- Help & Support
- Lung Health & Diseases
- Lung Procedures, Tests & Treatments
- Oxygen Therapy
- Traveling with Oxygen

Oxygen Therapy: Traveling with Oxygen
It may take more planning, but many people successfully travel while using oxygen therapy. Learn some key points to consider before you travel with oxygen.
- A compressed oxygen tank is oxygen gas stored in a tank under pressure. Small tanks can be carried.
- A liquid oxygen unit contains oxygen gas cooled to a very low temperature. Most tanks come with a portable unit that you can carry or pull on a cart.
- A portable oxygen concentrator (POC) takes in the air around you to concentrate oxygen and give you more of it. It uses electricity from a battery or by plugging into an outlet.
- You can use an FAA-approved portable oxygen concentrator (POC). Some airlines offer in-flight oxygen for a fee.
- You can’t use compressed gas or liquid oxygen on the plane.
- When you make your reservation, tell the airline that you’ll be using oxygen during the flight. You may need to send paperwork from your doctor or fill out the airline’s medical form.
- Bring extra POC batteries and your own nasal prongs.
- If you will be using the airline’s oxygen system, keep in mind that it’s only on the plane, not throughout the airport.
- Arrange for oxygen supplies during layovers and at your destination.
- Call the local bus or train office at least three days before you depart. Tell them that you’re traveling with oxygen. Ask about their policies. Most bus or train companies allow personal oxygen devices onboard.
- Bring extra oxygen units as baggage, if allowed.
- Carry your oxygen prescription with you.
- Place the oxygen unit upright. Put it on the floor or on the seat beside you. Secure the unit with a seat belt.
- Don’t smoke or let anyone else smoke in the car.
- Keep the windows open at least a crack so air can circulate.
- Don’t leave oxygen units in a hot car.
- When you book your cruise, tell the cruise company that you’ll be traveling with oxygen. Most cruise lines require a four- to six-week notice to travel with oxygen.
- Ask your healthcare provider to give the cruise company a letter that includes a brief health history and your oxygen prescription.
- Work with your oxygen supplier to have oxygen units sent to the cruise ship before you depart. Ask the supplier to tell you how many tanks you’ll need at ports of call. The supplier may be able to arrange those for you.
- Search online for special cruises for people on oxygen.
- Being around crowds can increase your risk of getting sick. Consider wearing a mask when you’re not using your oxygen. Wash your hands often. Don’t use alcohol-based hand sanitizers because they are flammable.
- If you are traveling out of the country, take extra precautions to understand airline policies. If you use a POC, make sure you have the right electrical adapter so you can plug it in.
- Work with a travel agent to help make plans for any travel abroad.
- If you have trouble breathing, appear pale or blue or have chest pain, seek medical attention right away.
If you use oxygen, make sure you know where you are getting oxygen during each leg of your trip.
You are not alone.
Many people with lung disease use oxygen. There are several ways you can connect with other people and lung disease experts to help you get started with oxygen:
- Call our free Lung HelpLine at 1-800-LUNGUSA (1-800-586-4872) or visit Lung.org/helpline to talk with a medical professional.
- Get started with a pulmonary rehabilitation program. Trained respiratory therapists can help answer your questions about oxygen and teach you how to stay active.
- Better Breathers Club . In-person or virtual meetings led by trained facilitators that offer educational and supportive connections.
- Patient & Caregiver Network . Nationwide, online patient support program providing direct access to education, support and connection to others also living with lung disease.
- Connect with other patients facing lung disease in one of our free online support communities .
Page last updated: November 17, 2022
A Breath of Fresh Air in Your Inbox
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Traveling with Supplemental Oxygen
Planning ahead when you need to take oxygen on a trip
Before Your Trip
Altitude and oxygen needs.
- Regulations on Airplanes
If you have a condition such as chronic obstructive pulmonary disease (COPD) and are planning to travel, you may need to take supplemental oxygen with you. When you are traveling on an airplane, by train, or on a bus, or staying in a hotel, you need to be aware of considerations and possible restrictions.
As you prepare for a trip with supplemental oxygen, check that your equipment and devices are permitted for use during your travel and at your destination. Be sure to ask whether you will have space and be afforded accommodations to use your device.
Prepare for your travels by bringing batteries or chargers to power your equipment. Keep in mind that international destinations and cruise ships may have power outlet configurations that do not match the ones you are used to.
When you are traveling with oxygen , it is important to plan ahead. It is a good idea to schedule a pre-trip medical examination, especially if you will be traveling on an airplane, hiking, staying at a high elevation (such as on a mountain), leaving the country, or going away for a long period of time.
Obtain a letter of medical necessity from your healthcare provider during your pre-trip medical exam. Most airlines require that this letter include your healthcare provider's contact information, a statement about your specific condition, healthcare provider approval for air travel, and confirmation that you require supplemental oxygen, as well as the flow rate and duration of use. You may need to present it when you go through airport security, board your plane, go through customs, and/or at your hotel if you need to stay in a specially accommodated room.
Don't forget to pack all of your regular medications in your carry-on luggage and, if needed, to bring an adequate supply of COPD rescue inhalers with you throughout your trip.
It's always a good idea to keep any medications in their original containers so that you will get the right treatment in case of an emergency.
A high altitude may change the oxygen pressure around you—essentially increasing your oxygen requirement. This doesn't have a significant effect on most people, but if you have a pulmonary disease, a slight change in oxygen pressure can make you feel short of breath.
Your healthcare provider may change your prescription for oxygen supplementation if you are staying at a high elevation or flying during your travels. In fact, some people who do not regularly need to use supplemental oxygen might need to use it only in these circumstances.
Supplemental Oxygen on Airplanes: Regulations
When making an airline reservation, be sure to ask about specific regulations and restrictions that may apply when carrying oxygen onboard your flight.
According to the U.S. Department of Transportation Nondiscrimination on the Basis of Disability in Air Travel Act, oxygen-dependent passengers may now carry their own Federal Aviation Administration (FAA)-approved, battery-powered portable oxygen concentrators (POCs) onboard U.S. domestic and international flights with 19 or more passenger seats, beginning or ending in the United States.
The policy states that:
- Airlines must permit a passenger to use his/her POC during the flight if it is labeled as FAA-approved.
- Airlines may not charge for providing accommodations required by the rule, such as hazardous materials packaging for batteries.
- Airlines may charge for optional services such as providing oxygen.
Assistive devices do not count against any limit on the number of pieces of carry-on baggage, and they have priority over other items for storage in the baggage compartment.
In addition to POCs, respiratory assistive devices also include nebulizers, respirators, and continuous positive airway pressure (CPAP) machines. Liquids associated with a nebulizer are exempt from the 3-1-1 liquids rule.
Compressed oxygen tanks and liquid oxygen are not allowed on airplanes.
FAA-Approved POCs
POCs are permitted on flights only if they are approved by the FAA. Consider renting your POC from an oxygen supply company if you don't typically need oxygen, or if the device you regularly use is not FAA-approved.
According to the FAA, the following devices are approved to carry on board your flight:
- AirSep FreeStyle
- AirSep LifeStyle
- AirSep Focus
- AirSep Freestyle 5
- (Caire) SeQual eQuinox Oxygen System (model 4000)
- Delphi RS-00400 / Oxus RS-00400
- DeVilbiss Healthcare iGo
- Inogen One G2
- lnogen One G3
- lnova Labs LifeChoice Activox
- International Biophysics LifeChoice / lnova Labs LifeChoice
- Invacare XPO2 / XPO 100
- Invacare Solo2
- Oxylife Independence Oxygen Concentrator
- Precision Medical EasyPulse
- Respironics EverGo
- Respironics SimplyGo
- SeQual Eclipse
- SeQual SAROS
- VBox (3B Medical) Trooper (Aer X) Oxygen Concentrator
For more information about FAA requirements for traveling with oxygen by airplane, visit the FAA website .
World Standards. Plug and socket types .
European Federation of Allergy and Airways Diseases Patients Associations. Enabling air travel with oxygen in Europe: an EFA booklet for patients with chronic respiratory disease .
Federal Aviation Administration. Acceptance criteria for portable oxygen concentrators .
Stoller JK. Patient education: supplemental oxygen on commercial airlines (Beyond the Basics) .
Transporation Security Administration. Disabilities and medical conditions: respiratory equipment .
US Department of Transportation. Passengers with disabilities: about the Air Carrier Access Act .
By Deborah Leader, RN Deborah Leader RN, PHN, is a registered nurse and medical writer who focuses on COPD.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.62(595); February 2012

