avoid dehydration .
For children 2 years old and up, anti-nausea medications are sold over the counter, some in chewable tablet and liquid forms. But ask the doctor before giving one to your child. Side effects can include drowsiness or excitability, dry mouth, constipation, and blurred vision.
For insurance on trips, take along a durable plastic bag, wipes or a damp cloth, and a change of clothes.
Learn more:
- Family car trips: Easy ways to keep kids happy and entertained
- How to enjoy a plane trip with children
- Tips for traveling with babies and toddlers
- Planning a family trip
Was this article helpful?
Parents say: How to soothe your child when she has an owie

Test your health IQ: What's the best way to make the medicine go down?

Best toddler tablets

How should I react when my child hears someone make a racist remark? (ages 6 to 8)

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
AAP. 2015. Car sickness. American Academy of Pediatrics. https://www.healthychildren.org/English/health-issues/conditions/head-neck-nervous-system/Pages/Car-Sickness.aspx Opens a new window [Accessed August 2020]
Erskine S. 2019. Motion sickness. U.S. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-by-air-land-sea/motion-sickness Opens a new window [Accessed August 2020]
Mayo Clinic. 2018. What causes car sickness in children and how can I prevent it? https://www.mayoclinic.org/healthy-lifestyle/childrens-health/expert-answers/car-sickness-in-children/faq-20057876 Opens a new window [Accessed August 2020]
Mayo Clinic. 2017. Motion sickness: First aid. https://www.mayoclinic.org/first-aid/first-aid-motion-sickness/basics/ART-20056697 Opens a new window [Accessed August 2020]
MedlinePlus. 2020. Motion sickness. https://medlineplus.gov/motionsickness.html Opens a new window [Accessed August 2020]

Where to go next

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Travel With Medication Needed for a Sick Child
When traveling with medication for a sick child, be aware of these potentially complicating factors
- Travel Tips
- Medical Kits
- Who Shouldn't Fly
- Can Airlines Refuse?
Traveling with a sick child is often manageable with the right preparations. But if your child has or is suspected to have a serious contagious illness, like whooping cough or COVID-19, or poses a health risk to others, you will need to delay your trip until your child's condition is stabilized.
Many world destinations prohibit medications, like Adderall , that are commonly used by children in the United States. Certain medications, like insulin pens and epipens, usually need to be declared, since needles are prohibited on planes. Before you leave, research your destination carefully to ensure you are compliant.
This article explains what medicines you can and cannot take when traveling. It also provides a handful of tips for navigating airports and country-specific regulations.
Tips for Traveling With a Sick Child
Whether you are traveling by land, sea, or plane, the key to navigating travel with a sick child is getting (and staying) organized.
It's a good idea to keep all medications and supplies in a separate, clear "medical kit," so that they are easy to find and can be quickly retrieved when you need them.
The following tips and Transportation Security Administration (TSA) recommendations can help you organize your medical kit and prepare for your journey with a sick child.
Organizing Medications
Although medications can be packed in checked or carry-on luggage, it's best to bring them in your carry-on. That way, they will be available if you need them on the plane or in the airport.
While organizing your medical kit, consider including:
- Solid medications (such as pills or oral powders), which are permitted in carry-on or checked luggage in unlimited quantities, but will need to be Xd-rayed at the security checkpoint
- Extra medications in case your trip is extended or your medications get lost
TSA does not require passengers to bring medications in prescription bottles, so you can bring them in a pill organizer if you like. Laws vary between states and countries regarding prescription labeling, though. Check with the embassy at your destination to learn the respective laws.
Preparing Liquids and Other Types of Medications
Liquid medications are allowed in carry-on or checked bags, but you will need to follow a few regulations when flying with them:
- Medically necessary liquid medications can be brought in your carry-on or checked luggage in reasonable quantities. Tell an officer that you have a medically necessary liquid before starting the screening process. You may be asked to open the liquid medication for additional screening.
- Insulin is allowed in carry-on or checked luggage in reasonable quantities. At the security checkpoint, place insulin in a separate bin for X-ray screening.
- Nebulizers are allowed in carry-on bags but must be removed from the carrying case and X-rayed at the security checkpoint. Liquids associated with nebulizers are permitted in reasonable quantities.
As for injectables, inhalers, pumps, and aerosols:
- EpiPens can be packed in carry-on or checked luggage in reasonable quantities but must be declared to TSA officers at the security checkpoint for inspections.
- Insulin pumps are permitted in carry-on or checked luggage but must be accompanied by insulin. Tell TSA officers if you have diabetes and are wearing an insulin pump at the start of security screening.
- Medically necessary aerosols , such as metered-dose inhalers , are allowed in carry-on or checked bags in reasonable quantities but must be presented to TSA officers at the security checkpoint.
