Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
The evaluation of healthy patients prior to surgery is reviewed here. Preoperative assessments for specific systems issues and surgical procedures are discussed separately:
● (See "Evaluation of cardiac risk prior to noncardiac surgery" .)
● (See "Evaluation of perioperative pulmonary risk" .)
● (See "Perioperative medication management" .)

- This Site Only
- Stanford Medical Sites
- Ways to Give
- Find a Person
- Lane Library
The Preoperative Evaluation
Key Points to Start:
* Remember, you can access Epic through the Ether website ( ether.stanford.edu ) whether on or off campus*
* If there is no Pre-op done in Epic, do a chart biopsy, look up old records, and call the patient (if necessary) to gather this important information that is vital in developing a safe and effective anesthetic plan*
*One question to always keep in mind while completing your pre-op: Is this patient optimized for surgery?*
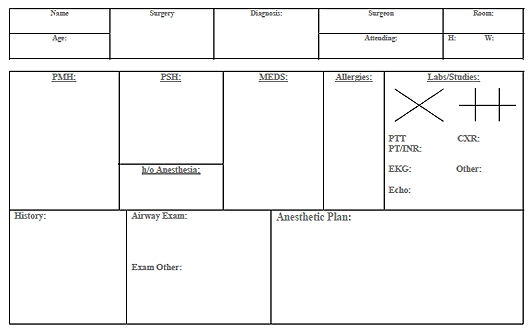
Preop Templates
Dr. Chu and Dr. Harrison talk about and simulate the Preoperative Evaluation from March START podcast
Identifying Statement
- Name, age, sex, planned surgery and indication for procedure, surgeon
Past Medical History :
Remember to list all known medical history with specific emphasis on the following:
- Hypertension (baseline blood pressures, what medications, any complications)
- Coronary artery disease (hx of MI, stents/CABG hx, recent functional studies (stress testing, cath reports, echos)
- Arrhythmias (what medications used, any implanted devices, recent symptoms, Holter tests, etc)
- COPD: (Medications used, frequency of exacerbations, steroid use, onhome oxygen, recent infections, any recent PFT information, recent CXR data if applicable)
- Asthma (Medications used, frequency of exacerbations, ever been intubated, steroid use)
- Smoking history (Pack year history, recent episodes of bronchitis, sputum production)
- Sleep apnea (may be a predictor of difficult airway)
- GERD (Medications used, degree and frequency of symptoms)
- Inflammatory bowel disease (Steroids/immunomodulators used)
- History of post-operative nausea or vomiting
- Diabetes Mellitus (Type I vs II, medications used, home fingerstick readings, last Hgb A1C, any known macro/microvascular complications)
- Thyroid disorders
- Adrenal insufficiency
- History of bleeding disorders, blood clots
- Is the patient on anticogulation medications? List any recent pertinent coagulation studies, if/when anticoagulation was reversed
- List any deficits including residual effects of old CVAs
- History of steroid use, lung/systemic involvement, any known joint (ie. atlanto- axial) instability
- ** Looking at an old anesthetic record is crucial to see if there were any airway difficulties in patients with RA!**
- Note preoperative pain score and document any history of chronic pain and list all preoperative pain medications and dosages taken by the patient (chronic opiate users may require more intra-operatively)
- List all other medical conditions
Review of Systems : Remember to be systematic and complete, with particular focus on the following:
- Constitutional : recent fevers or infections, nighttime sweating, motion sickness symptoms
- Cardiovascular : Exercise tolerance (how many stairs?), angina, activity level
* Patients who cannot meet the demand of 4-METS are high risk—Climbing a flight of stairs is 4-METs*
- Pulmonary : Shortness of breath, cough, dyspnea on exertion, smoker, use of inhalers, baseline oxygen if applicable
- Gastrointestinal : Reflux symptoms, NPO status
How long should your patient fast?
* Any case which is emergent and these guidelines cannot be followed, rapid sequence intubation is indicated*
- Heme : Easy bruising or bleeding
- Musculoskeletal : Any cervical motion instability, myalgias, range of motion of extremities
Past Surgical History
- Past surgeries and their indications, any complications, where surgeries were performed (if known)
- Any implications for your plan? (ie cervical fusion surgery may impede normal intubation positioning)
Past Anesthetic History
- Prior history of adverse reactions to anesthesia, problems with airway management, difficult IV access, prolonged emergence, post-operative nausea/vomiting
*Prior anesthesia records are an invaluable source for this kind of information—find it and use it!!*
Risk Factors for Developing PONV
Family History
- History of malignant hyperthermia, pseudocholinesterase deficiency, or any other adverse reactions
Social History
- Alcohol use: How frequent, last drink, any complications from use
- Tobacco use: Duration in pack years, when patient last smoked
- Illicit drug use: Past or present use, when patient last used
- **Consider urine toxicology screen if clinically indicated to prevent autonomic instability**
Medications
- List all medications that the patient is taking, including over the counter and herbal medications. List the most important drugs first and give doses for important medication
- Especially medications for hypertension, diabetes, opiate pain medications, and blood thinners!
- List all allergies, especially latex and antibiotics, and reactions to each allergen if known.
Preoperative Physical Examination
- Weight and height, vitals including room air saturation, and general appearance
- Airway : Includes Mallampati score, thyromental distance, cervical motion
Mallampati Scoring
- Cardiovascular : complete exam with a focus on murmurs or rubs, check for bruits
- Respiratory : complete exam with a focus on wheezes or crackles
- Neurologic : complete exam, note any deficits discovered and compare to old records
- Extremities : complete exam, note any clubbing, deformities, bruising, and gauge level of difficulty for IV access
Additional Information
- Full interpretation including rate, rhythm, and ST changes. If available, compare to old EKGs to assess changes
- Review all recent labs and if abnormal results, compare to old values to assess changes
Assessment and Developing an Anesthetic Plan
ASA Status Classification
Dr. Chu and Dr. Harrison model how to construct an anesthetic plan from March START podcast
- Consult the surgery listing to see how the surgeon booked the case—is this anesthetic option appropriate?
- Search resources in developing your plan
- Jaffe’s Anesthesiologist’s Manual of Surgical Procedures is an excellent pre/intra/post-op reference
- Consult your big sib or other colleagues to discuss your plan and inquire about other options
A talking point during your OR day could be developing your anesthetic plans for the following day’s cases!
- Define the type of anesthesia: MAC, GA, TIVA, Regional, etc
- Note what additional invasive monitors/IV access that will be required
Calling your Attending :
Dr. Chu and Dr. Harrison model how to call your attending to discuss your pre-ops from March START podcast
- You can find your Attending’s contact information here on ether , and click on “dashboard”
- Send courtesy page if no answer with short message (no patient information!) and callback number
Always come up with your own anesthetic plan before talking the case over, but be open to change and suggestions from your attending!
You are here:, current tab: 2.

Anesthesia Resources
Airway coverage, ether dashboard, paging directory, call schedules, intranet information, scheduler phone, 500p orientation, perioperative guidelines and eras pathways, resident stuff.
- 2021 Tutorial Textbook
- Resident Case Presentation and Anesthetic Planning Outline
- Self-Assessment and Feedback Form
- Setting up Room
- Quick Guide to Common Anesthesia Procedures
- Drug set up, Autonomics Recall, and Drug Reference Sheet
- Pre-Ops and Calling Your Attending
- Charting Tips
- ASA Difficult Airway
- CA-1 (July) Lecture Series
- CA-1 (Regular) Lecture Series
- CA-1 Journal Club
- Critical Events
- Computing/IT Resources
Specialty Resources
Library (majic), videos/podcasts.
- External Links
- ACGME Case Log
- Residency Program
- MSD Quality Improvement

Site Navigation:
Footer links:.
- © 2024 Stanford Medicine
- Terms of Use

ISCHEMIC DISEASE (CAD)
Practical perioperative medicine.

G U I D E T O
Preoperative evaluation, sponsored in part through a grant from perioperative medicine education, inc..
This guide is intended as a clinical resource for clinicians performing preoperative evaluations. The author has done his best to assure the information is current and based upon the available evidence. Recommendations which are based on the author's opinion only (due to contradicting or lack of evidence from the literature) are italicized or specifically noted as such. When using this guide, keep in mind that it is only a guide and that even the best evidence may not apply to every patient situation. This information is not intended to replace the advice of a healthcare provider about diagnosis, treatment, or prognosis. The author is not responsible for medical decisions that may be made based on information on this site since it is provided for informational purposes. Patients should always consult their healthcare providers before deciding on a treatment plan.