Air travel for patients with chronic obstructive pulmonary disease: a case report
Introduction.
This case report aims to assist primary care physicians in managing borderline hypoxemic patients with chronic obstructive pulmonary disease (COPD), enabling them to fly safely.
CASE REPORT
A 63-year-old female smoker (80 pack years) travelled from Athens, Greece to Amsterdam in The Netherlands. She had been diagnosed with hypertension, moderate COPD, mild cardiac failure, and severe osteoarthritis in the left knee. Thirty minutes after take-off she started to experience severe dyspnea, without tachycardia or chest pain, that required immediate medical attention. After administering oxygen at 2L/min, the symptoms slowly improved and she arrived safely in Amsterdam.
The patient had experienced similar symptoms during other flights in the past. Her GP thought that she should be examined by cardiologists and pulmonologists to assess the possible need for in-flight oxygen supplementation. The cardiologist conducted a full clinical examination, as well as an electrocardiogram and heart ultrasound, and decided that, as the cause of the oxygen desaturation during flight was not from her heart, she should be referred to pulmonologists for further assessment.
The pulmonologists conducted spirometry and an arterial saturated oxygen (SaO 2 ) test. The results were: a forced expiratory volume in 1second (FEV1) of 60% predicted; an FEV1/forced vital capacity (FVC) of 0.65; and a SaO 2 of 94%. The patient did not perform a 6-minute walking distance test (6MWT) as this was not possible due to the severe osteoarthritis of her left knee. As a hypoxia inhalation test was not available, even in the tertiary hospital, the pulmonologist said that the patient would probably need in-flight oxygen supplementation. This was based only on the available calculations (equations) for determining the need for oxygen supplementation in flight. The pulmonologist did not give precise advice to the patient and, as a result, the patient experienced the same dyspnea during flight as she had done before.
As the patient had experienced severe dyspnoea in previous flights, should her doctors be more careful and prepare her journey in a safer way?
COPD is a major public-health problem that, it is estimated, will be the fourth leading cause of death by 2030. 1 Two billion passengers travel each year by airplane; 2 18–44% have COPD. 3 , 4 Patients with moderate to severe COPD often develop symptoms due to hypoxia during flight, and most of them do not consult a physician before air travel as they have non-clinically significant hypoxemia at sea level. 3 A study in Norway showed that 25% of the patients with COPD developed hypoxia-related symptoms in flight. 4
Air pressure drops as altitude increases. The effects of increased altitude and the associated hypobaric features can result in hypoxia. Healthy individuals respond to hypoxia by increasing ventilation, balancing the hypobaric changes without any symptoms. Ventilation can be increased by increasing tidal volume and/or increasing respiratory rate. 5 However, increasing tidal volume for patients with respiratory problems, and especially for those with COPD, is a difficult task as they are often hyperinflated. Patients with respiratory failure will always need in-flight oxygen; it is highly likely that patients with moderate to severe COPD need in-flight oxygen as well.
Investigations
In patients with COPD, previous experiences during flights, medical history including GOLD-stage status, dyspnea assessment, and clinical examination should all be assessed. The physiological tests to assess fitness for flight that are currently available are:
- spirometry;
- diffusing capacity tests;
- arterial blood gas tests;
- saturation;
- hypoxemia prediction equations; and
- the hypoxia inhalation test.
Although the practical usefulness of FEV1, partial pressure of oxygen in the blood (PaO 2 ), and SaO 2 tests in successfully assessing the need for oxygen supplementation is questioned in several publications, 6 , 7 a rule of thumb is that patients with an SaO 2 of >95% will probably not need oxygen during flight, while those with an SaO 2 of <92% will. Patients with an SaO 2 of 92–95% are considered borderline. 8 The need for oxygen supplementation in patients with COPD during flights can be calculated using different equations. For example:
Although this equation is usually reliable, it might be inaccurate in borderline situations. In such cases, the most accurate test is the hypoxia inhalation test by breathing an oxygen fraction of 15% at sea level; however, this is seldom performed in clinical practice. Patients with a post-hypoxia inhalation test saturation of <85% need in-flight oxygen. Independently, if a hypoxia-altitude simulation test or a hypobaric chamber is used to achieve hypoxia conditions, special caution to oxygen titration is needed — using a nasal cannula underestimates the oxygen dose required. The oxygen delivery equipment can result in the same PaO 2 when a continuous-flow or oxygen-conserving device is used, whereas PaO 2 is lower when portable oxygen concentrators (POCs) are used. 10
In-flight oxygen is usually prescribed at a rate of 2–4L/min and should be given by nasal cannulae. 7 This will partially reverse altitude-induced hypoxemia symptoms in patients with COPD. 11 Nowadays, many airlines allow POCs on board, but often only specific types. 7 Box 1 shows a practical guidance to help ensure safe air travel for patients with COPD.
Box 1. Guidance to help ensure safe air travel for patients with COPD
For patients.
- Plan routes and carriers, and ask for their policy regarding oxygen
- Ask your doctor for the appropriate assessment(s)
- Inform carriers and airport authorities 1 week before departure about your requirements for oxygen during the flight, and transportation to and from the aircraft
For doctors
- Take a full history from patients with respiratory diseases, including previous symptoms during flights, medical history, and comorbidities
- Assess your patient 1 month before departure, taking into account specific trip details
- Provide your patient with formal papers stating the disease and estimated oxygen flow necessary on board
- Use the Frequent Traveller's Medical Card in order to obtain extensive details on medical history for patients who travel frequently by air
For patients and doctors
- Visit the website of the European Lung Foundation (ELF, www.european-lung-foundation.org ). The ELF has created a database that gives information and individual oxygen policies for over 300 major airlines in Europe. This is useful as airline policies can vary greatly.
The patient has provided written consent for this article to be published.
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Hosted content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 67, Issue 11
- Air travel and chronic obstructive pulmonary disease: a new algorithm for pre-flight evaluation
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Anne Edvardsen 1 , 3 ,
- Aina Akerø 2 ,
- Carl C Christensen 1 ,
- Morten Ryg 1 ,
- Ole H Skjønsberg 2 , 3
- 1 Department of Respiratory Physiology, Glittreklinikken, Hakadal, Norway
- 2 Department of Pulmonary Medicine, Oslo University Hospital, University of Oslo, Oslo, Norway
- 3 Faculty of Medicine, University of Oslo, Oslo, Norway
- Correspondence to Anne Edvardsen, Department of Respiratory Physiology, Glittreklinikken, 1485 Hakadal, Norway; anne.edvardsen{at}glittreklinikken.no
Background The reduced pressure in the aircraft cabin may cause significant hypoxaemia and respiratory distress in patients with chronic obstructive pulmonary disease (COPD). Simple and reliable methods for predicting the need for supplemental oxygen during air travel have been requested.
Objective To construct a pre-flight evaluation algorithm for patients with COPD.
Methods In this prospective, cross-sectional study of 100 patients with COPD referred to hypoxia-altitude simulation test (HAST), sea level pulse oximetry at rest (SpO 2 SL ) and exercise desaturation (SpO 2 6MWT ) were used to evaluate whether the patient is fit to fly without further assessment, needs further evaluation with HAST or should receive in-flight supplemental oxygen without further evaluation. HAST was used as the reference method.
Results An algorithm was constructed using a combination of SpO 2 SL and SpO 2 6MWT . Categories for SpO 2 SL were >95%, 92–95% and <92%, the cut-off value for SpO 2 6MWT was calculated as 84%. Arterial oxygen pressure (PaO 2 HAST ) <6.6 kPa was the criterion for recommending supplemental oxygen. This algorithm had a sensitivity of 100% and a specificity of 80% when tested prospectively on an independent sample of patients with COPD (n=50). Patients with SpO 2 SL >95% combined with SpO 2 6MWT ≥84% may travel by air without further assessment. In-flight supplemental oxygen is recommended if SpO 2 SL =92–95% combined with SpO 2 6MWT <84% or if SpO 2 SL <92%. Otherwise, HAST should be performed.
Conclusions The presented algorithm is simple and appears to be a reliable tool for pre-flight evaluation of patients with COPD.
- Pulmonary disease
- chronic obstructive
- ambulatory oxygen therapy
- COPD epidemiology
- COPD mechanisms
- long-term oxygen therapy (LTOT)
- pulmonary rehabilitation
- respiratory measurement
https://doi.org/10.1136/thoraxjnl-2012-201855
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Key messages
What is the key question.
Can pulse oximetry at rest and during exercise be used to decide whether patients with chronic obstructive pulmonary disease (COPD) should use supplemental oxygen during air travel?
What is the bottom line?
A simple and reliable pre-flight evaluation algorithm for patients with COPD based on sea-level pulse oximetry at rest and during a 6 min walk test is presented.
Why read on?
The pre-flight evaluation algorithm might be useful for physicians treating patients with COPD.
Introduction
The reduced atmospheric pressure in the aircraft cabin may cause severe in-flight hypoxaemia and respiratory symptoms in patients with lung disease, for example, chronic obstructive pulmonary disease (COPD). 1–9 With the growing prevalence of COPD 10 and a large proportion of patients with COPD travelling by air, 1 , 9 simple and practical methods for pre-flight evaluation of the patients' fitness to air travel have been requested. 1 , 3 , 11
Current air travel statements 1 , 2 , 12 recommend supplemental oxygen when the arterial oxygen pressure (PaO 2 ) is expected to fall below 6.6 or 7.3 kPa (50 or 55 mm Hg). Various lung function variables, prediction equations and algorithms have been proposed to estimate in-flight PaO 2 , the need for in-flight supplemental oxygen, and to select patients needing more advanced pre-flight testing, such as the hypoxia-altitude simulation test (HAST). 1 , 3 , 6 , 13–20 HAST is considered to be the clinical ‘gold standard’, 3 , 21 but is time consuming and not widely available. Thus, it is important to minimise the number of patients needing referral to HAST. Prediction equations, sea level PaO 2 and spirometric values alone have proven not to be reliable tools for estimating the risk of severe in-flight hypoxaemia. 1 , 3–5 , 16 , 22 In an algorithm published by the British Thoracic Society (BTS), sea-level oxygen saturation by pulse oximetry (SpO 2 SL ) was used as a discriminating variable, 13 and it was recently confirmed that a SpO 2 SL <92% seems to be an appropriate cut-off value for recommending in-flight supplemental oxygen without further pre-flight evaluation. 23 For SpO 2 SL ≥92%, however, the predictive properties for detecting in-flight hypoxaemia were lower. 23 It has been shown that both exercise desaturation 15 , 24 , 25 and aerobic capacity 4 , 5 correlate significantly with in-flight PaO 2 . Thus, it would be of interest to study if a combination of SpO 2 SL and standardised exercise testing could be used to minimise the number of patients needing more cumbersome pre-flight testing. Our hypothesis was that a combination of SpO 2 SL and oxygen desaturation during a 6 min walk test (6MWT) can be used to differentiate between patients with COPD needing or not needing supplemental oxygen during air travel, and patients who need further pre-flight evaluation with HAST.
To test this hypothesis, SpO 2 was measured in a group of patients with COPD at rest and during a 6MWT, and the results were compared with oxygen tension and saturation obtained during HAST. The primary aim of the study was to develop a simple and reliable algorithm for pre-flight evaluation of patients with COPD based on these variables. The secondary aim of the study was to evaluate if HAST can be performed with SpO 2 as a substitute for PaO 2 , since use of a non-invasive HAST could make the test simpler to perform and thereby more available.
This prospective cross-sectional study was performed at a pulmonary rehabilitation hospital in Norway. The Regional Committee for Medical Research Ethics approved the study (S-08640b), and written informed consent was obtained from the participants. The study was recorded in ClinicalTrials.gov ( NCT00896584 ).
Construction of the algorithm
The construction of the algorithm was based on sea-level measurements of lung function, blood gases, pulse oximetry and 6MWT. For recommending in-flight oxygen, PaO 2 HAST <6.6 kPa was chosen. 1 , 14 , 21 , 26 To make the algorithm practical and clinically useful, the non-invasive variables with highest correlation to PaO 2 HAST were analysed with receiver operating characteristics (ROC) analysis, first including all participants and second with subjects grouped according to SpO 2 >95%, 92–95% and <92%. 13 Results from the ROC analyses served as a basis for the construction of the algorithm, and thereafter all subjects were individually tested for calculation of the sensitivity and specificity of the new algorithm. Finally, the algorithm was prospectively validated on an independent sample of patients with COPD.
One hundred and thirty-nine consecutive patients with COPD who were referred from chest physicians in southern Norway to pre-flight evaluation were invited to participate in the study. The referral criteria were moderate to very severe COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), 27 previous air travel intolerance, or SpO 2 SL ≤95%. 1 , 13 The inclusion criteria were a diagnosis of moderate to very severe COPD 27 and the ability to perform a 6MWT. Exclusion criteria were unstable angina, uncontrolled hypertension, uncontrolled arrhythmia and long-term oxygen treatment. Thirty-nine patients were excluded, resulting in a study population of 100 subjects ( figure 1 ). Sixty-nine of the participants had known comorbidities, the most frequent being systemic arterial hypertension, ischaemic heart disease and muscular-skeletal disorders. All patients used their daily medication.
- Download figure
- Open in new tab
- Download powerpoint
Flow chart describing the patient selection. COPD, chronic obstructive pulmonary disease; 6MWT, 6 min walk test; HAST, hypoxia-altitude simulation test; LTOT, long-term oxygen treatment.
Fifty additional patients with COPD who were referred to HAST with equal criteria as the study population were used to validate the algorithm.
Sea-level measurements and HAST
Lung function tests were performed according to standard criteria. SpO 2 SL was measured with pulse oximetry (Nonin 3100 Wristox or Nonin PalmSat 2500, Nonin Medical Inc, North Plymouth, Massachusetts, USA), and simultaneously an arterial blood sample was drawn from a radial artery catheter and immediately analysed (ABL800 Flex, Radiometer, Copenhagen, Denmark). Exercise-related dyspnoea was measured with the modified Medical Research Council Dyspnoea Scale (mMRC). 28
The 6MWT was performed in accordance with standard criteria, 29 and SpO 2 and dyspnoea (Borg CR10 30 ) were recorded every minute. None of the patients used supplemental oxygen during the 6MWT.
HAST was used to simulate a cabin pressure corresponding to an altitude of 2438 m above sea level (8000 ft). 6 The subjects breathed 15.1% oxygen (15.1% O 2 , 84.9% N 2 , Yara Praxair, Norway) from a non-diffusing gas collection bag (170 litre Douglas-bag, Hans Rudolph Inc, Shawnee, USA) through a facemask (Mirage Full Face Mask, ResMed Corp, Poway, California, USA), and arterial blood samples were taken after 15 min hypoxic exposure. 6 , 18 The SpO 2 should be stable for 5 min before arterial blood sampling, otherwise the test was prolonged to 20 min. Electrocardiogram, SpO 2 and dyspnoea were continuously monitored. The patients were recommended in-flight supplemental oxygen if PaO 2 HAST was <6.6 kPa. 1
To calculate sample size, we assumed that sensitivity and specificity would be approximately 80% in the planned study. It was then shown that 100 patients were needed to construct a new algorithm in which sensitivity and specificity should have CI length <16%. Patient characteristics are presented as mean and SD, unless otherwise specified. Relations between PaO 2 HAST and patient characteristics were assessed from Pearson's correlation coefficient and one-way repeated measures analysis of variance. ROC analyses were performed with sea-level SpO 2 , SpO 2 during 6MWT (SpO 2 6MWT ) and walking distance against PaO 2 HAST <6.6 kPa as the discriminating variables. Statistical analyses were performed with PASW software (V.18.0; Chicago, Illinois, USA). Differences were considered significant if p<0.05.
Patient characteristics
The study comprised patients with COPD (n=100), with demographic characteristics as presented in table 1 . According to the GOLD classification, 27 22%, 46% and 32% were in the GOLD categories II, III and IV, respectively.