- Glucose monitors with metal or lithium batteries should be carried in carry-on luggage and should be presented to TSA officers at the security checkpoint.
- Inhalers are permitted in carry-on or checked luggage in reasonable quantities but will need to be X-rayed at the security checkpoint.
Federal regulations prohibit passengers from bringing their own supplemental oxygen onto airplanes. If you or your child require supplemental oxygen, you will need to call the airline at least 72 hours before your flight to arrange in-flight supplemental oxygen.
If you do not want a medical item to be X-rayed, you may request a visual inspection instead. Make this request before sending your items through the X-ray tunnel.
Not Sure if You Can Bring It?
Use the TSA "What Can I Bring?" website to find specific instructions related to most medications and medical supplies. This website provides instructions for external medical devices (such as feeding tubes), mercury thermometers, personal oxygen, syringes, and more.
Readying a "Back-Up" Plan
Plan where you will go for medical attention if needed. Write important numbers and addresses down and keep them in your medical kit.
Is there a children's hospital, pediatrician, or clinic where you are staying or on your travel route? This is especially important for international travelers and when you are on a cruise.
Even facilities that promote family travel and provide licensed healthcare providers for sick travelers are not guaranteed to have a pediatrician available in case of severe illness.
The nearest children's hospital or local medical society may be able to help you find a pediatrician if you are traveling and your child gets sick.
When traveling in another country, an international clinic , your travel agency, the U.S. Embassy, or the U.S. Consulate may be able to help you locate a pediatrician.
If your child has a chronic medical problem, consider acquiring a medical alert bracelet for them to wear, just in case they get sick and you aren't around. This is especially important if your child has severe allergies, diabetes, seizures, or another condition that may require sudden and specific medical care.
Informing Your Healthcare Provider
Before leaving, schedule a checkup with a pediatrician and/or pediatric specialist to ensure your child's medical problems are stable.
Be transparent about your plans with the healthcare provider—they may be able to offer you some travel tips that are specific to your child's condition.
Depending on your destination, certain vaccinations may be recommended for you and/or your child to protect from disease. The CDC provides detailed information about recommended vaccines for every country in the world.
If you are traveling internationally, take some time to review the country-specific recommendations, and make a list of any vaccines your child does not have. It may help to bring this list to your provider's office in case you have questions.
Contacting Your Pharmacist for Refills
If you lose a prescription while traveling internationally, contact your healthcare provider and explain your situation. Your provider may be able to write you a new prescription that you can bring to a pharmacy near you. You can also visit a local urgent care to see if they can help.
If you are traveling within the United States, you can:
- Find a nearby pharmacy that is in-network with your insurance provider.
- Call or visit the pharmacy and explain your situation.
- Call your home pharmacy and ask them to transfer your medication to your pharmacy of choice.
In the past, in order to have your prescription transferred, you would need to contact your healthcare provider and ask them to cancel the prescription then re-submit it to a new pharmacy. According to regulations updated in 2023, however, all you need to do is contact your home pharmacy directly and ask them to initiate the switch.
There is one important caveat to the updated regulations. Prescriptions may only be transferred between pharmacies once . So, if you want to transfer a prescription back to your original pharmacy after your trip, you will need to have it canceled and re-submitted by your healthcare provider.
Complying with Laws and Regulations
Different states and countries have different laws regarding the types and quantities of medications that travelers are permitted to bring.
For example, France permits travelers to only bring the amount of medication needed for the duration of the trip. And, if the medication is a narcotic , a written letter to customs providing the name and dosage of the medication is required.
Meanwhile, countries like Japan, Singapore, and much of Europe have banned Adderall, Ritalin, and a number of other medications that are common in the United States.
Bringing controlled drugs into a foreign country can come with steep consequences, from local fines, to jail time and deportation. In Singapore, having as little as three grams of morphine can result in the death penalty.
TSA advises international travelers to prepare "requisite medical documentation" from their prescribing physician at least two months before departure. The documentation should include:
- The prescribing physician's contact information and/or credentials
- The diagnosis and treatment
- The medication regimen, including any need for needles or syringes
Additionally, the name on the prescription, container, and traveler's passport must match.
If a medication contains narcotics, you may need to submit an application to the country's Narcotics Control Division or Food and Drug Administration for permission prior to entry.
For psychotropic medications , including antidepressants, you may need to notify the medical officer at the embassy in your home country. Do this well in advance so that all appropriate parties are aware before you arrive at customs.
What Else Should Go in a Medical Kit?
Your medical kit should contain everything you need to manage your child's health condition, as well as other medical items your child may only need on occasion.