Contact: [email protected]

- Theatre Etiquette
- Hand Washing
- Scrubbing, Gowning, and Gloving
- Assisting in Theatre
- The Operation Note
- Surgical Safety
- Suture Materials
- Surgical Instruments
- Infiltration of Local Anaesthetic
- Drain Insertion
- Abscess Drainage
- Skin Lesion Excision
- Damage to Local Structures
- Acute Inflammation
- Chronic Inflammation
- Wound Healing
- Basic Wound Management
- Venepuncture
- Cannulation
- Blood Cultures
- Intravenous Infusions
- Female Catheterisation
- Male Catheterisation
- Pre-Op Assessment
- Pre-Op Management
- Fluid Management
- Blood Products
- Perioperative Nutrition
- Enhanced Recovery
- Day Case Surgery
- Haemorrhage
- Nausea & Vomiting
- Atelectasis
- Fat Embolism
- Anastomotic Leak
- Post-Op Ileus
- Bowel Adhesions
- Incisional Hernia
- Constipation
- Acute Kidney Injury
- Urinary Retention
- Urinary Tract Infection
- Hypoglycaemia
- Hyperkalaemia
- Hypokalaemia
- Hypernatremia
- Hyponatraemia
- Surgical Site Infection
- Wound Dehiscence
- Initial Assessment
- The General Approach
- A-E Assessment
- Referring a Patient
- IV Fluid Management
- Post-Op Fever
- Post-Op Pain
- Cardiovascular
- Respiratory
- Cardiothoracic Incisions
- Digital Rectal
- Abdominal Incisions
- Peripheral Vascular
- Peripheral Venous
- Cranial Nerves
- Peripheral Neurological
- Diabetic Foot
- Thyroid Gland
- Foot & Ankle
- Oral Cavity
- Certifying Death
- Acute Abdomen
- Haematemesis
- Gastric Outlet Obstruction
- Bowel Obstruction
- Bowel Perforation
- Rectal Bleeding
- Oesophageal Cancer
- Oesophageal Tears
- Motility Disorders
- Hiatus Hernia
- Peptic Ulcer Disease
- Gastric Cancer
- Inguinal Hernia
- Femoral Hernia
- Abdominal Wall Hernia
- Gastroenteritis
- Angiodysplasia
- Small Bowel Tumours
- Neuroendocrine Tumours
- Acute Appendicitis
- Colorectal Cancer
- Diverticular Disease
- Crohn’s Disease
- Ulcerative Colitis
- Pseudo-Obstruction
- Haemorrhoids
- Pilonidal Sinus
- Fistula-in-Ano
- Anorectal Abscess
- Anal Fissure
- Rectal Prolapse
- Anal Cancer
- Colic & Cholecystitis
- Cholangitis
- Cholangiocarcinoma
- Hepatocellular Carcinoma
- Liver Cysts
- Liver Abscess
- Acute Pancreatitis
- Chronic Pancreatitis
- Pancreatic Cancer
- Cystic Neoplasms of the Pancreas
- Splenic Infarct
- Splenic Rupture
- Acutely Painful Limb
- Lower Limb Ulcers
- Carotid Artery Disease
- Abdominal Aortic Aneurysm
- Aortic Dissection
- Thoracic Aortic Aneurysm
- Acute Limb Ischaemia
- Chronic Limb Ischaemia
- Acute Mesenteric Ischaemia
- Chronic Mesenteric Ischaemia
- Pseudoaneurysm
- Peripheral & Visceral Aneurysms
- Varicose Veins
- Venous Insufficiency
- Thoracic Outlet Syndrome
- Subclavian Steal Syndrome
- Hyperhidrosis
- Scrotal Pain
- Acute Urinary Retention
- Chronic Urinary Retention
- Lower Urinary Tract Symptoms
- Scrotal Lumps
- Renal Tract Calculi
- Pyelonephritis
- Renal Cancer
- Renal Cysts
- Urinary Incontinence
- Bladder Cancer
- Benign Prostatic Hyperplasia
- Prostate Cancer
- Prostatitis
- Epididymitis
- Testicular Torsion
- Testicular Cancer
- Fournier’s Gangrene
- Paraphimosis
- Penile Fracture
- Penile Cancer
- Peyronie’s Disease
- Hypospadias
- Cryptorchidism
- Balanitis Xerotica Obliterans
- Osteoarthritis
- Fracture Management
- Acutely Swollen Joint
- Open Fracture
- Compartment Syndrome
- Septic Arthritis
- Osteomyelitis
- Bone Tumours
- Clavicle Fracture
- Rotator Cuff Tear
- Shoulder Fracture
- Shoulder Dislocation
- Humeral Shaft Fracture
- Biceps Tendinopathy
- Adhesive Capsulitis
- Subacromial Impingement Syndrome
- Supracondylar Fracture
- Olecranon Fracture
- Radial Head Fracture
- Elbow Dislocation
- Olecranon Bursitis
- Epicondylitis
- Distal Radius Fracture
- Scaphoid Fracture
- Carpal Tunnel Syndrome
- Dupuytren’s Contracture
- De Quervain’s Tenosynovitis
- Ganglionic Cysts
- Trigger Finger
- Radiculopathy
- Degenerative Disc Disease
- Cervical Fracture
- Thoracolumbar Fracture
- Neck of Femur Fracture
- Hip Osteoarthritis
- Femoral Shaft Fracture
- Quadriceps Tendon Rupture
- Distal Femur Fracture
- Pelvic Fracture
- Acetabular Fracture
- Knee Osteoarthritis
- Meniscal Tear
- Patella Fracture
- Tibial Shaft Fracture
- Tibial Plateau Fracture
- Iliotibial Band Syndrome
- Ankle Fracture
- Calcaneal Fracture
- Achilles Tendonitis
- Talar Fracture
- Tibial Pilon Fracture
- Lisfranc injury
- Hallux Valgus
- Plantar Fasciitis
- The Limping Child
- Growth Plate Fracture
- Triple Assessment
- Galactorrhoea
- Inflammatory Disease
- Benign Tumours
- Gynaecomastia
- Carcinoma in Situ
- Invasive Cancer
- Surgical Treatments
- Non-Surgical Treatments
- Hoarse Voice
- Facial Palsy
- Hearing Loss
- Otitis Externa
- Acute Otitis Media
- Otitis Media with Effusion
- Chronic Mucosal Otitis Media
- Chronic Squamous Otitis Media
- Acute Rhinosinusitis
- Chronic Rhinosinusitis
- Periorbital Cellulitis
- Nasal Trauma
- Obstructive Sleep Apnoea
- Tonsillitis
- Deep Neck Space Infections
- Foreign Bodies
- Sialolithiasis
- Sialadenitis
- Salivary Gland Tumours
- Thyroid Cancer
- Head & Neck Cancer
- Assessment of Head Injury
- Extradural Haematoma
- Subdural Haematoma
- Diffuse Axonal Injury
- Traumatic Spinal Cord Injury
- Monro-Kellie Doctrine
- Intracranial Pressure Monitoring
- Hydrocephalus
- Subarachnoid Haemorrhage
- Intracranial Aneurysms
- Intracerebral Haemorrhage
- Arteriovenous Malformation
- Intracranial Infections
- Pituitary Tumours
- Spinal Tumours
- Deep Brain Stimulation
- Epilepsy Surgery
- Cauda Equina Syndrome
- Spinal Cord Compression
- Spinal Infections
- Principles of Wound Management
- Burns Assessment
- Burns Reconstruction
- Skin Grafts and Flaps
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Flexor Tendon Injuries
- Extensor Tendon Injuries
- Metacarpal Fractures
- Phalangeal Fractures
- Nail Bed Injuries
- Finger Replantation
- Skin Abscess
- Necrotising Fasciitis
- Bite Injuries
- Hand Infections
- Cardiopulmonary Bypass
- Bridge to Transplantation
- Foetal & Adult Circulation
- Coronary Artery Disease
- Valvular Disease
- Cardiac Tumours
- Lung Cancer
- Airway Disorders
- Chest Wall Disorders
- Mediastinal Tumours
- Diaphragmatic Hernia
- Pneumothorax
- Haemothorax
- Principles of Transplantation
- Concepts of Brain Death
- Organ Retrieval
- Immunosuppression in Transplantation
- Renal Transplantation
- Liver Transplantation
- Pancreas Transplantation
- Heart Transplantation
- Lung Transplantation
- I&D Abscess
- Diagnostic Laparoscopy
- Appendicectomy
- Small Bowel Resection
- Hartmann’s Procedure
- Gastroscopy
- Colonoscopy
- Excision of a Lump
- Open Inguinal Hernia Repair
- Laparoscopic Inguinal Hernia Repair
- Open Umbilical Hernia Repair
- Laparoscopic Cholecystectomy
- Nissen Fundoplication
- Oesophagectomy
- Gastric Band
- Gastric Bypass
- Sleeve Gastrectomy
- Lay Open Fistula
- Haemorrhoidectomy
- Pilonidal Sinus Repair
- Reversal of a Stoma
- Right Hemicolectomy
- Left Hemicolectomy
- Anterior Resection
- Abdominoperineal Resection
- Carotid Endarterectomy
- Open AAA Repair
- Lower Limb Amputation
- Angioplasty and Stenting
- Embolectomy
- Femoral Endarterectomy
- Arterial Bypass
- Axillofemoral Bypass
- Lower Limb Bypass
- Fem-Fem Crossover
- Endovenous Ablation
- Varicose Veins Stripping
- Foam Sclerotherapy
- AV Fistula Formation
- Cervical Rib Excision
- Flexible Cystoscopy
- Rigid Cystoscopy
- Suprapubic Catheterisation
- Scrotal Exploration
- Inguinal Orchidectomy
- Hydrocoele Excision
- Epididymal Cyst Excision
- Circumcision
- Dorsal Slit Procedure
- Ureteric Stent Insertion
- Percutaneous Nephrolithotomy
- Nephrectomy
- Flexible Nasal Endoscopy
- Microlaryngoscopy
- Grommet Insertion
- Myringoplasty
- Adenoidectomy
- Septoplasty
- Functional Endoscopic Sinus Surgery
- Parotidectomy
The Pre-Operative Assessment
Last updated: July 3, 2021 Revisions: 39
- 1 Pre-Operative History
- 2.1 American Society of Anaesthesiologists Grade
- 3.1.1 Group and Save versus Cross-Match
- 3.2 Cardiac Investigations
- 3.3 Respiratory Investigations
- 3.4 Other Tests
The pre-operative assessment is an opportunity to identify co-morbidities that may lead to patient complications during the anaesthetic, surgical, or post-operative period . Patients scheduled for elective procedures will generally attend a pre-operative assessment 2-4 weeks before the date of their surgery.
In this article, we shall look at the components of an effective pre-operative history , examination , and routine investigations that can be performed.
Pre-Operative History