- View inline
Baseline patient characteristics, n=100
Sea-level SpO 2 was used as a grouping variable as follows: SpO 2 SL >95% (12% of patients), SpO 2 SL 92–95% (55% of patients) and SpO 2 SL <92% (33% of patients).
All patients were tested with HAST. Mean HAST values for PaO 2 and SpO 2 were 6.3 kPa (SD 0.6 kPa) and 83% (SD 4%), respectively. Seventy-three per cent of patients had a PaO 2 HAST <6.6 kPa, indicating that they, in accordance with current guidelines, should use in-flight supplemental oxygen. There was an increase of 0.8 (SD 1.0) in dyspnoea score (Borg CR10) (p<0.001). Eighteen per cent of patients reported moderate to strong dyspnoea (Borg score 3–6), but there was no significant correlation between dyspnoea score and PaO 2 HAST (r=0.16, p=0.115). None of the patients experienced hypoxia-induced myocardial ischaemia or arrhythmias.
Walking test
The patients covered a distance varying from 150 to 604 m during the 6MWT ( table 1 ). The mean decrease in SpO 2 during the 6MWT was 10% (SD 5%) (p<0.001), and the mean SpO 2 6MWT was 83% (SD 6%) ( table 1 ).
Associations between in-flight PaO 2 and sea-level characteristics
Significant correlations between sea=level characteristics and in-flight PaO 2 are presented in table 2 . PaO 2 SL , SpO 2 6MWT and SpO 2 SL showed the strongest correlation with PaO 2 HAST PaO 2 SL was not included in the further analyses since one aim of the study was to develop a non-invasive evaluation method. Diffusing capacity of the lung for carbon monoxide ( D L,CO), D L,CO/alveolar volume, total lung capacity (TLC), residual volume (RV), RV/TLC and dyspnoea measured with mMRC showed no significant relationship with in-flight PaO 2 .
Variables with significant correlation to PaO 2 during HAST, n=100
ROC analyses were used as the basis for developing the pre-flight evaluation algorithm. SpO 2 SL and SpO 2 6MWT showed good diagnostic properties (area under curve 0.78 and 0.79, respectively) for detection of in-flight PaO 2 <6.6 kPa ( figure 2 ). The patients were grouped and data analysed according to the BTS pulse oximetry categories, SpO 2 SL >95%, 92–95% and <92% ( figure 3 ). In the group with sea-level SpO 2 SL <92%, 30 of 33 (91%) patients dropped below the recommended level for minimum in-flight PaO 2 (6.6 kPa), and were thereby in need of supplemental oxygen during air travel. Regarding the 55 patients in the group with SpO 2 SL from 92% to 95%, a ROC analysis with SpO 2 6MWT showed good prognostic properties (area under curve 0.80) for detection of in-flight PaO 2 <6.6 kPa. The suggested cut-off value was SpO 2 6MWT <84% (sensitivity 88%, 95% CI 80% to 96%; specificity 69%, 95% CI 52% to 85%). With regard to patients with SpO 2 SL >95%, 5 of 12 (42%) had an in-flight PaO 2 <6.6 kPa. In this group, ROC analysis showed exercise desaturation as a good prognostic variable, with an optimal cut-off value for SpO 2 6MWT <84% (area under curve 0.71; sensitivity 80%, 95% CI 40% to 100%; specificity 71%, 95% CI 29% to 100%).
Receiver operating characteristics curves: (A) sea-level SpO 2 , with PaO 2 HAST <6.6 kPa or ≥6.6 kPa as the discriminating variable, area under curve 0.78; and (B) SpO 2 during the 6MWT, with PaO 2 HAST <6.6 kPa or ≥6.6 kPa as the discriminating variable, area under curve 0.79. 6MWT, 6 min walk test; HAST: hypoxia-altitude simulation test; PaO 2 , arterial oxygen pressure; SpO 2 , arterial oxygen saturation measured with pulse oximetry.
SpO 2 during 6MWT versus PaO 2 HAST . Patients are grouped after sea-level SpO 2 >95%, 92–95% and <92%. Recommended level for minimum in-flight PaO 2 (6.6 kPa) and cut-off for exercise desaturation (84%) is marked. 6MWT, 6 min walk test; HAST, hypoxia-altitude simulation test; PaO 2 , arterial oxygen pressure; SpO 2 , arterial oxygen saturation measured with pulse oximetry; ●, SpO 2 >95%; ●, SpO 2 92–95%; ○, SpO 2 <92%.
Based on the above analyses a pre-flight evaluation algorithm was constructed ( figure 4 ). The algorithm was based on sea-level resting pulse oximetry (SpO 2 SL ) and exercise desaturation during the 6MWT (SpO 2 6MWT ) as the primary and secondary discriminator for evaluating whether the patient was fit to fly without further assessment, in need of further evaluation with HAST or should receive in-flight supplemental oxygen without further evaluation.
Pre-flight evaluation algorithm. 6MWT, 6 min walk test; alt, alternatively; HAST, hypoxia-altitude simulation test; PaO 2 , arterial oxygen pressure; SpO 2 , arterial oxygen saturation measured with pulse oximetry.
The pre-flight evaluation algorithm had a sensitivity of 99% (95% CI 96% to 100%) and a specificity of 82% (95% CI 67% to 96%) when all 100 subjects were individually tested. According to the algorithm, one-third (33%) of the patients would be advised to perform extended pre-flight testing with HAST. Six per cent of the patients were not correctly classified by the algorithm; of these, one patient was misclassified as fit to fly despite a PaO 2 HAST <6.6 kPa (SpO 2 SL 97% and SpO 2 6MWT 87%, measured PaO 2 HAST 6.3 kPa), and five patients would have been recommended to use in-flight oxygen without, in fact, having a PaO 2 HAST <6.6 kPa (mean PaO 2 HAST 7.2 kPa (SD 0.3 kPa)). The patients selected by the algorithm for further pre-flight evaluation with HAST had a mean PaO 2 HAST of 6.6 kPa (SD 0.6 kPa).
After the algorithm was established, it was prospectively validated on an independent sample of 50 patients with COPD who were referred to HAST ( table 3 ). Eight patients had SpO 2 SL >95% (16%), 27 patients had SpO 2 SL 92–95% (54%) and 15 patients had SpO 2 SL <92% (30%). For all but four patients a correct choice was obtained with regard to use of in-flight supplemental oxygen. These four patients were recommended supplemental oxygen without having a PaO 2 HAST <6.6 kPa. However, it should be noted that they all had PaO 2 HAST values close to the recommended limit (mean PaO 2 HAST 6.6 kPa (SD 0.1 kPa)). The sensitivity and specificity for the algorithm in this independent sample of patients were 100% (95% CI 90% to 100%) and 80% (95% CI 60% to 95%), respectively. The 20 patients which the algorithm selected for further pre-flight evaluation with HAST had a mean PaO 2 HAST of 6.9 kPa (SD 0.5 kPa).
Baseline characteristics for patients used in the separate validation of the algorithm, n=50
HAST: PaO 2 versus SpO 2
The secondary aim was to evaluate if HAST can be performed with SpO 2 as a substitute for PaO 2 . There was a strong correlation between PaO 2 HAST and SpO 2 HAST (r=0.81, p<0.001) during HAST. The area under the ROC curve when using pulse oximetry to detect in-flight PaO 2 <6.6 kPa was 0.93, indicating strong prognostic properties for the method ( figure 5 ). The analysis suggested a cut-off value for SpO 2 HAST ≤85% with a sensitivity of 89% (95% CI 81% to 96%) and a specificity of 81% (95% CI 67% to 96%) when SpO 2 HAST was used as a substitute for PaO 2 HAST <6.6 kPa ( figure 5 ). When using SpO 2 HAST , instead of PaO 2 HAST an independent sample of 50 patients with COPD, we obtained a sensitivity of 90% (95% CI 77% to 100%) and a specificity of 85% (95% CI 70% to 100%). Three patients were misclassified as fit to fly despite having PaO 2 HAST <6.6 kPa (mean PaO 2 HAST 6.3 kPa), and three patients would have been recommended to use in-flight oxygen without, in fact, having a PaO 2 HAST <6.6 kPa (mean PaO 2 HAST 6.7 kPa).
Receiver operating characteristics curve of SpO 2 HAST as a substitute for PaO 2 HAST < or ≥6.6 kPa, area under curve 0.93. HAST, hypoxia-altitude simulation test; PaO 2 , arterial oxygen pressure; SpO 2 , arterial oxygen saturation measured with pulse oximetry.
A large number of patients with COPD travel by air, most of them without severe in-flight medical problems. 9 , 13 However, some patients develop severe hypoxaemia. 1 , 2 , 4–7 Thus, simple and consistent pre-flight assessment guidance regarding the need for in-flight supplemental oxygen has been requested. 1 , 3 , 11 In the present study we have constructed and validated a simple and clinically feasible algorithm for pre-flight assessment of patients with COPD based on sea-level resting SpO 2 and SpO 2 values during a 6MWT.
Various proposed equations and single sea-level variables have proven not to predict in-flight hypoxaemia with a satisfactory precision. 1 , 3–5 , 16 , 22 Several authors have suggested that exercise-related outcomes may be useful discriminators. 4 , 5 , 14 , 24 , 25 Previous studies from our group show that aerobic capacity correlates with in-flight hypoxaemia. 4 , 5 Chetta et al showed that desaturation during the 6MWT provides useful information in the pre-flight assessment. 24 Since oxygen saturation measured with pulse oximetry, at rest and during a 6MWT, is frequently used in the medical care of patients with COPD, 31 an algorithm employing a combination of these variables would be simple to implement in a busy clinical practice. An assessment algorithm that can discriminate between patients who will need supplemental oxygen during air travel and those who can travel without such equipment would be of considerable value in the evaluation of patients with COPD intending to travel by air, especially if the number of unequivocal findings needing more extensive pre-flight evaluation is reduced.
The results from our group have previously indicated that the BTS algorithm with only sea-level SpO 2 cannot be used with confidence to predict in-flight hypoxaemia. 23 A large number of patients at risk of developing severe hypoxaemia was not detected, and a considerable number of patients needed more advanced pre-flight evaluation. 23 By adding a 6MWT, including measurement of SpO 2 , the current study shows that the number of patients needing referral to HAST was markedly reduced. The 6MWT is a widely used test to assess exercise performance in patients with COPD, and is much more available than HAST. However, it is important that the 6MWT is performed according to guidelines, and it must be stressed that shortcuts must be avoided. 29 The suggested algorithm has a high sensitivity, which was reproduced when applying it prospectively on a separate group of patients with COPD. None of these study subjects were misclassified as fit to fly without supplemental oxygen. Due to somewhat lower specificity, the algorithm overestimated the risk of in-flight hypoxaemia, resulting in unnecessary use of supplemental oxygen in 8% of the patients.
According to our results, patients with COPD who have SpO 2 SL >95% and without severe exertional desaturation (SpO 2 ≥84%) can travel safely by air without further pre-flight assessment. In addition, further pre-flight assessment is not necessary in patients with SpO 2 SL <92% 13 , 23 or in patients with SpO 2 SL 92–95% and SpO 2 6MWT <84%. These patients should, according to our results, be equipped with supplemental oxygen during the flight. Thus, extended pre-flight assessment with HAST might be limited to patients with either the combination of resting SpO 2 SL >95% and severe exercise desaturation (SpO 2 <84%) and to patients with SpO 2 SL between 92% and 95% without severe exercise desaturation (≥84%). In these two groups of patients, the level of in-flight hypoxaemia was difficult to predict, underlining the need for pre-flight testing with HAST.
Even though HAST is increasingly used in pre-flight assessment, 32 , 33 it is not widely available. 11 , 21 HAST has been shown to be a good predictor of in-flight PaO 2 18 , 32 , 34 , 35 and the results obtained are reproducible. 32 However, one might find it cumbersome to take repeated arterial blood samples or insert a radial artery catheter, and substitution of arterial blood gas measurement with pulse oximetry would simplify the HAST procedure considerably. To our knowledge, comparison of arterial blood gases and pulse oximetry during HAST has not previously been published. As expected, a strong correlation between PaO 2 HAST and SpO 2 HAST was observed, and when using a cut-off value for SpO 2 HAST ≤85% as a substitute for a PaO 2 HAST <6.6 kPa, acceptable values for sensitivity and specificity of the test were obtained. Our results show that use of pulse oximetry during HAST may underestimate the need for in-flight oxygen. Thus, the authors would recommend arterial blood gas measurement during HAST as the method of choice.
To our knowledge, this is the first prospective study to use a set of common baseline characteristics for the construction of a pre-flight evaluation algorithm. The good prognostic properties of the algorithm were confirmed by a prospective validation on a separate group of subjects with COPD. However, it should be noted that a selected group of patients was studied; they were all referred for pre-flight evaluation. These are the patients for whom the algorithm is intended. One must also keep in mind that the present study only comprised patients with moderate to very severe COPD 27 and that the algorithm may not be applicable to patients with other lung diseases.
In conclusion, an algorithm for pre-flight evaluation of patients with COPD is presented, employing simple non-invasive oximetry at rest and during walking. By using the algorithm, the majority of a population consisting of patients with moderate to very severe COPD could be classified as fit to fly or in need of supplemental oxygen without more advanced pre-flight assessment.
Acknowledgments
Leiv Sandvik, Professor in Biostatistics, Oslo University Hospital, is gratefully acknowledged.
- Ahmedzai S ,
- Balfour-Lynn IM ,
- ↵ Aerospace Medical Association Medical Guidelines Task Force . Medical guidelines for Airline Travel, 2nd ed . Aviat Space Environ Med 2003 ; 74 : A1 – 19 . OpenUrl PubMed Web of Science
- Silverman D ,
- Christensen CC ,
- Refvem OK ,
- Edvardsen A ,
- Gong H Jr ,
- Tashkin DP ,
- Dillard TA ,
- Beninati WA ,
- Shiner RJ ,
- Partridge MR
- Hardie JA ,
- McBurnie MA ,
- Vollmer WM ,
- Shrikrishna D ,
- ↵ British Thoracic Society . Managing passengers with respiratory disease planning air travel: British Thoracic Society recommendations . Thorax 2002 ; 57 : 289 – 304 . OpenUrl FREE Full Text
- Faughnan ME ,
- Stanbrook MB ,
- Rajagopal KR ,
- Moores LK ,
- Bilello KL ,
- Robson AG ,
- Hartung TK ,
- Martin SE ,
- Bradley JM ,
- Castagnetti C ,
- ↵ The Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) . 2010 . http://www.goldcopd.org/ (accessed 16 Jun 2012).
- Mahler DA ,
- ↵ ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories . ATS Statement: guidelines for the six-minute walk test . Am J Respir Crit Care Med 2002 ; 166 : 111 – 17 . OpenUrl CrossRef PubMed Web of Science
- Palange P ,
- Carlsen KH ,
- Naughton MT ,
- Rochford PD ,
- Pretto JJ ,
- Swanney MP ,
- Seccombe LM ,
Funding The study was funded by grants from The Norwegian Heart and Lung Patient Organisation and The Norwegian Foundation for Health and Rehabilitation.
Competing interests None.
Ethics approval Ethics approval was provided by The Regional Norwegian Committee for Medical Research Ethics.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Continuous Flow
- Pulse Flow and Continuous Flow
- FAA-Approved
- All Portable Oxygen Concentrators
- Accessories
- Stationary Oxygen Concentrators
- Philips Respironics
- Precision Medical
- Rhythm Healthcare
- Customer Reviews
- ❓Quiz: What Portable Concentrator is Best For You?
- User Manuals
- Arya Biomed Corp Company Profile
- Caire Inc Company Profile
- GCE Healthcare Company Profile
- Philips Respironics Company Profile
- ResMed Company Profile
- How to Select a Portable Oxygen Concentrator?
- Best Portable Oxygen Concentrators - 2022
- CAIRE SeQual Eclipse 5 Review
- CAIRE Freestyle Comfort Review
- CAIRE Airsep Focus Review
- ResMed Mobi Review
- Philips Respironics SimplyGo Mini Review
- Philips Respironics SimplyGo Review
- Oxlife Independence Review
- GCE Zen-O Review
- GCE Zen-O Lite Review
- State Laws About Driving With Oxygen in the US
- How to Travel With Oxygen on a Plane
- 39 Airlines That Allow Portable Oxygen Concentrators
- Best Portable O2 Concentrators for High Altitude
- Best Portable Oxygen Concentrators for Travel
- Return & Exchange Agreement
- Financing Return & Exchange Policy
- Customer Service Ticket
Travel With COPD: Effective Tips For Safe and Easy Travel
Chronic Obstructive Pulmonary Disease (COPD) is a debilitating respiratory condition that creates several lifestyle challenges for its victims. Despite prolonged survival — thanks to new therapies , better management plans, and innovative technologies — substantial burdens remain for individuals with moderate to severe lung diseases.. Environmental exposure to various pollutants is particularly concerning, and forces some patients to remain homebound.
Taxing disease management makes it harder for some COPD patients to travel. But with a little extra planning and preparation, traveling with COPD is entirely possible. It only requires making simple, yet significant, pre-travel plans to ensure a safe trip.
To learn more about traveling with COPD, continue reading!
What is COPD?
Chronic Obstructive Pulmonary Disease, or COPD for short, is a chronic lung disease that causes airflow blockage and breathing-related problems. Its hallmark symptoms include breathing difficulty, wheezing, frequent coughing, mucous production, and chest pain or tightness.
COPD pertains to a group of lung diseases clustered in the same category, including Chronic Bronchitis and Emphysema. It's a progressive disease, meaning it will worsen over time, especially in the absence of medical intervention.
COPD is a significant cause of disability for most patients, forcing some to remain homebound. While there is no permanent cure for COPD, treatments and lifestyle changes typically lead to prolonged survival outcomes.