Things to include in a travel medicine kit might include:
- A pain and fever reducer, such as ibuprofen and/or acetaminophen
- A steroid cream for itching
- An antihistamine for hives and other allergic reactions
- A cough and cold medicine for older children
- An antibiotic ointment (in a container of 3.4 ounces or less—unless medically necessary)
- A regular first aid kit
Keep in mind that if you are bringing an aerosol medication in your carry-on, it must be medically necessary. Aerosol insecticides, for example, are permitted in checked luggage only.
Is My Child Too Sick to Fly?
Do not fly if you or your child has a contagious disease that poses a serious threat to other people, such as:
- Tuberculosis
- Rubella (German measles)
- Whooping cough (pertussis)
- Meningococcal disease (meningitis)
- Severe flu or another respiratory illness
If you or your child has a history of the following conditions, see your healthcare provider for an evaluation before you travel to ensure the condition is stable:
- Cardiovascular disease
- Lung disease
- Mental illness
- Recent surgery
- Deep vein thrombosis or pulmonary embolism
- Sickle cell disease
Travel is rarely contraindicated (advised against) during a normal pregnancy. However, it's best to delay travel if your pregnancy requires close medical supervision. Reasons not to travel when pregnant include:
- You are in active or premature labor
- You have a suspected ectopic pregnancy
- You have vaginal bleeding
- You have a history of preeclampsia
Cabin air pressure changes can lead to barotrauma , recognizable by pain in the ear during take-off. Although barotrauma is rarely dangerous, it can lead to dizziness, hearing loss, or permanent tinnitus. To reduce these risks, consult with a healthcare provide before travel if your child has:
- An ear, nose, or sinus infection
- Severe congestion
- Had recent ear, nose, throat, or abdominal surgery
Will the Airline Refuse My Sick Child?
You or your child may be denied boarding if you have or are suspected to have a serious contagious illness that poses a public health threat.
Airline officials will suspect contagious illness if you or your child has one or more of the following symptoms:
- Difficulty breathing
- Persistent cough
- Decreased consciousness
- Sudden confusion
- Unexplained bruising or bleeding
- Persistent diarrhea
- Persistent vomiting
- Headache with stiff neck
- Appearing obviously unwell
- Symptoms of other contagious diseases
Less than 1% of passengers are denied boarding in the United States each year. Nonetheless, airline officials are permitted to deny boarding or remove any person from a flight who appears obviously sick, or who is believed to pose a health threat to others.
Inform the airport security screener if your child has any special needs for going through security, or if they might get upset during the security procedures because of their medical condition.
Before you travel with a sick child, give yourself plenty of time to organize a medical bag with daily medications, medical supplies, and any other extras your child may need. Most medications are permitted in carry-on or checked luggage. However, if you plan to fly with a medication that is liquid, aerosol, or involves needles, you will need to declare it to TSA officers at the security checkpoint.
Depending on your destination, you may need to prepare medical documentation, especially if you need to travel with a narcotic or psychotropic drug. There can be steep consequences for bringing controlled substances into another country, so don't take chances. If you have questions about traveling with your medications, contact a physician or use resources provided by TSA to learn more.
Centers for Disease Control and Prevention. Air travel .
Harvard Global Support Services. Tips for traveling with medication .
American Diabetes Association. What can I bring with me on the plane .
Transportation Security Administration. Can you pack your meds in a pill case and more questions answered .
Transportation Security Administration. What can I bring? .
Transportation Security Administration. Insulin .
United States Drug Enforcement Administration. Revised regulation allows DEA-registered pharmacies to transfer electronic prescriptions at a patient's request .
France in the United States. Information for private individuals - Medicine .
Transportation Security Administration. Traveling with medication .
Centers for Disease Control and Prevention. Protecting travelers' health from airport to community: Investigating contagious diseases on flights .
Centers for Disease Control and Prevention. Pregnant travelers .
Centers for Disease Control and Prevention. Preventing spread of disease on commercial aircraft: Guidance for cabin crew .
GAO. Airline consumer protections .
U.S. Department of Transportation. Bumping & oversales .
By Vincent Iannelli, MD Vincent Iannelli, MD, is a board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Iannelli has cared for children for more than 20 years.
Travel-Ease
Generic name: meclizine [ MEK-li-zeen ] Brand names: Antivert , Bonine , Bonine Max, Dramamine Less Drowsy , Dramamine Nausea Long Lasting, Travel-Ease Drug class: Anticholinergic antiemetics
Medically reviewed by Drugs.com on Aug 29, 2023. Written by Cerner Multum .
What is Travel-Ease?
Travel-Ease is used in adults and children aged 12 years and older to treat or prevent nausea , vomiting and dizziness caused by motion sickness .
Travel-Ease is also used in adults to treat symptoms of vertigo (dizziness or spinning sensation) caused by disease that affects your inner ear.
Travel-Ease may also be used for purposes not listed in this medication guide.