The pre-operative history follows the same structure as typical history taking, with the addition of some anaesthetic and surgery specific topics.
History of the Presenting Complaint
A brief history of why the patient first attended and what procedure they have subsequently been scheduled for. One should also confirm the side on which the procedure will be performed (if applicable)
There may be aspects of the disease or condition requiring surgery that are important for the anaesthetist to be aware of; for example, head and neck surgery may indicate the presence of abnormal airway anatomy.
Past Medical History
A full past medical history (PMH) is required, with the following specifically asked about:
- Screening questions may elucidate undiagnosed disease and prompt further investigation, e.g. the presence of exertional chest pain , syncopal episodes , or orthopnoea
- Questions including whether the patient is able to lie flat for a prolonged period or has a chronic cough are key as these may preclude spinal anaesthesia; also screen for symptoms and signs of obstructive sleep apnoea , if the patient has any risk factors
- Renal disease , including their baseline renal function and any renal-specific medications
- Endocrine disease , specifically diabetes mellitus and thyroid disease
- Whilst this may be overlooked as a diagnosis or in their past medical history, particularly if patient managed with over-the-counter medicines, it is important to ask about at the pre-operative assessment
Other specific questions it may be useful to ask themselves the following questions:
- Pregnancy – as part of the pre-operative checklist on the day of surgery, for females of reproductive age a urinary pregnancy test is mandatory in the majority of hospitals
- Sickle Cell Disease – could they have undiagnosed sickle cell disease, especially if their country of birth does not have routine screening for sickle cell
Past Surgical History
Has the patient had any previous operations ? If so, what, when, and why?
If the patient is having a repeat procedure, this can significantly change both the surgical time and ease of operation , and hence influence the anaesthetic technique used
Past Anaesthetic History
Has the patient had anaesthesia before ? If so, for what operation and what type of anaesthesia? Were there any problems? Did the patient experience any post-operative nausea and vomiting ?
Drug History
A full drug history is required, as some medications require stopping or altering prior to surgery. Ask about any known allergies, both drug and non-drug allergies
Family History
Whilst most hereditary conditions relating to anaesthesia are extremely rare , such as malignant hyperthermia , it is important to ask about any known family history of problems with anaesthesia
Social History
Ensure to ask the patient about smoking history, alcohol intake , and any recreational drug use
Other important social factors to make note of include:
- Language spoken and the need for an interpreter
- Living situation , as the absence of an adult at home may require an admission overnight
Pre-Operative Examination
In the pre-operative examination, two distinct examinations are performed; the general examination (to identify any underlying undiagnosed pathology present) and the airway examination (to predict the difficulty of airway management e.g. intubation). If appropriate, the area relevant to the operation can also be examined.
Perform a full general examination , looking closely for any obvious cardiovascular (in particular undiagnosed murmurs or signs of heart failure), respiratory, or abdominal signs. An anaesthetic examination , including an airway assessment (typically using the Mallampati score), will also be performed by the anaesthetist prior to any surgery
American Society of Anaesthesiologists Grade
On all anaesthetic charts, a patient will be given an American Society of Anaesthesiologists (ASA) grade after their pre-operative assessment, which has been subjectively assessed and based on the criteria below. A patient’s ASA grade directly correlates with their risk of post-operative complications and absolute mortality.
Pre-Operative Investigations
The nature of the exact investigations required depends on a number of factors, including co-morbidities, age, and the nature of the procedure.
The urgency of the surgery will also dictate which conditions need further investigation and management prior to surgery. For example, elective surgery is often delayed for poorly controlled blood glucose levels in diabetic patients, to allow time for optimisation
Each specific hospital is likely to provide local guidelines , however it is useful to understand the tests than could be done pre-operatively and have an appreciation as to why each may be requested. NICE produce a colour traffic light table which can further guide your investigative decisions.
Blood Tests
- Most patients will get a full blood count , predominantly used to assess for any anaemia or thrombocytopenia , as this may require correction pre-operatively to reduce the risk of cardiovascular events or allow for preparation of blood products
- To assess the baseline renal function , which help inform fluid management and drug decisions, both for anaesthesia and post-operative analgesia (e.g. morphine is generally avoided in those with CKD)
- Important in the assessing liver metabolism and synthesising function , useful for peri-operative management; if there is suspicion of liver impairment, LFTs may help direct medication choice and dosing
- There are several conditions or diseases that may require specific bloods, such as HbA1C or thyroid function tests (TFTs)
- Any indication of deranged coagulation , such as iatrogenic causes (e.g. warfarin), inherited coagulopathies (e.g. haemophilia A/B), or liver impairment, will need identifying and correcting or managing appropriately in the peri-operative period
- Group and Save (G&S) +/- cross-matching
Group and Save versus Cross-Match
Group and Save (G&S) and Cross-Match (X-match) are two tests that are slightly different in their aims:
- A G&S is recommended if blood loss is not anticipated, but blood may be required should there be greater blood loss than expected
- This process also takes ~40 minutes (in addition to the 40 minutes required to G&S the blood, which must be done first), and should be done pre-emptively if blood loss is anticipated
Cardiac Investigations
An ECG is often performed in individuals with a history of cardiovascular disease or for those undergoing major surgery . It can indicate any underlying cardiac pathology and provide a baseline for comparison if there are post-operative concerns for cardiac ischaemia.
An echocardiogram (ECHO) provides very useful information for the anaesthetist as it helps to risk stratify and tailor the intra-operative care of the patient. It may be considered if the person has (1) a heart murmur (2) ECG changes (3) signs or symptoms of heart failure.
For patients with untreated ischaemic heart disease, or symptoms of angina, myocardial perfusion scans are often performed to look for inducible ischaemia.
Respiratory Investigations
If a patient has a chronic lung condition e.g. COPD, spirometry may be of use in assessing current baseline and predicting post-operative pulmonary complications in these patients. Patients may also be referred for spirometry if there are symptoms and signs of undiagnosed pulmonary disease.
Plain film chest radiographs (CXR) are less commonly performed routinely pre-operatively and should be used only when necessary
Other Tests
Especially for urological procedures, a urinalysis must be performed to assess if there is any evidence or suspicion of ongoing urinary tract infection
All patients will have swabs taken from the nostril and perineum for MRSA colonisation . If this is isolated, decontamination hair and body wash , along with topical ointment applied to the nostrils, will be given.
Cardiopulmonary Exercise Testing
High-risk patients undergoing major surgery may be referred for cardiopulmonary exercise testing (CPET) . This usually involves a graded intensity period on a stationary bicycle whilst wearing a mask, as well as ECG monitoring. It provides useful information, such as the VO2max and anaerobic threshold , which can be used to risk-stratify patients for post-operative complications and need for higher level care environments
[start-clinical]
[end-clinical]
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview

- about Merck
- Merck Careers
Preoperative Evaluation
- Procedural Risk Factors |
- Patient Risk Factors |
- More Information |
Before elective surgical procedures, whether done in an outpatient or inpatient setting, the surgical team may consult an internist for a formal preoperative evaluation to minimize risk by identifying correctable abnormalities and by determining whether additional perioperative monitoring and treatment are needed. The goal of a thorough preoperative evaluation should be to provide patients with a personalized surgical plan to minimize operative risk and postoperative complications. In some cases, elective procedures should be delayed when possible so that certain underlying disorders (eg, hypertension, diabetes, hematologic abnormalities) can be optimally controlled. In other cases, patients deemed high risk for major surgery may be identified preoperatively as candidates for less invasive interventions.
A thorough preoperative medical evaluation may require input from nonsurgical consultants (eg, internists, cardiologists, pulmonologists) to help assess surgical risk. Such consultants may also help manage preexisting disease (eg, diabetes) and help prevent and treat perioperative and postoperative complications (eg, cardiac, pulmonary, infectious). Psychiatric consultation is occasionally needed to assess capacity or help deal with underlying psychiatric problems that can interfere with recovery.
Older patients may benefit from involvement of an interdisciplinary geriatric team , which may need to involve social workers, therapists, ethicists, and other practitioners.
Because not all surgical procedures are elective, the acuity and type of proposed operation should be considered as well as the patient's risk with surgery. For example, if an emergency procedure is required (eg, for intra-abdominal hemorrhage, perforated viscus, necrotizing fasciitis), there is usually no time for a full preoperative evaluation. However, the patient's history should be reviewed as expeditiously as possible, particularly for allergies and to help identify factors that increase risk of emergency surgery (eg, history of bleeding problems or adverse anesthetic reactions).
A relevant preoperative history includes information about all of the following:
Current symptoms suggesting an active cardiopulmonary disorder (eg, cough, chest pain, dyspnea during exertion, ankle swelling) or infection (eg, fever, dysuria)
Risk factors for excessive bleeding (eg, known bleeding disorder, history of bleeding excessively with dental procedures, elective surgeries, or childbirth)
Risk factors for thromboembolism ( Professional. Deep Venous Thrombosis (DVT) )
Risk factors for infection
Risk factors for cardiac disease
Known disorders that increase risk of complications, particularly hypertension, heart disease, kidney disease, liver disease, diabetes, asthma, and COPD (chronic obstructive pulmonary disease)
Previous surgery, anesthesia, or both, particularly their complications
Tobacco, alcohol, and illicit drug use
Current prescription and nonprescription drug and supplement use
History of obstructive sleep apnea or excessive snoring
If an indwelling bladder catheter may be needed, patients should be asked about prior urinary retention and prostate surgery.
Physical examination
Physical examination should address not only areas affected by the surgical procedure but also the cardiopulmonary system, as well as a search for any signs of ongoing infection (eg, upper respiratory tract, skin).
When spinal anesthesia is likely to be used, patients should be evaluated for scoliosis and other anatomic abnormalities that may complicate lumbar puncture.
Any cognitive dysfunction, especially in older patients who will be given a general anesthetic, should be noted. Preexisting dysfunction may become more apparent postoperatively and, if undetected beforehand, may be misinterpreted as a surgical complication.
In symptomatic patients, those with known underlying disease, or those undergoing operations with a higher risk of significant bleeding or other complications, laboratory evaluation may include the following tests:
Complete blood count (CBC) and urinalysis (glucose, protein, and cells) usually are done. CBC is particularly relevant in patients > 65 or in younger patients with significant anticipated blood loss.
Serum electrolytes and creatinine and plasma glucose are measured unless patients are extremely healthy and < 50, the procedure is considered very low risk, and use of nephrotoxic drugs is not expected.
Liver tests are often measured if abnormalities are suspected based on the patient’s history or examination.
Coagulation studies and bleeding time are needed only if patients have a personal or family history of bleeding diathesis or a disorder associated with bleeding.
ECG is done for patients at risk of coronary artery disease (CAD), including all men > 45 and women > 50, and for severely obese patients (body mass index ≥ 40 kg/m 2 ) with at least one risk factor for atherosclerotic cardiovascular disease (eg, diabetes, smoking, hypertension, or hyperlipidemia) or poor exercise tolerance ( 4 ).
Chest x-ray only in patients with symptoms of or risk factors for underlying cardiopulmonary disease.
Pulmonary function testing may be done if patients have a known chronic pulmonary disorder or symptoms or signs of pulmonary disease.
Patients with symptomatic CAD need additional tests (eg, stress testing , coronary angiography ) before surgery.
Testing references
1. Fleisher LA, Fleischmann KE, Auerbach AD, et al : ACC/AHA 2014 guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery (executive summary); a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130:2215-2245, 2014. doi: 10.1161/CIR.0000000000000105
2. O'Neill F, Carter E, Pink N, et al : Routine preoperative tests for elective surgery: summary of updated NICE guidance. BMJ 354:i3292, 2016. doi:10.1136/bmj.i3292
3. Feely MA, Collins CS, Daniels PR, et al : Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician 87(6):414-418, 2013.
4. Poirier P, Alpert MA, Fleisher LA, et al : Cardiovascular evaluation and management of severely obese patients undergoing surgery: a science advisory from the American Heart Association. Circulation 120(1):86-95, 2009. doi:10.1161/CIRCULATIONAHA.109.192575
Procedural Risk Factors
Procedural risk is highest with the following:
Heart or lung surgery
Hepatic resection
Intra-abdominal surgeries that are estimated to require a prolonged operative time or that have a risk of large-volume hemorrhage (eg, Whipple procedure, aortic surgery, retroperitoneal surgery)
Open prostatectomy
Major orthopedic procedures (eg, hip replacement)
Patients undergoing elective surgery that has a significant risk of hemorrhage should consider banking blood for autologous transfusion should it be needed. Autologous transfusion decreases the risks of infection and transfusion reactions.
Emergency surgery has a higher risk of morbidity and mortality than the same surgery done electively.
Patient Risk Factors
The contribution of patient risk factors to perioperative morbidity and mortality is best estimated by validated quantitative risk calculators. For example, the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) has developed a risk calculator to predict perioperative adverse events (see ACS NSQIP Surgical Risk Calculator ). Use of these tools not only allows uniformity in interpreting surgeons' outcomes data but also contributes to better shared decision-making and informed consent for patients and family members ( 1 ).
Older age is associated with decreased physiologic reserve and greater morbidity if a complication occurs. However, chronic disorders are more closely associated with increased postoperative morbidity and mortality than is age alone. Older age is not an absolute contraindication to surgery.
Cardiac risk factors
Cardiac risk factors dramatically increase surgical risk. Perioperative cardiac risk is typically assessed using the American College of Cardiology/American Heart Association's Revised Cardiac Risk Index ( see Figure: Algorithm for risk stratification for noncardiac surgery ). It considers the following independent predictors of cardiac risk:
History of coronary artery disease (CAD)
History of heart failure
History of cerebrovascular disease
Serum creatinine (2.0 mg/dL)
Risk of cardiac complications increases with increasing risk factors:
No risk factors: 0.4% (95% confidence interval 0.1 to 0.8%)
1 risk factor: 1.0% (95% confidence interval 0.5 to 1.4%)
2 risk factors: 2.4% (95% confidence interval 1.3 to 3.5%)
≥ 3 risk factors: 5.4% (95% confidence interval 2.8 to 7.9%)
A high-risk surgical procedure (eg, vascular surgery, open intrathoracic or intraperitoneal procedure) also independently predicts a high cardiac perioperative risk.
Patients with active cardiac symptoms (eg, of heart failure or unstable angina) have a particularly high perioperative risk. Patients with unstable angina have about a 28% risk of perioperative myocardial infarction. In patients with stable angina, risk is proportional to their degree of exercise tolerance. Patients with active cardiac symptoms thus require thorough evaluation. For example, the cause of heart failure should be determined so that perioperative cardiac monitoring and treatment can be optimized before elective surgery. Other cardiac testing, such as stress echocardiography or even angiography , should be considered if there is evidence of reversible cardiac ischemia on preoperative evaluation.
Preoperative care should aim to control active disorders (eg, heart failure, diabetes) using standard treatments. Also, measures should be taken to minimize perioperative tachycardia, which can worsen heart failure and increase risk of myocardial infarction; for example, pain control should be optimized and beta-blocker therapy should be considered, especially if patients are already taking beta-blockers. Coronary revascularization should be considered for patients with unstable angina. If a heart disorder cannot be corrected before surgery or if a patient is at high risk of cardiac complications, intraoperative and sometimes preoperative monitoring with pulmonary artery catheterization may be advised. Sometimes the cardiac risk outweighs the benefit of surgery. In such cases, a less invasive procedure may provide or serve as a bridge to definitive treatment (eg, tube cholecystostomy for cholecystitis) and decrease morbidity and mortality.
Algorithm for risk stratification for noncardiac surgery
Incidental bacterial infections discovered preoperatively should be treated with antibiotics. However, infections should not delay surgery unless prosthetic material is being implanted; in such cases, surgery should be postponed until the infection is controlled or eliminated.
Patients with respiratory infections should be treated and have evidence that the infection has resolved before receiving inhalational anesthesia.
Viral infections with or without fever should be resolved before elective surgery is done, especially if a general anesthetic is going to be used.
Fluid and electrolyte imbalances
Fluid and electrolyte imbalances should be corrected before surgery. Hypokalemia, hyperkalemia, hypocalcemia, and hypomagnesemia must be corrected before general anesthesia to decrease risk of potentially lethal arrhythmias. Dehydration and hypovolemia should be treated with IV fluids before general anesthesia to prevent severe hypotension on induction—blood pressure tends to fall when general anesthesia is induced.
Nutritional disorders
Undernutrition and obesity increase the risk of postoperative complications in adults. Nutritional status is assessed preoperatively using history, physical examination, and laboratory tests.
Severe nutritional risk factors include the following:
A body mass index 2 or a history of unintentional weight loss > 10% of body weight over 6 months or 5% over 1 month
Suggestive physical examination findings (eg, muscle wasting, signs of specific nutritional deficiencies)
It is important to ask whether weight loss was intentional, because unintentional weight loss may reflect a catabolic state refractory to nutritional repletion, suggesting serious underlying pathology such as cancer.
< 2 ). In some cases, surgery can be delayed so patients can receive nutritional support, sometimes for several weeks (eg, in chronically undernourished patients, to help prevent the refeeding syndrome).
Significant obesity (body mass index > 40 kg/m 2 ) increases perioperative mortality risk because such patients have increased risk of cardiac and pulmonary disorders (eg, hypertension, pulmonary hypertension, left ventricular hypertrophy, heart failure, coronary artery disease). Obesity is an independent risk factor for deep venous thrombosis and pulmonary embolism; preoperative venous thromboembolism prophylaxis is indicated in most obese patients. Obesity also increases risk of postoperative wound complications (eg, fat necrosis, infection, dehiscence, and abdominal wall hernias).
Patient risk factor references
1. Bilimoria KY, Liu Y, Paruch JL, et al : Development and evaluation of the universal ACS NSQIP surgical risk calculator: A decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217(5):833-42.e423, 2013. doi:10.1016/j.jamcollsurg.2013.07.385
2. Weimann A, Braga M, Harsanyi L, et al : ESPEN guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr 25:224–244, 2006. doi: 10.1016/j.clnu.2006.01.015
More Information
The following English-language resource may be useful. Please note that The Manual is not responsible for the content of this resource.
2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery : A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Learn about the flu shot , COVID-19 vaccine , and our masking policy »
- Doctors, Clinics & Locations, Conditions & Treatments
- Patients & Visitors
- Medical Records
- Support Groups
- Help Paying Your Bill
- COVID-19 Resource Center
- Locations and Parking
- Visitor Policy
- Hospital Check-in
- Video Visits
- International Patients
View the changes to our visitor policy »
View information for Guest Services »
New to MyHealth?
Manage Your Care From Anywhere.
Access your health information from any device with MyHealth. You can message your clinic, view lab results, schedule an appointment, and pay your bill.
ALREADY HAVE AN ACCESS CODE?
Don't have an access code, need more details.
Learn More about MyHealth » Learn More about Video Visits »
MyHealth for Mobile
Get the iPhone MyHealth app » Get the Android MyHealth app »