What Makes Traveling With COPD Different?
Air travel is safe and comfortable for most passengers, even those with COPD and respiratory diseases. Some COPD patients, however, may be at more risk for travel-related symptoms than others. Fortunately, these individuals can be identified with proper screening and pre-flight assessment.
There remains, however, a need for a clear consensus surrounding altitude simulation tests and assessments for in-flight hypoxemia. According to a North American study that reported on a cohort of 100 COPD patients, those that forgo air travel have a lower mean forced expiratory volume in 1 second (FEV1), which suggests that patients with severe COPD choose not to travel by air
Airlines need to identify which individuals are likely to develop moderate to severe respiratory symptoms during air travel — hence the practice of pre-flight assessment.
There are three methods for this assessment:
- The first method consists of asking passengers whether they can accomplish a 50-meter walk test. If the answer is yes, then they are probably fit to fly.
- The second method applies several prediction equations developed from studies involving COPD patients that are exposed to a normobaric or hypobaric hypoxic environment. These studies typically measure arterial blood gas (ABG) tensions as an indicator of a passenger's fitness to fly..
- The third method involves the hypoxic challenge test. This test utilizes the oxygen saturation measured by pulse oximetry to identify passengers that will need in-flight supplemental oxygen.

10 COPD Travel Tips for Air Travel
Flying with COPD can be pretty challenging, especially if it's your first time. Whether you're traveling for leisure, business, or treatment, adequate preparation and planning are essential to ensure a safe and comfortable trip.
Before you can even pack your bags and walk out the front door, consider these ten air travel tips:
1. Schedule An Appointment With Your Doctor
Before booking a flight, talk to your healthcare provider about your travel plans. Specifically, make sure to ask them these essential questions :
- Will it be safe for you to travel?
- When traveling at a high altitude, will your oxygen requirements change?
- Are there any potential changes in your medications you need to consider?
2. Never Forget Your Medical Records
Ask your doctor for a copy of your medical records at your appointment. You can also ask them for a summary of your case. It will be helpful during emergencies so that any medical professional unfamiliar with your history can better understand how to treat you.
3. Avoid Travelling Alone
For severe cases of COPD, especially those with comorbidities like cardiac disease, it's advisable to travel with someone — whether it's a significant other, a relative, or a friend. If you fall ill during the flight, your travel companion should be equipped to answer relevant questions about your medical condition and history.
4. Stock Up on Your Meds
Nothing could be worse than leaving home to travel thousands of kilometers away only to realize that you’ve run out of medication halfway through the trip. To avoid this calamity, stock up on all your essential medicines before the day of your flight.
5. Travel With Oxygen
If you're flying to your destination, note that an airplane's cabin is pressurized to withstand high altitudes. This means that the air inside the cabin will contain less oxygen than average during a flight. As a result, the risk factors for COPD patients increase.
If you need in-flight oxygen, travel with a reliable oxygen concentrator. If you're traveling with an oxygen unit, inform the airline weeks before the day of your flight.
6. Work With the Accommodation In Your Destination
Tell them about your oxygen needs if you have accommodations at your destination, like a hotel. Inform them that you will bring it with you or that someone will deliver the equipment.
7. Check The Battery Power
If you're using a portable oxygen concentrator unit, ensure you have enough batteries. The unit must last from the first take-off to the final landing. Carry excess batteries with you in case of delays or layovers.
8. Plan the Medical Care At Your Destination
If you're traveling to a new destination, ask your healthcare provider to recommend a local doctor or hospital you can use in the case of emergencies. Get their phone number and address and add that information to your medical folder.
9. Consider Using A Wheelchair
When you're making travel reservations, consider asking for a wheelchair. The walk from your gate to the aircraft might be long, and you need to preserve the batteries of your POC. The security check-in might also be a long wait, so having a wheelchair comes in handy.
10. Arrive Early
Flight hindrances are common when traveling, especially when medical equipment must be accommodated.. Arrive a few hours early for your flight so you have enough time to clear your medical needs and equipment.