Travel-Ease side effects
Get emergency medical help if you have signs of an allergic reaction : hives, difficult breathing, swelling of your face, lips, tongue, or throat.
Common side effects of Travel-Ease may include:
drowsiness ;
dry mouth ;
vomiting; or
feeling tired.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Use only as directed. Tell your doctor if you use other medicines or have other medical conditions or allergies.
Before taking this medicine
You should not use Travel-Ease if you are allergic to it.
Do not give Travel-Ease to anyone younger than 12 years old without medical advice.
Tell your doctor if you have or have ever had:
breathing problems such as asthma , emphysema , or chronic bronchitis ;
an enlarged prostate or urination problems;
recently used alcohol, sedatives, or tranquilizers; or
liver or kidney disease.
Tell your doctor if you are pregnant or breastfeeding.
How should I take Travel-Ease?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Use the medicine exactly as directed.
Swallow the tablet whole and do not crush, chew, or break it.
You must chew the chewable tablet before you swallow it.
To prevent motion sickness, take Travel-Ease about 1 hour before you travel or anticipate having motion sickness. You may take this medicine once every 24 hours while you are traveling, to further prevent motion sickness.
To treat vertigo, you may need to take Travel-Ease several times daily. Follow your doctor's instructions.
Store at room temperature away from moisture, heat, and light.
What happens if I miss a dose?
Travel-Ease is used when needed. If you are on a dosing schedule, skip any missed dose. Do not use two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking Travel-Ease?
Avoid driving or hazardous activity until you know how Travel-Ease will affect you. Your reactions could be impaired.
Avoid drinking alcohol. Drinking alcohol with this medicine can cause side effects.
What other drugs will affect Travel-Ease?
Using Travel-Ease with other drugs that make you drowsy can worsen this effect. Ask your doctor before using opioid medication, a sleeping pill, a muscle relaxer, or medicine for anxiety or seizures .
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which may increase side effects or make the medicines less effective.
Other drugs may affect Travel-Ease, including prescription and over-the-counter medicines, vitamins , and herbal products . Tell your doctor about all other medicines you use.
More about Travel-Ease (meclizine)
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic antiemetics
- Breastfeeding
- En español
Patient resources
Other brands.
Antivert , Bonine , Dramamine Less Drowsy , Meclicot , ... +3 more
Professional resources
- Meclizine monograph
- Meclizine (FDA)
Related treatment guides
- Motion Sickness
- Nausea/Vomiting
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
Copyright 1996-2024 Cerner Multum, Inc. Version: 8.01.
ondansetron , hydroxyzine , lorazepam , olanzapine , dexamethasone , promethazine , diphenhydramine , meclizine , Benadryl , prochlorperazine
Who can and cannot take hyoscine hydrobromide - Brand names: Kwells, Joy-Rides, Kwells Kids, Travel Calm, Scopoderm
Who can take hyoscine hydrobromide.
Hyoscine hydrobromide travel sickness tablets can be taken by most adults and children from the age of 3 years.
Patches for travel sickness can be used by most adults and children from the age of 10 years.
Who may not be able to take hyoscine hydrobromide
Hyoscine hydrobromide is not suitable for some people. To make sure it's safe for you, tell a pharmacist or doctor before taking it if you:
- have ever had an allergic reaction to hyoscine hydrobromide or any other medicine
- have an eye problem called primary angle closure glaucoma
- have difficulty peeing or a bowel blockage
- have myasthenia gravis , a condition that causes muscle weakness
- have heart problems, including a very fast heart rate
- have thyroid, kidney or liver problems
- have epilepsy (seizures)
- have digestive problems, such as acid reflux or severe constipation
- have ulcerative colitis
- have a high temperature
- are pregnant or trying to get pregnant, as hyoscine hydrobromide is not recommended in pregnancy
Page last reviewed: 5 October 2022 Next review due: 5 October 2025
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 5 - Rubella
- Section 5 - Smallpox & Other Orthopoxvirus-Associated Infections
Rubeola / Measles
Cdc yellow book 2024.
Author(s): Paul Gastañaduy, James Goodson
Infectious Agent
Transmission, epidemiology, clinical presentation.
INFECTIOUS AGENT: Measles virus
TRAVELER CATEGORIES AT GREATEST RISK FOR EXPOSURE & INFECTION
PREVENTION METHODS
Rubeola is a vaccine-preventable disease
DIAGNOSTIC SUPPORT
Measles virus is a member of the genus Morbillivirus of the family Paramyxoviridae .
Measles is transmitted from person to person via respiratory droplets and by the airborne route as aerosolized droplet nuclei. Infected people are usually contagious from 4 days before until 4 days after rash onset. Measles is among the most contagious viral diseases known; secondary attack rates are ≥90% among susceptible household and institutional contacts. Humans are the only natural host for sustaining measles virus transmission, which makes global eradication of measles feasible.