WELCOME BACK
Anesthesia preoperative evaluation clinic, experts in preoperative anesthesia assessment.
If you are scheduled for surgery, you may have questions about anesthesia and pain control. Our goal at the Stanford Preoperative Anesthesia Evaluation Clinic is to give you all the information you need to set your mind at ease about the safety of anesthesia and relief of post-surgical discomfort.
As national leaders in preoperative anesthesia evaluation, our doctors work with medically complex and/or frail patients that other providers may decline to treat. We work with thousands of patients each year including many who travel to us from around the country and the world.
We go far beyond the usual history and physical to thoroughly evaluate your medical history and conditions before you have surgery. You can access our services at multiple convenient locations in the Bay Area.

- See All Locations »

Care and Treatment
What to expect.
At the Stanford Anesthesia Preoperative Evaluation Clinic, we perform a comprehensive review of your past medical history, assess your current health status and obtain any additional testing we feel is required to help keep you safe during anesthesia.
If you have undergone a preoperative anesthesia examination in the past, you may be expecting a brief physical evaluation and an order for an EKG test. We go well beyond this brief exam. Our goal is to determine your readiness for anesthesia and create an individualized plan that tells you exactly what you need to do in the days and hours leading up to your surgery.
Preparing for Your Anesthesia Evaluation Appointment
Your surgeon will schedule your appointment with our clinic. If you have any test results or medical records from your primary care physician, cardiologist, or other physician for your upcoming surgical procedure in anesthesia, please bring them with you so we can review them during your visit.
Anesthesia Evaluation: What to Expect
Start by checking in at the front desk. Our friendly staff will assist you with any questions.
Here’s what to expect during your appointment:
- You will undergo a brief physical examination by a specially trained anesthesia nurse practitioner or an anesthesiology resident physician. These professionals will perform a chart review with you and obtain a detailed medical history.
- One of our anesthesiologists will talk with you about your medical history, clarify any test results and determine if you would benefit from additional testing prior to your surgery. If so, the Anesthesia Preoperative Evaluation Clinic will make any required appointments for you before you leave our facility.
- Our anesthesia team may discuss various anesthesia options available to you. These may include combinations such as conscious sedation with a regional nerve block, for example. We encourage you to ask any questions you may have about these different types of anesthesia.
- One of our nurse practitioners or an anesthesiologist will discuss with you what to expect on the day of surgery. We want you and your family to understand exactly how the day will unfold. We welcome your questions about post-operative pain management so you know what to expect when you wake up.
- What medications to take normally
- Which medications to stop taking – and when to stop taking them
- What you may eat prior to surgery
- When to stop eating and drinking before surgery
- Any special medications you will need to take before surgery, along with instructions about exactly how to take them
- Transportation arrangements you will need to get to and from the hospital
- We will answer absolutely all of your questions. We want you to feel confident and prepared for your surgery by the time you leave your appointment.
Learn more about the doctors at the Anesthesia Preoperative Evaluation Clinic.
Depending on your individual needs, your preoperative assessment visit may last between 30 and 60 minutes. It may take a little longer if we need to telephone one of your providers to clarify your medical history.
If you need additional preoperative testing we may be able to arrange a same-day appointment at another clinic.
For Patients
Stanford Health Care is known worldwide for the advanced patient care provided by its doctors and staff. We also provide a wide range of guest services and amenities to our patients and visitors. Learn more about preparing for a hospital stay, billing and financial services, and our other support programs in Patients & Visitors .
We plan to perform a very thorough assessment of your readiness for anesthesia. You can help us in this process by obtaining past and current medical records, test results and films. When we have access to all of this information, we may be able to avoid sending you for additional testing.
Anesthesia Evaluation: What to Bring
Please bring the following to your anesthesia evaluation appointment, if you have them:
- Medical records
- Laboratory test results
- Cardiac test results, including ECG and stress test results
- Contact information for your physician(s)
If you have questions about whether or not you should bring a particular document or test result, please do bring it with you.
You may hand carry these items to your appointment to the clinic where you will have your preoperative evaluation or fax them in advance.
- Billing and insurance
For Health Care Professionals
At Stanford, we work with medically complex and frail patients other anesthesia providers decline to treat. While many anesthesia providers won’t evaluate a patient until a surgery date is set, we will see high-risk patients for a consult-only appointment in advance to determine if they meet the necessary criteria to receive anesthesia.
HOW TO REFER
Fax a referral form with supporting documentation to 650-320-9443.
PHYSICIAN HELPLINE
Stanford Health Care provides comprehensive services to refer and track patients, as well as the latest information and news for physicians and office staff. For help with all referral needs and questions, visit Referral Information .
You may also submit a web referral or complete a referral form and fax it to 650-320-9443 or email the Referral Center at [email protected] .
At Stanford we understand sometimes even the sickest patients require non-emergent surgery to extend their life or improve their quality of life. If you have questions about your patient’s readiness for anesthesia, or if another provider has declined to treat your patient, the Stanford Anesthesia Preoperative Evaluation Clinic will evaluate your high-risk patients and make recommendations regarding how to prepare them for anesthesia
Schedule a High-Risk Consult-only Appointment
Surgeons and other providers may make an appointment directly with any of the four Stanford Anesthesia Preoperative Evaluation Clinic locations. Please advise your patients about what to expect and what to bring with them to their appointment.
If we find your patient is not a candidate for anesthesia, we will work with them to optimize their health to prepare them for anesthesia. We offer:
- In-patient optimization for patients that need intensive support
- Nutrition counseling when baseline health needs a boost
- Other supportive services as required on a per-case basis
- Frequent communication with the patient’s surgeon and other medical clinicians to keep everyone informed of the individual’s progress
- Send referrals online
- Place radiology and lab orders
- View referral status
- Access medical records
Learn More About MedLink »
For general inquires or questions about anesthesiology or perioperative care, call:
Anesthesia Preoperative Evaluation Clinic at Stanford Hospital: 650-724-1429
Anesthesia Preoperative Evaluation Clinic at Stanford Medicine Outpatient Center: 650-721-7852
Anesthesia Preoperative Evaluation Clinic at Stanford Cancer Center South Bay: 408-426-4900
Anesthesia Preoperative Evaluation Clinic at Byers Eye Institute: 650-723-6995