10 COPD Travel Tips for Ship Travel
Of course, air travel isn't the only transportation there is. If you're traveling by ship or cruise, there's an entirely different set of requirements you must consider if you're traveling with COPD. Here are some practical tips to make it easier for you:
1. Be Mindful of the Weather
Weather changes can cause COPD symptoms to become worse. If your destination has cold weather, make sure that you pack warm clothing. Wear a face mask or scarf so you won't inhale allergens or dust.
2. Inform the Cruise Line Weeks Before The Departure Date
While many cruise lines allow their passengers to travel with oxygen units, it doesn't mean you can show up with one. Inform the cruise line four to six weeks before the scheduled departure date to ensure they approve it.
3. Stay Up To Date With Vaccinations
If you're traveling, check the Centers for Disease Control and Prevention (CDC) for the necessary vaccinations. They offer a worldwide (A to Z) map that includes the travel requirements for each country. If you're not traveling internationally, consider getting a flu shot.
4. Reduce The Risk Of Infection
Traveling on a cruise ship increases risk factors related to lung infection. To avoid placing yourself at high risk, consider doing a few of these things:
- Avoid coffee, alcohol, and tea
- Drink plenty of water
- Wash your hands frequently and bring along a hand sanitizer
- Consider wearing a face mask to avoid inhaling any airborne droplets and particles
- Bring prescribed antibiotics with you
5. Make Sure That Everything Is Ready
Usually, you will need to make the arrangements for oxygen by yourself. Bring your portable oxygen concentrator or other oxygen units with you. Also, bring a copy of your medical records in case of emergencies.
6. Get A Letter From your Healthcare Provider
A letter from your doctor or healthcare provider stating you are approved and fit for travel is required by some cruise lines. The letter should include a list of your medications and oxygen needs.
7. Request A Smoke-Free Area
When booking a hotel in your destination or a room on the cruise ship, make sure to request a non-smoking one to avoid breathing in smoke during your stay or travel.
8.Eat Healthy and Exercise
Of course, one essential travel tip is to take care of yourself. Do so before, during, and after the trip. It means you need to eat healthy food and exercise regularly to strengthen your physical body. It will also help lessen fatigue, increase your energy, and boost your mood for the trip.
9. Get Enough Rest
Remember to pace yourself. Take the time to get enough rest before and during the trip. Restore your energy so that you will get all the exciting plans!
10. Don't Travel Alone
You need a travel partner, not just for your safety and well-being, but also as a companion. It ensures that someone nearby knows about your medical needs and is ready to step in when needed.

What Are The Things You Should Take When You Travel With COPD?
To make traveling with COPD easier, prepare a checklist of all supplies and things you need. Doing so will save you from constantly worrying if you forgot something or scrambling to pack everything before leaving.
Here are the most vital things you need to take with you when you are traveling with COPD:
- Nasal Cannulas
- Oxygen Tank or POC units
- Medications
- Hand Sanitizers
- Extra Tubing
FAQs About Traveling With COPD
Can people with copd travel in an rv.
Yes, as long as they have everything they need to maintain and sustain their oxygen therapy, they can travel in an RV.
Can I get Travel Insurance with COPD?
Yes. Once you declare that you have COPD, you can compare a wide range of quotes for special COPD travel insurance policies.
Can you Travel Abroad with COPD?
Yes. People with COPD can indeed travel abroad. You can travel safely and comfortably if you comply with your airline's oxygen-related requirements.
Is it Safe for Someone with COPD to Travel to High Elevations?
Traveling with high elevations of 10,000 ft or higher should be avoided by people with COPD, especially those with severe conditions.
5. Cost of Travel Insurance with COPD
It typically depends on what the travel insurance covers. These costs vary from insurance to insurance, so it is best to reach out and discuss with your insurance company to know the specific answer.

Travelling With COPD Is Easier With Reliable Portable Oxygen Concentrators
When you prepare correctly, traveling with COPD can be hassle-free and stress-free! Regardless of what type of travel you are planning — whether it's venturing the sky or sailing the seas — planning will save you time. Ensure that you follow all the requirements and are ready to go!
References:
- Ergan B, Akgun M, Pacilli AMG, Nava S. Should I stay or should I go? COPD and Air Travel, European Respiratory Society. European Respiratory Society. Available at: https://err.ersjournals.com/content/27/148/180030
- What is COPD? National Heart Lung and Blood Institute. U.S. Department of Health and Human Services. Accessed: November 21, 2022 https://www.nhlbi.nih.gov/health/copd
- Johnson, A.O.C. (2003) Chronic obstructive pulmonary disease. 11: Fitness to fly with COPD, Thorax. BMJ Publishing Group Ltd. Available at: https://thorax.bmj.com/content/58/8/729 (Accessed: November 21, 2022)
- Deborah Leader, R.N. (2022) Traveling with COPD: Tips to make your trip a success, Verywell Health. Verywell Health. Available at: https://www.verywellhealth.com/traveling-with-copd-914970 (Accessed: November 21, 2022).
- Traveling with COPD. COPD Foundation. Available at: https://www.copdfoundation.org/Learn-More/I-am-a-Person-with-COPD/Traveling-with-COPD.aspx (Accessed: November 21, 2022).
- What it takes to travel with COPD. WebMD. Available at: https://blogs.webmd.com/copd/20210921/what-it-takes-to-travel-with-copd (Accessed: November 21, 2022).
Written by Andy Flynn
Medically reviewed by aaron gravely, m.d., leave a comment.
Comments must be approved before appearing
* Required fields
- Oxygen Concentrators
- Privacy Policy
- Terms of Service
- Refund Policy
- SpryLyfe Blog
Portable Oxygen Concentrators
- SeQual Eclipse 5
BBB Accredited Business

Copyright © 2024 SpryLyfe.
Empire Theme by Pixel Union .
- American Express
Added to your cart:
You are using an outdated browser. Please upgrade your browser .
- Moscow Tours
Our 20 Best Moscow Tours of 2022
Join us on an unforgettable tour to Moscow, the capital of Russia. Imagine visiting Red Square, St. Basil’s the Kremlin and more. Moscow is one of Europe’s most vibrant cities and one of Russia’s most historical. All of our tours to Moscow are fully customizable and can be adjusted to fit any budget. Our most popular tours are listed below. Please click on the tour details to learn more or contact us for more information about our Moscow tours using the form at the side of the page. You can also schedule a call with one of our Russian travel specialists to learn more.

Classic Moscow
This is our most popular Moscow tour that includes all the most prominent sights. You will become acquainted with ancient Russia in the Kremlin, admire Russian art in the Tretyakov Gallery, listen to street musicians as you stroll along the Old Arbat street, and learn about Soviet times on the Moscow Metro tour.
Accommodation
PRIVATE TOUR

A Week in Moscow
This tour is a perfect choice for those who wish to get to know Moscow in depth. One of the highlights of this package is the KGB history tour which gives an interesting perspective on the Cold War. You will also have time for exploring the city on your own or doing extra sightseeing.

Weekend in Moscow
This tour is a great way to get acquainted with the capital of Russia if you are short of time. You will see all the main attractions of the city, the most important of which is the Kremlin - the heart of Russia. The tour starts on Friday and can be combined with a business trip.

Group Tour Moscow Break by Intourist
Russia's capital has so much to offer, from the Kremlin and the Metro to the Old Arbat street and the Tretyakov Gallery. Besides these sites, you will also visit a fascinating country estate which today is quite off the beaten path, Gorky Estate, where the Soviet leader Lenin spent the last months of his life.

Kolomenskoye Tour with transport
The history of Kolomenskoye stretches back for centuries. In 1380, Dmitri Donskoi’s army passed through Kolomenskoye on their way to the Kulikovo battlefield, and it was...
Tours by car

Kremlin, Red Sq., Cathedrals & Armory Tour
The Kremlin is truly a fascinating structure, at the same time it is an ancient tower, the city’s former military fortification, a palace, an armory, the sovereign treasury...
Walking tours

Kremlin, Red Sq., Cathedrals, Armory, Diamond Fund Tour

Old Arbat walking tour
You will be told of the street’s interesting history and view the street’s artisan culture. You will also have the opportunity to view and purchase souvenirs from the...

Tour to Sergiev Posad with transport
Considered by some to be the Russian Vatican, Sergiev Posad is the temporary residence of the Patriarch of the Russian Orthodox Church. The Trinity St. Sergius Monastery (Lavra)...