Measles was declared eliminated (defined as the absence of endemic measles virus transmission in a defined geographic area for ≥12 months in the presence of a well-performing surveillance system) from the United States in 2000. Measles virus continues to be imported into the country from other parts of the world, however, and recent prolonged outbreaks in the United States resulting from measles virus importations highlight the challenges faced in maintaining measles elimination.
Given the large global measles burden and high communicability of the disease, travelers could be exposed to the virus in any country they visit where measles remains endemic or where large outbreaks are occurring. Most measles cases imported into the United States occur in unvaccinated US residents who become infected while traveling abroad, often to the World Health Organization (WHO)–defined Western Pacific and European regions. These travelers become symptomatic after returning to the United States and sometimes infect others in their communities, causing outbreaks.
Nearly 90% of imported measles cases are considered preventable by vaccination (i.e., the travelers lacked recommended age- and travel-appropriate vaccination). Furthermore, observational studies in travel clinics in the United States have shown that 59% of pediatric and 53% of adult travelers eligible for measles-mumps-rubella (MMR) vaccine at the time of pretravel consultation were not vaccinated at the visit, highlighting a missed opportunity to reduce the likelihood of measles introductions and subsequent spread. Encourage all eligible travelers to receive appropriate MMR vaccination. Outbreak investigations are costly and resource intensive, and infected people—in addition to productivity losses—can incur direct costs for the management of their illness, including treatment, quarantine, and caregiving.
The incubation period averages 11–12 days from exposure to onset of prodrome; rash usually appears ≈14 days after exposure. Symptoms include fever, with temperature ≤105°F (≤40.6°C); conjunctivitis; coryza (runny nose); cough; and small spots with white or bluish-white centers on an erythematous base appearing on the buccal mucosa (Koplik spots). A characteristic red, blotchy (maculopapular) rash appears 3–7 days after onset of prodromal symptoms. The rash begins on the face, becomes generalized, and lasts 4–7 days.
Common measles complications include diarrhea (8%), middle ear infection (7%–9%), and pneumonia (1%–6%). Encephalitis, which can result in permanent brain damage, occurs in ≈1 per 1,000–2,000 cases of measles. The risk for serious complications or death is highest for children aged ≤5 years, adults aged ≥20 years, and in populations with poor nutritional status or that lack access to health care.
Subacute sclerosing panencephalitis (SSPE) is a progressive neurologic disorder caused by measles virus that usually presents 5–10 years after recovery from the initial primary measles virus infection. SSPE manifests as mental and motor deterioration, which can progress to coma and death. SSPE occurs in ≈1 of every 5,000 reported measles cases; rates are higher among children <5 years of age.
Measles is a nationally notifiable disease. Laboratory criteria for diagnosis include a positive serologic test for measles-specific IgM, IgG seroconversion, or a significant rise in measles IgG level by any standard serologic assay; isolation of measles virus; or detection of measles virus RNA by reverse transcription PCR (RT-PCR) testing. The Centers for Disease Control and Prevention’s Measles Virus Laboratory is the national reference laboratory; it provides serologic and molecular testing for measles and technical assistance to state public health laboratories for the collection and shipment of clinical samples for molecular diagnostics and genetic analysis. See detailed information on diagnostic support .
A clinical case of measles illness is characterized by generalized maculopapular rash lasting ≥3 days; temperature ≥101°F (38.3°C); and cough, coryza, or conjunctivitis. A confirmed case is one with an acute febrile rash illness with laboratory confirmation or direct epidemiologic linkage to a laboratory-confirmed case. In a laboratory-confirmed or epidemiologically linked case, the patient’s temperature does not need to reach ≥101°F (38.3°C) and the rash does not need to last ≥3 days.
Treatment is supportive. The WHO recommends vitamin A for all children with acute measles, regardless of their country of residence, to reduce the risk for complications. Administer vitamin A as follows: for infants <6 months old, give 50,000 IU, once a day for 2 days; for infants 6 months old and older, but younger than 12 months, give 100,000 IU once a day for 2 days; for children ≥12 months old give 200,000 IU once a day for 2 days. For children with clinical signs and symptoms of vitamin A deficiency, administer an additional (i.e., a third) age-specific dose of vitamin A 2–4 weeks following the first round of dosing.
Measles has been preventable through vaccination since a vaccine was licensed in 1963. People who do not have evidence of measles immunity should be considered at risk for measles, particularly during international travel. Acceptable presumptive evidence of immunity to measles includes birth before 1957; laboratory confirmation of disease; laboratory evidence of immunity; or written documentation of age-appropriate vaccination with a licensed, live attenuated measles-containing vaccine 1 , namely, MMR or measles-mumps-rubella-varicella (MMRV). For infants 6 months old and older, but younger than 12 months, this includes documented administration of 1 dose of MMR; for people aged ≥12 months, documentation should include 2 doses of MMR or MMRV (the first dose administered at age ≥12 months and the second dose administered no earlier than 28 days after the first dose). Verbal or self-reported history of vaccination is not considered valid presumptive evidence of immunity.