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Tests and visits before surgery
Your surgeon will want to make sure you are ready for your surgery. To do this, you will have some checkups and tests before surgery.
Many different people on your surgery team may ask you the same questions before your surgery. This is because your team needs to gather as much information as they can to give you the best surgery results. Try to be patient if you are asked the same questions more than once.
Pre-op Checkup
Pre-op is the time before your surgery. It means "before operation." During this time, you will meet with one of your doctors. This may be your surgeon or primary care doctor:
- This checkup usually needs to be done within the month before surgery. This gives your doctors time to treat any medical problems you may have before your surgery.
- During this visit, you will be asked about your health over the years. This is called "taking your medical history." Your doctor will also do a physical exam.
- If you see your primary care doctor for your pre-op checkup, make sure your hospital or surgeon gets the reports from this visit.
Some hospitals also ask you to have a phone conversation or meet with an anesthesia pre-op nurse before surgery to discuss your health.
You may also see your anesthesiologist the week before surgery. This doctor will give you medicine that will make you sleep and not feel pain during surgery.
Visits With Other Doctors
Your surgeon will want to make sure that other health conditions you may have will not cause problems during your surgery. So you may need to visit:
- A heart doctor (cardiologist), if you have a history of heart problems or if you smoke heavily, have high blood pressure or diabetes, or are out of shape and cannot walk up a flight of stairs.
- A diabetes doctor (endocrinologist), if you have diabetes or if your blood sugar test in your pre-op visit was high.
- A sleep doctor, if you have obstructive sleep apnea , which causes choking or a stop in breathing when you are asleep.
- A doctor who treats blood disorders (hematologist), if you've had blood clots in the past or you have close relatives who have had blood clots.
- Your primary care provider for a review of your health problems, exam, and any tests needed before surgery.
Tests Before Surgery
Your surgeon may tell you that you need some tests before surgery. Some tests are for all surgical patients. Others are done only if you are at risk for certain health conditions.
Common tests that your surgeon may ask you to have if you have not had them recently are:
- Blood tests such as a complete blood count (CBC) and kidney, liver, and blood sugar tests
- Chest x-ray to check your lungs
- ECG ( electrocardiogram ) to check your heart
Some doctors or surgeons may also ask you to have other tests. This depends on:
- Your age and general health
- Health risks or problems you may have
- The type of surgery you are having
These other tests may include:
- Tests that look at the lining of your bowels or stomach, such as a colonoscopy or upper endoscopy
- Heart stress test or other heart tests
- Lung function tests
- Imaging tests, such as an MRI scan , CT scan , or ultrasound test
Make sure the doctors who do your pre-op tests send the results to your surgeon. This helps keep your surgery from being delayed.
Alternative Names
Before surgery - tests; Before surgery - doctor visits
Levett DZ, Edwards M, Grocott M, Mythen M. Preparing the patient for surgery to improve outcomes. Best Pract Res Clin Anaesthesiol . 2016;30(2):145-157. PMID: 27396803 pubmed.ncbi.nlm.nih.gov/28687213/ .
Sandberg WS, Dmochowski R, Beauchamp RD. Safety in the surgical environment. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery . 21st ed. St Louis, MO: Elsevier; 2022:chap 9.
Review Date 2/28/2022
Updated by: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
Tip: Turn on your clipboard history .
Find us at Mastodon , Facebook , Threads , Twitter , Reddit , Youtube , & Linkedin
Check out the cheat sheet – you can print it off if you’d like.
5 well-known features and 5 hidden gems
Preoperative Note
- View Live Form Edit Markup Data Dictionary
There are 2 form elements.
- Fill from CSV file
Fill from CSV data
Result - copy and paste this output:.
- Save to CSV file
- Show CSV data
Note S. Preoperative Note. The SOAPnote Project. https://www.soapnote.org/complete/preoperative-note/. Published May 11, 2013. Updated February 22, 2023. Accessed May 1, 2024.
Send Feedback for this SOAPnote Cancel reply
Your email address will not be published. Required fields are marked *
- Yoga Prescription
- Suicide Risk Assessment
- SOAPnote Project Donations since 2023-11-01
Take our product tour to see why we're the leader in cloud practice management software
Take your patients from referral to receipt through the cloud
Your Practice in the palm of your hands with our Doctor App.
Discover the latest news, expert interviews and practical advice to help strengthen and support your practice.
Our resources have helped thousands of medical professionals with everything from patient experience to practice efficiency.
Learn how to use the Patient Portal and improve your health journey.
View upcoming and view-on-demand webinars.
Clinic to Cloud is trusted by more than 7,200 healthcare professionals worldwide.
Looking for a tutorial, product updates, and education? Our help centre will have the answers you need.
Find the help you need here.
Unlocking a new vision for connected care.
Search for helpful articles, research papers, and guides.
Creating Your Pre-Op Checklist and Post-Op Checklist Templates
In private surgical practices, pre-operative checklists and post-operative checklists are commonly used by admin staff. It forms an important part of documenting the needs and requirements for a patient who is having an upcoming procedure .
In this article, our Professional Education Manager, Cheryl Ladikos , outlines the guiding principles for having a pre-op and post-op checklist, why it’s important, and how to eff ectively create these checklists that is tailored for each individual practice.
Whether you’re a New Fellow, Practice Manager or Business Manager, it is important to develop tools that your admin staff can use and o ne of the common tools of a surgical practice is a pre-op checklist and post-op checklist. These checklists , often combined into one, can help practices to prepare a patient for an upcoming procedure . It follows the patient’s journey from start to finish and focuses on health and safety. These checklists also become a vital communication tool and auditing trail in a patient’s medical record.
What are the guiding principles in pre- and post-operative care?
Based on my experience as a Practice Manager, I believe t here are three guiding principles in developing the most effective pre- and post-op care:
Guiding Principle 1: Understand Perioperative Care
Perioperative care is the care given to patients before, during, and after surgery and can take place in a hospital, day surgery or within a private practice. Perioperative care generally includes three stages:
- Pre-operative
- Intra-operative
- Post-operative
In most cases, it is the first and third stage that is used in a private practice as the intra-operative stage is managed within a hospital environment.
The aim of understanding perioperative care is to provide better conditions for a patient before a procedure takes place. By collecting information prior to surgery, a practice can make better decisions about advanced care planning. This also helps patients to pr epare for surgery, whether physically or emotionally.
Nurses play an important role in the care of their patients . The care provided should be competent, holistic and evidenced based and must consider the patient’s emotional and psychological responses, as described in this HealthTimes article.
Guiding Principle 2: Understand Your Patient ’s Needs
When developing a pre- and post-operative checklist for your practice, it is first and foremost about your patient. You r patient is entrusting the Surgeon with a procedure which is to improve or promote better health outcomes and your practice has a duty of care to ensure that the procedure will run smoothly. Your patients have different experiences, and you need to prepare them physically and emotionally and to ensure that they are we ll-informed prior to surgery.
- Patient – what information do you need from your patient so that safe care is provided? What information do you need to provide to your patient so that they are well-informed about their upcoming procedure?
Guiding Principle 3: Understand Other Stakeholder Needs
By adopting patient-centric care, you must then consider the needs and requirements that fulfill all these important stakeholders:
- Surgeon – what do es the Surgeon need to perform the procedure effectively and safely ?
- Anaesthetist – what information do they need to know about the patient for safe choice and dosage of anaesthesia ?
- Assistant Surgeo n - not all procedures require an Assistant Surgeon however, if needed, what information do they need to know about your patient so that they can effectively and safely assist the Surgeon?
- Hospital Theatre – what information do they need to know about your patient and the Surgeon’s needs , to ensure a safe operating environment ?
Why is a pre- and post-op checklist important?
Pre-op and post-op checklists are an important communication tool used within private surgical practices for each patient having an upcoming procedure. It is important for administrative staff to be aware of these tools and how to use them effectively, as it is not just a list with tick boxes. These checklists are important because it become s an auditing trail to demonstrate how your practice has effectively prepared for the health and safety of your patient ’s upcoming surgical procedure.
How can I create a pre- and post-op checklist?
The following list provides information about how you can create a pre- and post-op checklist:
- Pre- and post-op checklist templates needs to be tailored for each individual practice.
- Create a template which can be used for all procedures, rather than a checklist for each procedure.
- Ask the Surgeon and Anaesthetist (s) to find out what are the common key ques tions that they need to have answered prior to surgery .
- Develop rapport with your Hospital Admissions or Theatre Managers and find out what information they would like to obtain from your practice.
- Draft a list and formulate the questions in a chronological order, making sure that each question is easily understood by admin staff.
- Create your final list into your practice management software, if it has the capability of creating Checklist Templates like in Clinic to Cloud.
- Educate your staff about using the checklist for each procedure , and how to use it.
For a list of commonly asked questions, click on this link to download a copy of our Private Practice Pre-Op and Post-Op Checklist Guide .
For more information on Clinic to Cloud, click here or contact us today.