Tour to Kuskovo with transport
The Kuskovo Estate often called the Moscow Versailles due to its perfectly preserved French park, is an example of an 18th century, luxurious Moscow summer residence. Its history...

Tour to Tsaritsyno with transport
The Tsaritsyno Estate is located in the southern part of Moscow. The estate was constructed for Catherine the Great by the Russian architects Bazhenov and Kazakov in a romantic...

Moscow Metro and Old Arbat Tour
The Moscow Metro is one of the largest and most grandly built metro systems in the world. It was meant to be a showcase of the Soviet Union’s achievements for both the Russians...

Vodka Museum Tour with transport (excursion and vodka tasting)
Vodka is an important component of Russian life, an element of national identity and everyday culture. We invite you to visit the Vodka Museum and feel the atmosphere of long-gone...

Mikhail Bulgakov Apartment Museum
This apartment museum located close to Patriarch Ponds became the prototype of the "bad apartment" described in the novel "The Master and Margarita." Currently the museum's...

Kremlin, Red Sq., Cathedrals & Diamond Fund Tour
The State Museum of Lev Tolstoy Tour
Take this opportunity to learn more about the Russian writer Lev Tolstoy. During the visit to the museum you will see part of a vast collection of exhibits connected to Tolstoy...

Novodevichy Convent Tour with transport
Tour of the Novodevichy Monastery. Founded in 1524 by Grand Prince VasiliIoanovich, the original convent was enclosed by fortified walls and contained 12 towers. The structure...

City Tour with Visit to St. Basils & Red Sq. with transport
Panoramic City Tour. This Moscow tour is a great start to your trip and the best way to get acquainted with many of the city’s major highlights. Our professional guide will...

City Tour of Moscow
Head to the heart of Moscow with a professional guide on a 4-hour private walk through the city center. See Tverskaya and Old Arbat streets, Theatre Square with the world-famous...

Moscow Metro walking tour

Kremlin, Red Square and Cathedrals Tour

KGB Tour with transport
This is a very interesting and insightful tour. You will visit places connected with Stalin’s terror - a time of great repression and fear. You will be shown monuments to...

Soviet and Post-Soviet Moscow Tour
The tour begins with a drive or walk down Tverskaya Street – a Soviet masterpiece. In the years of Soviet power, Tverskaya began to undergo a transformation: it was widened...

Tretyakov State Gallery Tour
This world-famous gallery contains masterpieces of Russian art beginning in the 10th century up until today. You will view exquisite Russian icons and paintings from the 18th and...

Jewish Heritage of Moscow Tour
This tour offers a detailed look into the history and present-day life of the Jewish community of Moscow. On the tour, you will visit sites connected with the cultural and religious...

Vodka Museum Tour with transport (excursion only)

Lena, our guide in Moscow was excellent. She was very knowledgable and could answer any question we had for her. We liked that she could pick up on our interests and take us places we might not have thought of to go. When we realized that one of the places we had chosen to see would probably not be that interesting to us, she was able to arrange entry to the Diamond Fund and the Armoury for us. Riding the Metro with Lena was a real adventure and a lot of fun. In Saint Petersburg we found Anna well versed in the history of the Tsars and in the Hermitage collection. Arkady in Veliky Novgorod was a very good guide and answered all of our questions with ease. Novgorod was perhaps a long way to go for a day trip, but we did enjoy it. Vasily was a great driver to have and kept us safe with good humour and skill. We enjoyed ourselves so much, my daughter says she is already planning to return. We would both have no hesistation to recommend ExpresstoRussia to anyone we know.
Just wanted to let you know that My grandson Bruno and I couldn´t have been more pleased with our week in Moscow (6/15 - 6/21). We were absolutely enchanted with the whole experience, including getting lost a couple of times in the Metro during our free time. Although both our guides (both Eleanas) were excellent, I would particularly commend the first one (she took us to the Tatiakov, the KGB tour, and to that beautiful cemetery where so many great Russian artists, authors, composers, musicians, militarists, and politicians are buried). Her knowledge is encyclopedic; and her understanding of today´s Russia as a product of its past was, for us, truly enlightening. I will be taking another tour in Russia, with my wife, within the next two or three years. I will be in touch with you when the time comes. Meanwhile, I will refer you to other potential visitors to Russia as I meet them.
Tours to Moscow
Our Moscow tours are land only meaning that you arrange your own air travel to Russia and our expert staff meets you at the airport and handles everything else from there. Our online Airline Ticket booking system offers some of the most competitive rates to Russia available on the web so if you need tickets, please visit our Russian air ticket center . Rest assured that you will be taken great care of on one of our Moscow tours. Express to Russia has a fully staffed office in Moscow that will help to make your visit fun, informative and unforgettable. Please remember that of all these tours are private and can be adjusted to your taste. You can add, replace or skip some sights; you can add more days to the package or cut the tour short. Our specialists will be glad to help you create the tour of your dreams!

Moscow, a City Like No Other
Moscow is Russia’s largest city with a population of between 12 and 13 million. It is also Europe’s largest city and when you visit Moscow, you can feel it. The layout and architecture of the city is eclectic, ranging from crooked, ancient streets and alleyways to wide, bustling boulevards, from medieval churches to Stalin skyscrapers and to modern, glass buildings towering over everything and of course in the center of it all is the Kremlin and the magnificent Red Square. Moscow is also home to a fantastic, efficient and very beautiful metro system – each station having its own special design. In fact, Express to Russia’s Moscow metro tours and excursions are some of our most popular attractions that we offer. On our Moscow tours, you will see this and more.

Moscow Tours centering on Russian History
Moscow has a long and interesting history and has been the capital of Russia in many of its different iterations – capital of the Grand Duchy of Moscow , the Russian Empire and of course the Soviet Union (who could ever forget the Soviet Union?). Moscow, was founded in the 12th century by Prince Yuri Dolgaruki (Yuri of the long arms – he really did have long arms!). From that time on, it was home to the Russian Tsars until Peter the Great moved the capital to St. Petersburg in 1703. The city has survived invasions and sieges from the Mongols, the Tartars, the Poles, Lithuanians and Napoleon but has always persevered. Our Moscow tours will enlighten you on this great history and give you insights into Muscovites and their unique culture. Our Moscow tours show you what the city is like today but also brings to life the past. Moscow never seems to sleep and is bursting with energy. A Moscow tour with Express to Russia is truly the best way of getting to know Russia’s largest and most vibrant city.
Frequently Asked Questions From Our Travelers
What is the best time to visit moscow.
Any time of year is fine depending on what you plan to do. Summertime is pleasantly warm, ideal for exploring the city and its vibrant atmosphere, but Moscow will be much busier and accommodation is more expensive. Winter can be quite cold but beautiful nonetheless, and this is unproblematic if you intend to spend most of your trip in museums and galleries. There are also various festivals and events organised throughout the year. For more information about the best time to visit, read our guide
How many days are enough in Moscow?
If you plan your itinerary strategically and aren’t averse to a packed schedule, you can cover Moscow’s main sights over a long weekend. Most popular attractions are in the city centre, and the Moscow Metro allows you to cover much ground in a small amount of time. Ensure that your accommodation is fairly central and book tickets in advance, so that you can make the most of your days. For an informative and well-organised day out, check out our Moscow day tours with options to suit all interests.
Do they speak English in Moscow?
As Russia’s capital city, tourists are well accommodated in Moscow. There should be English-speaking staff in restaurants, bars, hotels, shops and attractions in tourist hotspots, and there are also English-speaking tourist police. Transport services have English translations on their maps and English announcements via intercom; alternatively, order taxis from the Yandex Taxi app (Russian Uber), though it’s unlikely that your taxi driver will speak English. If you get stuck and cannot communicate, it’s fine to use Google Translate.
Is it safe to travel to Moscow?
It is no less safe to travel to Moscow than to any European city if you exercise common sense and look after your belongings. As with every city some regions can be more unsavoury than others, but no tourist attractions are located there. The traffic in Moscow is notorious, so exercise caution when crossing roads. Do not take unlicensed taxis; book in advance or take public transport, which is widespread and perfectly safe. If you encounter any problems, look for the special tourist police who can help you. For more information, read our guide about staying safe in Russia .
Our travel brands include

Express to Russia
Join us on Facebook
We invite you to become a fan of our company on Facebook and read Russian news and travel stories. To become a fan, click here .
Join our own Russian Travel, Culture and Literature Club on Facebook. The club was created to be a place for everyone with an interest in Russia to get to know each other and share experiences, stories, pictures and advice. To join our club, please follow this link .
We use cookies to improve your experience on our Website, and to facilitate providing you with services available through our Website. To opt out of non-essential cookies, please click here . By continuing to use our Website, you accept our use of cookies, the terms of our Privacy Policy and Terms of Service . I agree
- United Arab Emirates
- Switzerland
- The Netherlands
- Puerto Rico
- United States
- New Zealand
- ➨ Choose from World Map
- Budget Travel
- Family Travel
- Getting Around
- Visas & Passports
- Work with Us
Browsing Category
- Czech Republic
- Saint Martin
- Uncategorized
Moscow Travel Guide: Best Things to Do + More [2023]
· everything to know about visiting moscow, including the best things to do and how to get around. ·.
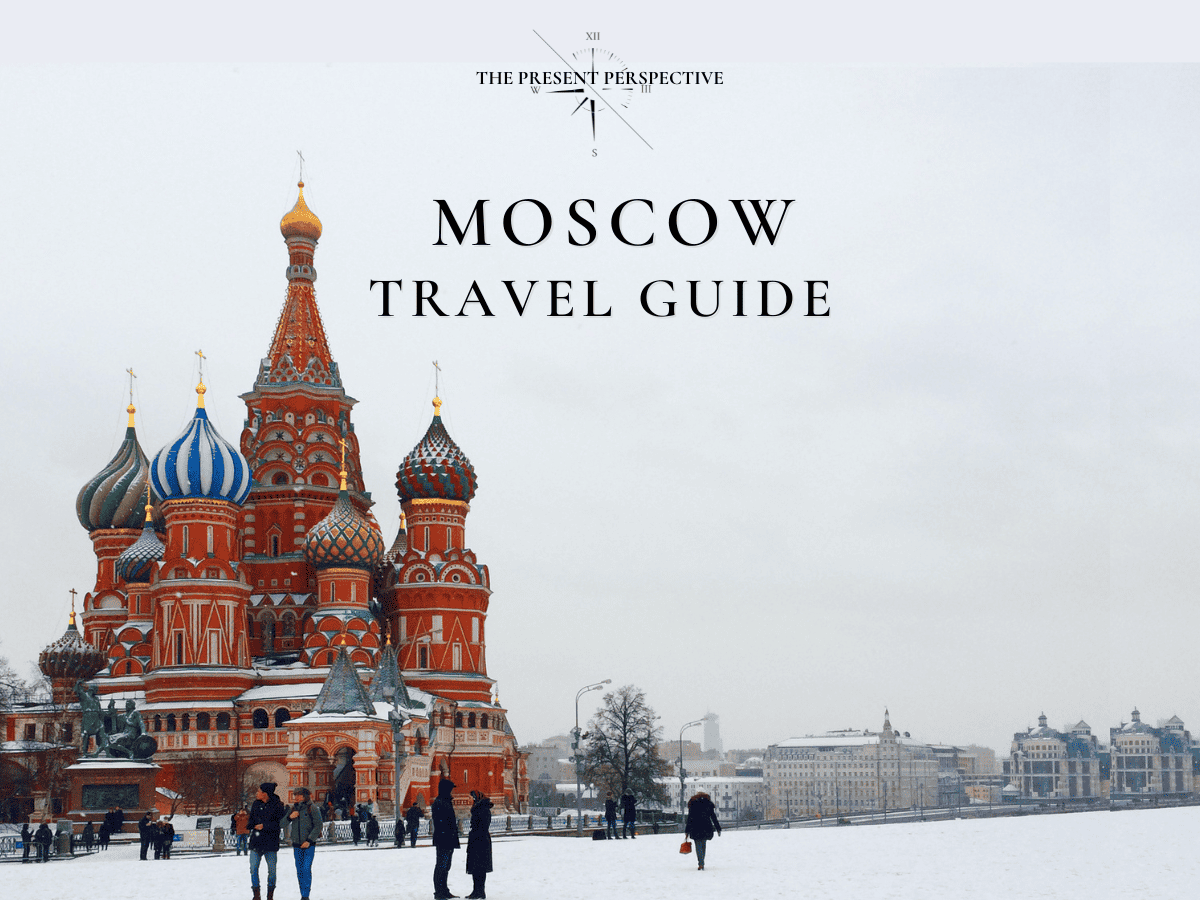
Moscow is Russia’s vibrant capital city, and it also happens to be the largest city in all of Europe. The city’s long and infamous history makes it one of the most unique places we have ever visited.
The architecture ranges from centuries-old palaces to uniform, gray concrete buildings. The people range from cold and private to warm and welcoming. Moscow is a city is strong juxtapositions, and we learned a lot during our time there.
This post will break down all you need to know about visiting Moscow, including the best things to do, how to get there, how to get around, and more.