1 From 1963–1967, a formalin-inactivated measles vaccine was available in the United States and was administered to ≈600,000–900,000 people. It was discontinued when it became apparent that the immunity it produced was short-lived. Consider people who received this vaccine unvaccinated.
Vaccination
Measles vaccine contains live, attenuated measles virus, which in the United States is available only in combination formulations (e.g., MMR and MMRV vaccines). MMRV vaccine is licensed for children aged 12 months–12 years and can be used in place of MMR vaccine if vaccination for measles, mumps, rubella, and varicella is needed.
International travelers, including people traveling to high-income countries, who do not have presumptive evidence of measles immunity and who have no contraindications to MMR or MMRV, should receive MMR or MMRV before travel per the following schedule.
Infants (6 months old and older, but younger than 12 months): 1 MMR dose. Infants vaccinated before age 12 months must be revaccinated on or after the first birthday with 2 doses of MMR or MMRV separated by ≥28 days. MMRV is not licensed for children aged <12 months.
Children (aged ≥12 months): 2 doses of MMR or MMRV separated by ≥28 days.
Adults born in or after 1957: 2 doses of MMR separated by ≥28 days.
One dose of MMR is ≈85% effective when administered at age 9 months; MMR and MMRV are 93% effective when administered at age ≥1 year. Vaccine effectiveness of 2 doses is 97%.
Adverse Reactions
In rare circumstances, MMR vaccination has been associated with anaphylaxis (≈2–14 occurrences per million doses administered); febrile seizures (≈1 occurrence per 3,000–4,000 doses administered, but overall, the rate of febrile seizures after measles-containing vaccine is much lower than the rate with measles disease); thrombocytopenia (≈1 occurrence per 40,000 doses during the 6 weeks after immunization); or joint symptoms (arthralgia develops among ≈25% of nonimmune postpubertal females from the rubella component of the MMR vaccination, and ≈10% have acute arthritis-like signs and symptoms that generally persist for 1–21 days and rarely recur; chronic joint symptoms are rare, if they occur at all). No evidence supports a causal link between MMR vaccination and autism, type 1 diabetes mellitus, or inflammatory bowel disease.
Contraindications
People who experienced a severe allergic reaction (difficulty breathing, hives, hypotension, shock, swelling of the mouth or throat) following a prior dose of MMR or MMRV vaccine, or who had an anaphylactic reaction to topically or systemically administered neomycin, should not be vaccinated or revaccinated. People who are allergic to eggs can receive MMR or MMRV vaccine without prior routine skin testing or the use of special protocols.
Immunosuppression
Enhanced replication of live vaccine viruses can occur in people who have immune deficiency disorders. Death related to vaccine-associated measles virus infection has been reported among severely immunocompromised people; thus, severely immunosuppressed people should not be vaccinated with MMR or MMRV vaccine. For a thorough discussion of recommendations for immunocompromised travelers, see Sec. 3, Ch. 1, Immunocompromised Travelers .
MMR vaccination is recommended for all people with HIV infection aged ≥12 months who do not have evidence of measles, mumps, and rubella immunity, and who do not have evidence of severe immunosuppression. The assessment of severe immunosuppression can be based on CD4 values (count or percentage); absence of severe immunosuppression is defined as CD4 ≥15% for ≥6 months for children aged ≤5 years, or CD4 ≥15% and CD4 count ≥200 cells/mL for ≥6 months for people aged >5 years.
People with leukemia in remission and off chemotherapy, who were not immune to measles when diagnosed with leukemia, may receive MMR vaccine. At least 3 months should elapse after termination of chemotherapy before administering the first dose of vaccine.
Steroids & Other Immunosuppressive Therapies
Avoid vaccinating people who have received high-dose corticosteroid therapy (in general, considered to be ≥20 mg or 2 mg/kg body weight of prednisone, or its equivalent, daily for ≥14 days) with MMR or MMRV for ≥1 month after cessation of steroid therapy. Corticosteroid therapy usually is not a contraindication when administration is short-term (<14 days) or a low to moderate dose (<20 mg of prednisone or equivalent per day).
In general, withhold MMR or MMRV vaccine for ≥3 months after cessation of other immunosuppressive therapies and remission of the underlying disease. See Sec. 3, Ch. 1, Immunocompromised Travelers , for more details.
MMR vaccines should not be administered to pregnant people or people attempting to become pregnant. Because of the theoretical risk to the fetus, people should be counseled to avoid becoming pregnant for 28 days after receiving a live-virus (e.g., MMR) vaccine.