Discover the latest news, expert interviews and practical advice to help strengthen and support your practice

IntelyCare for Healthcare Facilities > Resources > Nursing Job Description Samples > Pre-op Nurse Job Description Template
Pre-op Nurse Job Description Template
Search resource center.

Pre-operative nurses are essential to providing high-quality surgical care. They assist with patient admission, assess for risk factors , prepare patients for surgery, and coordinate treatment options with different members of the multidisciplinary team. If you’re looking to hire one of these clinicians for your peri-operative department , crafting a tailored pre-op nurse job description can help you find an employee with the skills for success.
In this article, we review the duties, skills, and qualifications of pre-operative nurses to help you recruit the best possible candidate. We also outline benefits, compensation, and flexible scheduling options that can help your position stand out among the competition.
Before you begin writing your job description, it can help to perform market research to see how other organizations advertise their nursing positions. Reviewing our pre-op nurse job postings can help refine your language and word choice to appeal to top candidates. You’ll then need to organize a set of pre-op nursing interview questions to ask your pool of qualified applicants. After completing these steps, you can focus on developing your job description.
Pre-Op Nurse
Tips: Start out your pre-op nurse job description by introducing your organization and the patient population you serve. Provide a brief description of the role and clarify the experience level you’re looking for. Sharing information on any awards, accolades, or certifications garnered by your team can give candidates insight into the exceptional care your facility provides.
Ready for an exciting next step in your peri-operative career? At [facility name], we’re looking to hire an experienced pre-operative nurse to join our surgical team. Ideal candidates will have at least three years of experience caring for adult and pediatric patients in an outpatient surgical setting.
Here at [facility name], we pride ourselves on our passion for patient safety, which is why we’ve been voted “Miami’s Safest Surgical Center” for the past two years. We’re excited to be expanding our industry-leading surgical intervention options and can’t wait to grow our dedicated and driven clinical team.
When you join our organization, you’ll have the opportunity to enroll in our full employee benefits package, which includes health insurance, tuition reimbursement, and subsidized transport to and from work. Continue reading as we outline the skills and qualifications we’re looking for and when you’re ready, apply below to join our team.
Tips: Now that you’ve introduced the basics of the position, take the opportunity to highlight key elements of your employee benefits package. With benefits making up over 30% of a job’s total compensation package, it’s important to show them off near the top of your pre-op nurse job description. Be sure to list a variety of professional, financial, and lifestyle perks to help you appeal to a wide array of applicants.
- Competitive pay
- Health, dental, and vision benefits
- FSA/HSA options
- 401(k) matching
- Paid vacation/holiday/family leave
- Free continuing education (CE) courses
- Tuition reimbursement of up to $5,000 per year
Duties and Responsibilities
Tips: Some facilities divide tasks between separate pre-operative and post-operative clinical teams, while others use one large perioperative team to assist with all stages of the surgical process. To prevent any confusion down the line, be sure to differentiate your organization’s pre-op nurse duties from those of a scrub or post-op nurse.
Job descriptions for pre-op nurses should also specify the clinical setting you’re hiring for. These employees work in a variety of patient care areas, including:
- Acute care hospitals
- Outpatient surgical centers
- Physician offices and clinics
Clarifying where the employee would be expected to work can help prospective candidates assess whether their unique clinical experience qualifies them for the role.
Pre-operative nurse duties include, but are not limited to, the following:
- Stocking medical supplies and preparing safety equipment in each patient room
- Performing pre-surgical assessments and documenting findings in the patient’s electronic health record (EHR)
- Communicating any patient allergies, anesthesia contraindications, and surgical risks with the surgical team
- Inserting and maintaining peripheral intravenous lines (PIVs)
- Providing the patient with the appropriate pain and anxiolytic medication and monitoring for complications
- Escorting the patient to the operating room and providing safe patient handoff to the receiving nursing team
- Educating patients and their family members on the surgical process and routinely updating them throughout the intra-operative phase
Pre-Op Nurse Salary and Schedule Requirements
Tips: Joining a new surgical team can come with a steep learning curve and may be daunting to nursing professionals comfortable in their current role. Show them why transitioning to your facility is worth the time and effort.
Your pre-op nurse job description should list an accurate pay rate and specify whether the position is hourly or salaried. Be sure to mention any opportunities for bonuses or pay raises to keep the interest of applicants who may be considering future career growth opportunities. Outline scheduling expectations, including evening, weekend, and on-call requirements, to prevent any misunderstandings later in the process.
- Our pre-operative nurse salary starts at $95,000 , with adjustments subject to education level and relevant leadership experience
- Overtime, on-call, holiday, and incentive pay available
- 6-week paid orientation period
- 3 scheduled 12-hour day shifts (7a-7p) per week
- Weekend day/night on-call shifts required (2 shifts per month required, with available opportunities for more at the employee’s request)
- Bi-weekly or weekly pay periods
Pre-Op Nurse Qualifications and Skills
Tips: Prospective applicants often have questions regarding the degree, licensure, and certification requirements of the position. Be sure to list all of your facility’s pre-op nurse job qualifications, along with any additional attributes or skills that could be helpful when performing the duties of the role. Specifying which qualifications are required and which are preferred can ensure you don’t inadvertently turn away suitable candidates.
Required Qualifications:
- Active and unencumbered RN license
- BSN required, MSN preferred
- BLS, ACLS, and PALS certified
- 2 years of experience working in the perioperative setting (pre-operative department, post anesthesia care unit, operating room, interventional radiology, etc.)
- Familiarity with electronic health record (EHR) documentation
Preferred Qualifications:
- Previous experience at a Level I Trauma Center
- CPAN or CAPA Certification
- Impeccable organization, time management, and critical-thinking skills
- Bilingual in English and Spanish
Call to Action
Tips: You’ve spent valuable time crafting a pre-op nurse job description that’s sure to wow prospective applicants. In this final section, it’s time to guide interested candidates to the job application. Including a link titled “Apply Now” or “Click Here to Apply” can encourage them to get started right away.
Ready to take the next step in your pre-operative nursing career? Click “Apply Now” to start filling out your application today. The entire process takes less than 10 minutes. Thank you for your interest — we look forward to hearing from you soon.
Recruit Great Pre-Op Nurses and Grow Your Surgical Team
Now that you’ve written an enticing pre-op nurse job description, you’re one step closer to finding an exceptional employee. Now, your organization might be looking for an easier way to grow your applicant pool. By posting your open roles to our nursing job board, you can reach over 1 million qualified clinicians who are ready to work.
Related Articles
Ccu nurse job description template, health informatics job description template, clinical pharmacist job description template, certified nurse midwife (cnm) job description template, ent nurse job description template, related jobs, reach 1 million+ nursing professionals, with the intelycare job board.
- Skip to main content
- Keyboard shortcuts for audio player
- Latest Show
- Terry Gross
- Tonya Mosley
- Contact Fresh Air
- Subscribe to NPR's Up First Email

Jon Bon Jovi, shown here in 2011, says the band's 1986 hit "Livin' on a Prayer" has "touched more lives than I could have ever dreamt." David Bergman/Hulu hide caption
Music Interviews
'i can only give the best': bon jovi on vocal surgery and his road to recovery.
A few years ago, Jon Bon Jovi stopped performing due to a vocal cord injury. The Hulu docuseries Thank You, Goodnight offers a career retrospective, plus a view of his surgery and return to the stage.

'I can only give the best': Bon Jovi on vocal surgery and the road to recovery
by Terry Gross
- See Fresh Air sponsors and promo codes

Follow these four steps to code quickly and accurately, while reducing the need to count up data points.
KEITH W. MILLETTE, MD, FAAFP, RPh
Fam Pract Manag. 2021;28(4):21-26
Author disclosure: no relevant financial affiliations.