The Best Things to Do in Moscow
1. explore the red square.
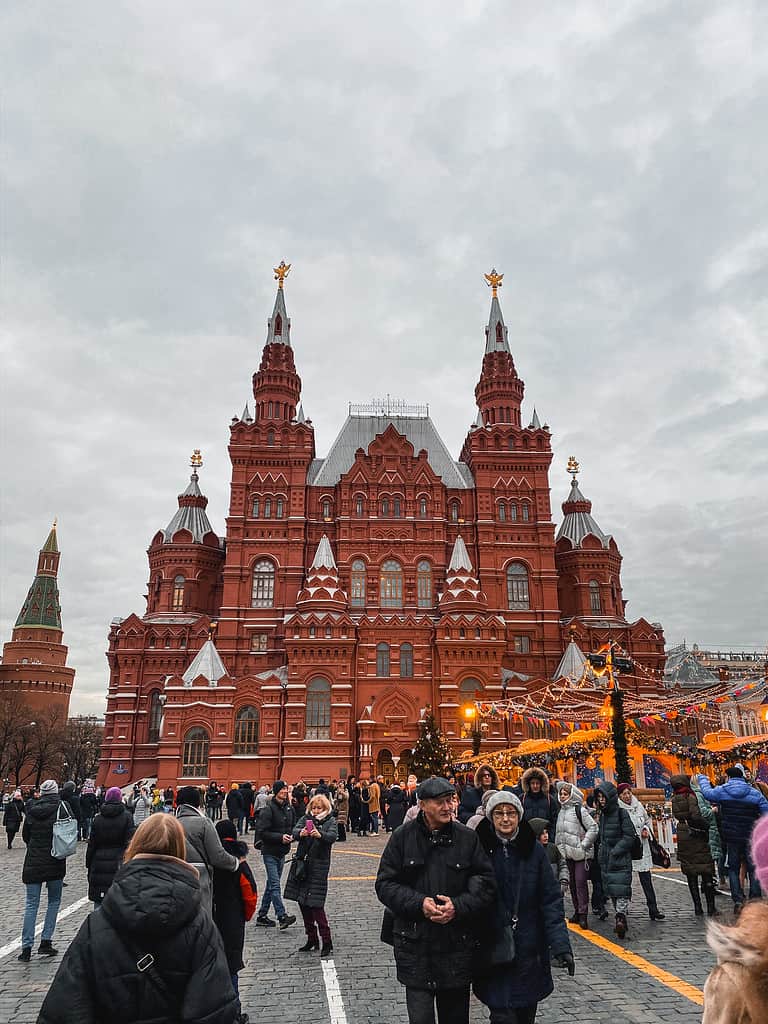
The Red Square is the heart of Moscow. Most of the city’s top attractions can be found here, including just about everything on this list. The Kremlin, St. Basil’s Cathedral, and Lenin’s Mausoleum are all located here, and the State Historical Museum and GUM are not far from here, either.
The Red Square is a common home for parades, protests, and seasonal celebrations. There are massive Christmas celebrations here, with food vendors and carnival rides set up in numbers.
2. Check Out the Ziferblat
The Ziferblat is a café in Moscow that is unlike any café we have ever been to. While most cafes charge you for your drinks and food, the Ziferblat charges you for your time.
Upon arrival, you are given a clock. When you leave, the barista calculates how much time you spent in the café and charges you accordingly. This concept was created to help visitors to be more intentional with their time, and the cafe itself is incredibly charming.
For a detailed look at everything you need to know before you visit, make sure you read my post about visiting the Ziferblat Cafe in Moscow .

3. Marvel at St. Basil’s Cathedral
St. Basil’s Cathedral is one of the most iconic churches in the world, and it was the single thing we were most excited to see while in Moscow. Built almost 500 years ago, St. Basil’s Cathedral is recognized by its colorful domes and whimsical style. The church is of the Russian Orthodox faith, and the inside is just as wondrous as the outside.
St. Basil’s Cathedral is located on the edge of the Red Square, making it incredibly convenient to visit. Entrance for non-worshippers costs 800 rubles, and tickets can be bought at the church

4. Explore the Kremlin
The Kremlin is the largest active fortress in Europe, and it is the site of most of Russia’s government affairs. In addition to government buildings, the Kremlin Complex is filled with courtyards, towers, and museums that are open to the public. If you have the time, you could spend a couple of days fully exploring all that there is to see in the Kremlin.

5. Walk Through Lenin’s Mausoleum
Vladimir Lenin is one of the most important figures in Russian history, and his body is located perfectly embalmed in a mausoleum in the Red Square. The Mausoleum is open to the public to visit, and as long as you are willing to go through a few security checks, it is easily one of the best things to do in Moscow. Its convenient location in the Red Square makes it a can’t miss attraction.
There is absolutely no photography allowed inside the Mausoleum. Do not test this rule.

6. Wander Along Arbat Street
The Arbat is a very popular street in Moscow that is lined with stores, cafes, and other touristy attractions. It is one of the oldest streets in the city, dating back to the 1400s. This street is both quaint and trendy, and there are many walking tours that introduce tourists to the neighborhood’s wonders and highlights.

7. Catch a Show at the Bolshoi Theatre
As a lover of the arts, it is hard to think of Moscow and not think of ballet. Russia has always been a top dog in the world of fine arts, and Bolshoi Theater is one of the best places to catch a performance. We were lucky enough to attend an Opera here, and it is a venue that you don’t want to miss out on if you enjoy opera, ballet, or orchestral performances.
8. Visit the State Historical Museum
The State Historical Museum is one of the most respected museums in Moscow. Despite its name, it is not really focused on the history of Russia as a nation. Rather, it contains a collection of artifacts from all throughout Russia’s history.
The museum’s collection is very broad in nature. It houses some items from indigenous tribes that used to occupy the region, pieces collected by the Romanov family, and more.
9. Wander Around GUM
GUM is an absolutely massive mall within walking distance of the Red Square. It isn’t just the size that draws visitors here; it’s the sense of luxury. The mall is so beautiful inside, much like the metro stations.
While visiting a mall might not sound like it belongs on a bucket list, this mall does. You will not want to miss out on visiting GUM while in Moscow.

10. Admire the Cathedral of Christ the Saviour
While St. Basil’s Cathedral is the most iconic church in Moscow, it isn’t the only one. The Cathedral of Christ the Saviour is absolutely stunning, with massive golden domes. It is the tallest Orthodox church in the world, and it is the seat of the Orthodox Patriarch of Moscow.
It is located just about a mile from the Red Square, just south of the Kremlin Complex. You can walk to it from the Red Square in about 20 minutes.
How to Get to Moscow
Flying to moscow.
Moscow has three major international airports: Sheremetyevo (SVO) , Domodedovo (DMO) , and Vnukovo (VKO) . All three of them are directly connected to downtown Moscow by the Aeroexpress trains, which leave every 30 minutes throughout the day. By Aeroexpress train, you can expect to get to the city center in 25-45 minutes depending on the airport that you fly into.
Sheremetyevo is the biggest and busiest of the three airports, and it is the one you are most likely to fly into – especially if you are coming from outside of Europe or the Caucus region. We flew into Sheremetyevo on a direct flight from New York City.
I usually provide backup airport options, because flying right into the city isn’t always the cheapest way to get where you’re going. Unfortunately, when it comes to Moscow, don’t really have a choice other than to fly right into Moscow. It is a very remote city, and it is usually the cheapest place to fly into in Russia as a whole.
Since Sheremetyevo is so busy, you will probably find a great flight option anyway. I wrote in my post about finding cheap flights that using hub airports will lead to more affordable airfare, and the same logic applies here. Even though Russia’s national airline, Aeroflot, is no longer a member of the SkyTeam Alliance, Moscow is still a major hub connecting passengers from all over the world.

READ OUR CHEAT SHEET
Train or Bus to Moscow
Trains and buses are one of the most popular ways to get around Europe. However, they’re of very little use when you’re trying to get to Moscow.
Moscow is hundreds of miles from the nearest major cities. The only major European city that can even be reached within 8 hours on the ground is St. Petersburg, and even the Baltic capitals of Riga, Vilnius, and Tallinn are over 12 hours away.
If you want to get to Moscow, the best option is almost always to fly. While the train routes to Moscow are scenic, they simply take forever.
How to Get Around Moscow
METRO | TROLLEYS | TRAMS | BUSES
Moscow has one of the most memorable metro systems in the world. Its metro lines are very deep underground, and the stations are absolutely stunning. Each station has its own unique style, but all of them contain escalators that seem to go on forever.

The system was built in an effort to showcase the power of the Soviet Union and its bright future. The plans were a form of propaganda, but they resulted in what is still one of the most visually appealing subway systems on earth.
Moscow’s metro system isn’t just pretty. It is also very useful and accessible. The system has 17 lines that connect the city and its surrounding area.
But wait; there’s more!
The Moscow metro system is also incredibly affordable, with each ride costing less than a dollar. The metro is by far the best way to get around Moscow, as it is almost impossible to beat the connection times and the low cost to ride.
Tickets can be bought at electronic, English-speaking kiosks in stations, or directly from ticket counters at certain larger stations. There are also day passes available, which are a very solid option if you plan on riding the metro several times per day.