Precautions
Personal or family history of seizures of any etiology.
Compared with administration of separate MMR and varicella vaccines at the same visit, use of MMRV vaccine is associated with a higher risk for fever and febrile seizures 5–12 days after the first dose among children aged 12–23 months. Approximately 1 additional febrile seizure occurs for every 2,300–2,600 MMRV vaccine doses administered. Use of separate MMR and varicella vaccines avoids this increased risk for fever and febrile seizures.
Thrombocytopenia
The benefits of primary immunization are usually greater than the potential risks for vaccine- associated thrombocytopenia. Avoid giving subsequent doses of MMR or MMRV vaccine, however, if an episode of thrombocytopenia occurred ≤6 weeks after a previous dose of vaccine.
Postexposure Prophylaxis
Measles-containing vaccine or immune globulin (IG) can be effective as postexposure prophylaxis. MMR or MMRV administered ≤72 hours after initial exposure to measles virus might provide some protection. If the exposure does not result in infection, the vaccine should induce protection against subsequent measles virus infection.
When administered ≤6 days of exposure, IG can be used to confer temporary immunity in a susceptible person. If the exposure does not result in modified or typical measles, vaccination with MMR or MMRV is still necessary to provide long-lasting protection. Six months after receiving intramuscularly administered IG, or 8 months after receiving intravenously administered IG, administer MMR or MMRV vaccine, provided the patient is aged ≥12 months and the vaccine is not otherwise contraindicated.
CDC website: Measles
The following authors contributed to the previous version of this chapter: Paul A. Gastañaduy, James L. Goodson
Bibliography
Centers for Disease Control and Prevention. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR-04):1–34.
Gastañaduy P, Redd S, Clemmons N, Lee AD, Hickman CJ, Rota PA, et al. Measles. In: Roush SW, Baldy LM, Kirkconnell Hall MA, editors. Manual for the surveillance of vaccine-preventable diseases. Atlanta: Centers for Disease Control and Prevention; 2019. Available from: www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html .
Hyle EP, Fields NF, Fiebelkorn AP, Taylor Walker A, Gastañaduy P, Rao SR, et al. The clinical impact and cost-effectiveness of measles-mumps-rubella vaccination to prevent measles importations among US international travelers. Clin Infect Dis. 2019;69(2):306–15.
Hyle EP, Rao SR, Bangs AC, Gastañaduy P, Parker Fiebelkorn A, Hagmann SHF, et al. Clinical practices for measles-mumps-rubella vaccination among US pediatric international travelers. JAMA Pediatr. 2020;174(2):e194515.
Hyle EP, Rao SR, Jentes ES, Parker Fiebelkorn A, Hagmann SHF, Taylor Walker A, et al. Missed opportunities for measles, mumps, rubella vaccination among departing U.S. adult travelers receiving pretravel health consultations. Ann Intern Med. 2017;167(2):77–84.
Lee AD, Clemmons NS, Patel M, Gastañaduy PA. International importations of measles virus into the United States during the post-elimination era, 2001–2016. J Infect Dis. 2019;219(10):1616–23.
National Notifiable Diseases Surveillance System. Measles (rubeola): 2013 case definition. Atlanta: CDC; 2013. Available from: https://ndc.services.cdc.gov/conditions/measles/ .
Patel MK, Goodson JL, Alexander JP Jr., Kretsinger K, Sodha SV, Steulet C, et al. Progress toward regional measles elimination—Worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1700–5.
Pike J, Leidner AJ, Gastañaduy PA. A review of measles outbreak cost estimates from the US in the post-elimination era (2004–2017): Estimates by perspective and cost type. Clin Infect Dis. 2020;1(6):1568–76.
World Health Organization. Measles vaccines: WHO position paper—April 2017. Wkly Epidemiol Rec. 2017;92(17):205–27.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
Two OTC medications that are commonly available include: Dimenhydrinate: This antihistamine is an effective treatment for motion sickness, but should not be given to children 2 or younger ...
Car sickness is a type of motion sickness. Motion sickness occurs when the brain receives conflicting information from the inner ears, eyes, and nerves in the joints and muscles. Imagine a young child sitting low in the back seat of a car without being able to see out the window — or an older child reading a book in the car.
Deep breathing can bring fast relief to motion sickness. Singing is a great way to get your child to breathe deeply. Try singing a song with your child. At the very least it will take her mind off the nausea. If the motion sickness persists, have your child lie down and try putting a cool cloth over his head.
Convenient travel case. ... To prevent motion sickness, the first dose should be taken 1/2 to 1 hour before starting activity. To prevent or treat motion sickness, see below: Children 2 to under 6 years: give ½ to 1 chewable tablet every 6-8 hours; do not give more than 3 chewable tablets in 24 hours, or as directed by a doctor; Children 6 to ...