The metro is by far the best way to get around Moscow.
In addition to the metro system, Moscow also has a network of buses, trams, and trolleys. This system is nowhere near as convenient or well-connected as the metro, though, and is likely of little use to you during your trip. There is no Uber in Moscow, but a similar app named Yandex is available if you need a ride in a pinch.
How Many Days Do You Need in Moscow?
Moscow is the biggest city in all of Europe, and it is absolutely loaded with things to do. You could spend weeks in Moscow and still find new things to do. Of course, most travelers don’t have that kind of time to spend in one place!
I recommend spending no less than three full days in Moscow, and ideally closer to five or seven.
Moscow is very spread out, and it can take some time to get from one major point to another. There are also so many places that are nice to just sit back and relax, which is hard to do when you’re in a hurry trying to cram activities into just a few days.
If you only have a week to visit Russia, I’d advise spending all of the time in one city. If you decide to split your time between Moscow and St. Petersburg, I recommend not trying to squeeze in any day trips beyond those two cities.

When Is the Best Time of the Year to Visit Moscow?
There are two different ways to approach this question. Personally, I think the best time to visit Moscow is around Christmas and New Year’s Day. While the weather will be absolutely freezing, Moscow is a surreal winter wonderland in December and January.
We were in Moscow right before Christmas. While it was very cold, you can always bundle up. Exploring the Christmas markets and pop-up ice skating rinks throughout Moscow is one of my favorite memories from anywhere I’ve traveled, and I dream of going back to do it again.
If you aren’t fond of the cold, Moscow is beautiful in the summer. It tends to get pretty cold in the shoulder seasons, so if you want warm weather, you should plan to visit in the summer. Moscow actually gets pretty warm in July and August, and there are a bunch of fantastic places to soak up the sun within the city.
The best time to visit Moscow is either around Christmas or from late May to August.

Is Moscow Safe to Visit?
While Moscow is a truly wonderful city, there’s no denying that visiting Russia comes with risks. As the country is run by an infamous communist dictator, concerns about visiting are valid. While we didn’t experience any sort of threat or negative treatment during our time in Moscow, we visited in a peaceful time.
In our experience, Russia doesn’t seem to detain normal Americans or Westerners to use as pawns. As a regular person, as long as you don’t commit any crimes, there is a slim chance you will run into any issues. However, Russia will not hesitate to enforce its laws against foreigners, and illegal behaviors will likely land you in a very compromising position.
Russia will not hesitate to enforce its laws against foreigners, and illegal behaviors will likely land you in a very compromising position.
To make matters worse, Russia has a bad reputation for gang violence. While the Russian mafia has very little interest in normal Western tourists, they won’t hesitate to pick a fight with anyone who ventures into their sphere of influence. If you seek out illegal substances or activities, you could be a target of the mafia.
If you seek out illegal substances or activities, you could be a target of the mafia.
Finally, since Russia’s invasion of Ukraine, things are all very different. Russia is currently at war, and there are battles raging within 8 hours of Moscow. While it is still relatively safe to visit, that could change at any time as the war with Ukraine continues.
Is Moscow Worth Visiting?
Without a doubt, Moscow is worth visiting. It is one of the most unique major cities we have ever visited, and we hope to make it back one day. The Russian Orthodox churches are stunning, the city’s history is unlike any other, and the food is to die for.
While many visitors prefer St. Petersburg to Moscow, I think Moscow deserves a lot of hype of its own. Moscow is the beating heart of Russian culture and history, and it’s a place I highly recommend checking out if you have the chance.

That’s all we have for you about Moscow! I hope this post was helpful as you plan your trip to Russia’s capital.
Have you been to Moscow? Or is this your first time visiting? Comment below if you have anything to add to our travel guide!
Hi, I'm Greg. I'm an avid traveler who has traveled to over 50 countries all around the world with my wife and kids. I've lived in Italy, Mexico, China, and the United States, and I dream of moving abroad again in the future. With this blog, I provide my audience with detailed destination guides to my favorite places and pro-tips to make travel as stress-free as possible.
Leave a comment
Save my name, email, and website in this browser for the next time I comment.
Meet The Author - Greg

Recent Post

How Much Does a Trip to Egypt Cost: Budget Breakdown
March 10, 2024

Best Time to Visit the India Gate in Delhi [2024]
March 1, 2024

Flying with a Sinus Infection: Tips to Avoid Pain
February 20, 2024

11 Best Things to Do in Breckenridge Besides Skiing
February 12, 2024

10 Best Beaches in Mexico for Families (We Lived Here)
February 3, 2024

IMAGES
VIDEO
COMMENTS
This means there is less oxygen in the plane during a flight. This is not usually a problem for people with healthy lungs, but it can cause people with COPD to be at risk of having low oxygen levels. If you need oxygen during exercise or sleep, you may also need it for air travel.
Dr Khabbaza: Air travel subjects patients with COPD to lower oxygen pressures in the cabin, which is similar to breathing about 15% oxygen at sea level. 1 Patients with COPD have a lower respiratory reserve and are at a higher risk of developing hypoxemia during air travel. Additionally, patients with chronic hypoxemia requiring continuous ...
A liquid oxygen unit contains oxygen gas cooled to a very low temperature. Most tanks come with a portable unit that you can carry or pull on a cart. A portable oxygen concentrator (POC) takes in the air around you to concentrate oxygen and give you more of it. It uses electricity from a battery or by plugging into an outlet.
This means there is less oxygen in the cabin air during a flight . This may cause some people with COPD to feel short of breath, dizzy, or tired . Some people with COPD may need to use oxygen during their flight . Studies show that if your oxygen level is 95% or above, you will not need supplemental oxygen during air travel .
Each airline has their own policies and procedures for traveling with oxygen. If traveling by car or train, you might need to arrange both portable and a more long-lasting oxygen supply. These arrangements can be discussed with your oxygen supplier. DO be aware that high altitudes, whether flying or just driving in the mountains, can increase ...
Depending on your method of transportation for your trip, you'll want to check with your specific company about any rules, regulations or procedures they have, especially if you're traveling with COPD and supplemental oxygen. Air Travel: Contact your airline a few weeks ahead of your departure date, regarding its policies on oxygen.
Chronic obstructive pulmonary disease (COPD) is a challenging respiratory problem throughout the world. Although survival is prolonged with new therapies and better management, the magnitude of the burden resulting from moderate-to-severe disease is increasing. One of the major aims of the disease management is to try to break the vicious cycle of patients being homebound and to promote an ...
As you prepare for a trip with supplemental oxygen, check that your equipment and devices are permitted for use during your travel and at your destination. Be sure to ask whether you will have space and be afforded accommodations to use your device. Prepare for your travels by bringing batteries or chargers to power your equipment.
Chronic obstructive pulmonary disease (COPD) is a preventable disease that is characterised by airflow limitation. ... can be found in the European Federation of Allergy and Airways Diseases Patients' Association booklet on enabling air travel with oxygen in Europe . Patients receiving long-term oxygen therapy can take their own cylinders if ...
In-flight oxygen is usually prescribed at a rate of 2-4L/min and should be given by nasal cannulae. 7 This will partially reverse altitude-induced hypoxemia symptoms in patients with COPD. 11 Nowadays, many airlines allow POCs on board, but often only specific types. 7 Box 1 shows a practical guidance to help ensure safe air travel for ...
For most passengers, even those with respiratory disease, air travel is safe and comfortable. Some patients with COPD may be at risk but, with screening, these patients can be identified and most can travel safely with supplemental oxygen. A House of Lords Select Committee on Science and Technology published a report entitled "Air Travel and Health" in November 2000.1 They concluded that ...
BTS recommendations for managing passengers with stable respiratory disease planning air travel were published in Thorax in 2011.1 This followed original guidance published in 20022 and an online update in 2004.3 The 2011 recommendations provided an expert consensus view based on literature reviews, aimed at providing practical advice for lung specialists in secondary care. Recognising that ...
Overall, air travel in patients with COPD is safe and generally requires just a slight increase in oxygen delivery in patients with or without pre-travel HAST. With all the newer modes of oxygen delivery now available, studies comparing and [evaluating] their reliability during air travel may be beneficial, although I am not sure an in-flight ...
Patients with COPD may need supplemental oxygen during air travel to avoid development of severe hypoxemia. The current study evaluated whether the hypoxia-altitude simulation test (HAST), in which patients breathe 15.1% oxygen simulating aircraft conditions, can be used to establish the optimal dose of supplemental oxygen. Also, the various types of oxygen-delivery equipment allowed for air ...
Background The reduced pressure in the aircraft cabin may cause significant hypoxaemia and respiratory distress in patients with chronic obstructive pulmonary disease (COPD). Simple and reliable methods for predicting the need for supplemental oxygen during air travel have been requested. Objective To construct a pre-flight evaluation algorithm for patients with COPD. Methods In this ...
Chronic Obstructive Pulmonary Disease (COPD) is a debilitating respiratory condition that creates several lifestyle challenges for its victims. ... utilizes the oxygen saturation measured by pulse oximetry to identify passengers that will need in-flight supplemental oxygen. 10 COPD Travel Tips for Air Travel. Flying with COPD can be pretty ...
Pulmonary function testing: These tests usually involve blowing into a tube and show how well air moves in and out of your lungs. Chest X-ray and CT scan: These imaging tests look for lung damage. Alpha-1 antitrypsin test: A test for a genetic cause of COPD. Arterial blood gas (ABG): These tests check your oxygen and carbon dioxide levels.
This tour is a perfect choice for those who wish to get to know Moscow in depth. One of the highlights of this package is the KGB history tour which gives an interesting perspective on the Cold War. You will also have time for exploring the city on your own or doing extra sightseeing. $ 941 From/Per person. Details.
3. Marvel at St. Basil's Cathedral. St. Basil's Cathedral is one of the most iconic churches in the world, and it was the single thing we were most excited to see while in Moscow. Built almost 500 years ago, St. Basil's Cathedral is recognized by its colorful domes and whimsical style.
Bus line 308 runs between the bus terminal at Moscow Domodedovo Airport and metro station Domodedovskaya. The shuttle bus departs every 15 minutes between 06.00 hours and 00.00 hours, travel time is 30 to 40 minutes. During the night, the bus runs every 40 minutes. A ticket costs 150 RUB and is available from the bus driver, luggage is free of ...
With bus 817 and bus 948 you can get in 35 minutes to metro station Planernaya (northernmost station metro line 7). With bus 851 and bus 949 it takes 25 minutes to metro station Rechnoy Vokzal (northernmost station metro line 2). The price of a bus ticket is 57 RUB or 80 RUB. From both stations you can take the metro to the centre of Moscow ...