Motion sickness is more common in children ages 2 to 12 years old. Some medicines used to prevent or treat motion sickness are not recommended for children. Talk to your healthcare professional about medicines and correct dosing of medicines for motion sickness for children. Only give the recommended dosage.
2 to 5 years (12.5 mg): ½ Kids chewable; 6 to 11 years (25 mg): 1 Kids chewable; 12 and older (50 mg): 1 regular tablet or chewable; Give the medicine 1 hour before traveling or going to a fun-park. The tablets give 6 hours of protection and are very helpful. Benadryl can also be used to prevent motion sickness. Use this if you do not have any ...
Motion sickness (travel sickness) is common, especially in children. It is caused by repeated unusual movements during travelling. Written by a GP. ... Hyoscine, or scopolamine, patches are suitable for adults and for children over 10 years old. The medicine is absorbed through your skin, although this method of medicine delivery is slow so the ...
Sea-Band Wristband, Child, Colors May Vary, 1 Pair, Anti-Nausea Acupressure Motion or Morning Sickness. $ 6.18. Amazon. "Some studies show acupressure bands can decrease symptoms of motion ...
He or she may suggest an over-the-counter travel sickness medicine for children older than age 2. Use the correct amount based on your children's age. Some of these medicines cause sleepiness or even agitation. Always get advice from your healthcare provider and be careful when using them. Don't use a motion sickness patch.
Ginger is a reasonable alternative to other medications, but often only available in capsules. For children 2 to 12 years old, dimenhydrinate is really their only choice. For people 12 years old and older, meclizine or transdermal scopolamine offer similar motion sickness protection with relatively less side effects.
Use anti-motion sickness medicine. Dimenhydrinate (such as Dramamine) is sold in chewable tablets for kids ages 2 and older. It's available without a prescription. This medicine should be given an hour before traveling, and one dose helps prevent symptoms for about six hours. Consider child-sized acupressure wristband s (such as Sea-Bands ...
Children & Motion Sickness. For children aged 2-12 years, dimenhydrinate (Dramamine), 1-1.5 mg/kg per dose, or diphenhydramine (Benadryl), 0.5-1 mg/kg per dose up to 25 mg, can be given 1 hour before travel and every 6 hours during the trip.
Provide some cool air. In the car, set the fan or air conditioner to blow lightly on your child or crack the window for a breeze. On a boat, take him out on deck. For a smoother ride in a large car with two rows of backseats, secure him in the middle row rather than the rearmost row (and for safety's sake, never in the front).
Medically necessary liquid medications can be brought in your carry-on or checked luggage in reasonable quantities. Tell an officer that you have a medically necessary liquid before starting the screening process. You may be asked to open the liquid medication for additional screening. Insulin is allowed in carry-on or checked luggage in ...
Hyoscine hydrobromide (Kwells and Joy-Rides) Other brand names: Kwells Kids, Travel Calm, Scopoderm. Hyoscine hydrobromide (Kwells and Joy-Rides) Find out how hyoscine hydrobromide treats travel sickness and how to take it. NHS medicines information on hyoscine hydrobromide - what it's used for, side effects, dosage and who can take it.
Scopolamine - the most commonly prescribed medication for motion sickness. It must be taken before symptoms start. It is available as a patch that is placed behind the ear 6-8 hours before ...
Motion sickness is caused by repeated movements when travelling, like going over bumps in a car or moving up and down in a boat, plane or train. The inner ear sends different signals to your brain from those your eyes are seeing. These confusing messages cause you to feel unwell. Find out more about motion sickness, an unpleasant combination of ...
What is Travel-Ease? Travel-Ease is used in adults and children aged 12 years and older to treat or prevent nausea, vomiting and dizziness caused by motion sickness.. Travel-Ease is also used in adults to treat symptoms of vertigo (dizziness or spinning sensation) caused by disease that affects your inner ear.. Travel-Ease may also be used for purposes not listed in this medication guide.
Advise adults traveling with children to seek medical attention for an infant or young child with diarrhea who has signs of moderate to severe dehydration, bloody diarrhea, body temperature >101.3°F (38.5°C), or persistent vomiting (unable to maintain oral hydration). Adequate hydration is the mainstay of TD management.
Hyoscine hydrobromide travel sickness tablets can be taken by most adults and children from the age of 3 years. Patches for travel sickness can be used by most adults and children from the age of 10 years. Who may not be able to take hyoscine hydrobromide. Hyoscine hydrobromide is not suitable for some people.
For infants 6 months old and older, but younger than 12 months, this includes documented administration of 1 dose of MMR; for people aged ≥12 months, documentation should include 2 doses of MMR or MMRV (the first dose administered at age ≥12 months and the second dose administered no earlier than 28 days after the first dose).