The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1 , 2 To ease the transition, previous FPM articles have laid out the new American Medical Association/CPT medical decision making guide 3 and introduced doctor–friendly coding templates (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), explained how to quickly identify level 4 office visits (see “ Coding Level 4 Visits Using the New E/M Guidelines ,” FPM , January/February 2021), and applied the new guidelines to common visit types (see “ The 2021 Office Visit Coding Changes: Putting the Pieces Together ,” FPM , November/December 2020).
After several months of using the new coding rules, it has become clear that the most difficult chore of coding office visits now is assessing data to determine the level of medical decision making (MDM). Analyzing each note for data points can be time-consuming and sometimes confusing.
That being the case, it's important to understand when you can avoid using data for coding, and when you can't. I've developed a four-step process for this (see “ A step-by-step timesaver ”).
The goal of this article is to clarify the new coding rules and terminology and to explain this step-by-step approach to help clinicians code office visits more quickly, confidently, and correctly.
The new evaluation and management office visit coding rules have simplified many things but are still a lot to digest, especially when it comes to counting data.
There are different levels of data and different categories within each level, which can make using data to calculate the visit level time-consuming and confusing.
By calculating total time, and then moving on to assessing problems and prescription drug management, most visits can be optimally coded without dealing with data at all.
OFFICE VISIT CODING RULES AND TERMINOLOGY
To make full use of the step-by-step process, we have to first understand the new rules, as well as coding terminology. Here is a brief summary.
Medically appropriate . Physicians and other qualified health care professionals may now solely use either total time or MDM to determine the level of service of an office visit. That means the “history” and “physical exam” components are no longer needed for code selection, which simplifies things. But your patient note must still contain a “medically appropriate” history and physical. So continue to document what is needed for good medical care.
New patient . A new patient is a patient who has not been seen by you or one of your partners in the same medical specialty and the same group practice within the past three years.
Total time and prolonged services . Total time includes all the time you spend on a visit on the day of the encounter (before midnight). It includes your time before the visit reviewing the chart, your face-to-face time with the patient, and the time you spend after the visit finishing documentation, ordering or reviewing studies, refilling medications, making phone calls related to the visit, etc. It does not include your time spent performing separately billed services such as wellness visits or procedures. Total time visit level thresholds differ for new patients vs. established patients. (See the total times in “ The Rosetta Stone four-step template for coding office visits .”)
The prolonged services code comes into play when total time exceeds the limits set for level 5 visits by at least 15 minutes.
Medical decision making . MDM is made up of three components: problems, data, and risk. Each component has different levels, which correspond to levels of service (low/limited = level 3, moderate = level 4, and high/extensive = level 5). The highest level reached by at least two out of the three components determines the correct code for the level of service. MDM criteria is the same for new and established patients.
Problems addressed . This includes only the problems you address at that specific patient visit. It does not include all the patient's diagnoses and does not include problems that are exclusively managed by another clinician. Problems addressed are separated into low-complexity problems (level 3), moderate-complexity problems (level 4), and high-complexity problems (level 5). To code correctly, you need to know the coding value of the problems you address. It is helpful to think of problems in terms of levels of service (e.g., a sinus infection is usually a level 3 problem, and pneumonia or uncontrolled diabetes are usually level 4 problems).
The simplest way to summarize problems is this: Life-threatening problems are level 5; acute or chronic illnesses or injuries are level 3 or 4 depending on how many there are, how stable they are, and how complex they are; and if there's just one minor problem, it's level 2.
(For more specifics see “ What level of problem did I address? ”)
Risk . Risk is also separated into “low” (level 3), “moderate” (level 4), and “high” (level 5) categories.
Level 3 risk includes the use of over-the-counter (OTC) medications.
Level 4 risk includes the following:
Prescription drug management: starting, stopping, modifying, refilling, or deciding to continue a prescription medication (and documenting your thought process),
Social determinants of health that limit diagnosis or treatment (this is when patients' lack of finances, insurance, food, housing, etc., affects your ability to diagnose, manage, and care for them as you normally would).
Level 5 risk includes the following:
Decisions about hospitalization,
Decisions about emergency major surgery,
Drug therapy that requires intensive toxicity monitoring,
Decisions to not resuscitate or to de-escalate care because of poor prognosis.
Data analyzed . For purposes of MDM, data is characterized as “limited” (level 3 data), “moderate” (level 4 data), or “extensive” (level 5 data). But each level of data is further split into Categories 1, 2, and 3. This can make calculating data complicated, confusing, and time-consuming. Here are the data components and terms you need to know.
Category 1 data includes the following:
The ordering or reviewing of each unique test , i.e., a single lab test, panel, X-ray, electrocardiogram (ECG), or other study.
Ordering and reviewing the same lab test or study is worth one point, not two; a lab panel (e.g., complete blood count or comprehensive metabolic panel) is worth one point,
Reviewing a pertinent test or study done in the past at your own facility or another facility,
Reviewing prior external notes from each unique source, including records from a clinician in a different specialty or from a different group practice or facility as well as each separate health organization (e.g., reviewing three notes from the Mayo Clinic is worth one point, not three, but reviewing one note from Mayo and one from Johns Hopkins is worth a total of two points),
Using an independent historian, which means obtaining a history from someone other than the patient, such as a parent, spouse, or group home staff member. (This is included in Category 2 for level 3 data, but falls into Category 1 for level 4 and 5 data.)
Category 2 data includes the following:
Using an independent historian (for level 3 data only),
Independent interpretation of tests, which is your evaluation or reading of an X-ray, ECG, or other study (e.g., “I personally reviewed the X-ray and it shows …”) and can include your personal evaluation of a pertinent study done in the past at your or another facility. It does not include reviewing another clinician's written report only, and it does not include studies for which you are also billing separately for your reading.
Category 3 data includes the following:
Discussion of patient management or test interpretation with an external physician, other qualified health care professional, or appropriate source. An external physician or other qualified health care professional is someone who is not in your same group practice or specialty. Other appropriate sources could include, for example, consulting a patient's teacher about the patient's attention deficit hyperactivity disorder.
A STEP-BY-STEP TIMESAVER
The majority of office visits can be optimally coded by using time or by looking at what level of problems were addressed (see Steps 1 and 2 below) and whether a prescription medication was involved.
A level 3 problem can be coded as a level 3 visit if you address it with an OTC or prescription medication. A level 4 problem can be coded as a level 4 visit if you order prescription medication or perform any other type of prescription drug management (modifying, stopping, or deciding to continue a medication). Most level 2 and level 5 office visits are straightforward, and most level 5 visits will be coded by time. They will typically be visits in which you address multiple problems or complicated problems and the total time exceeds 40 minutes for established patients. This is much more common than seeing critically ill patients who may require admission, which is another level 5 scenario. The few remaining patient visits that have not already been coded require analyzing data (Steps 3 and 4). (See “ The Rosetta Stone four-step template for coding office visits .”)
Step 1: Total time . Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to Step 2.
Step 2: “Problems plus.” Don't be afraid to move on from time-based coding if you believe you performed a higher level visit using MDM. Many visits can be coded with MDM just by answering these two questions: What was the highest-level problem you addressed during the office visit? And did you order, stop, modify, or decide to continue a prescription medication?
If you addressed a level 2 problem and your total time was less than 20 minutes (or less than 30 for a new patient), then code level 2.
If you addressed a level 3 problem, plus you recommended an OTC medication or performed prescription drug management, then code level 3.
If you addressed a level 4 problem, plus you performed prescription drug management, then code level 4.
Chronic disease management often qualifies as level 4 work. For documentation, think “P-S-R”: problem addressed, status of the problem (stable vs. unstable), and prescription drug management (Rx). This trio should make it clear to coders, insurance companies, and auditors that level 4 work was performed.
For instance, if a patient has controlled hypertension and diabetes and you document that you decided to continue the current doses of losartan and metformin, that's level 4 (two stable chronic illnesses plus prescription drug management). If you see a patient with even one unstable chronic illness and document prescription drug management to address it, that's also level 4.
For a level 5 problem, if you see a really sick patient and decide to admit or consider admission (and you document your thought process in your note), then code level 5.
By starting with total time and, if necessary, moving on to “problems plus,” you will probably be able to optimally code 90% of your office E/M visits. But on the rare occasions when you see a patient for level 4 or 5 problems for less than the required time and don't do any prescription drug management, you may have to proceed to Steps 3 and 4.
Step 3: Level 4 problem with simple data or social determinants of health concerns . Code level 4 if you saw a patient for a level 4 problem and did any of the following:
Personally interpret a study (e.g., X-ray),
Discuss management or a test with an external physician,
Modify your workup or treatment because of social determinants of health.
Step 4: Level 4 or 5 problem with complex data . If you saw a patient for a level 4 problem and still haven't been able to code the visit at this point, you have to tally Category 1 data points:
Review/order of each unique test equals one point each,
Review of external notes from each unique source equals one point each,
Use of an independent historian equals one point.
Once you reach three points, code it as level 4.
For a level 5 problem, if you see a really sick patient, order/interpret an X-ray or ECG, and review/order two lab tests, then code level 5.
Following these steps should allow you to quickly identify the optimal level to code most any E/M office visit (for pre-op visits, see “ Coding pre-ops template .”)
Here's a catchy rhyme to remember the basic outline of the steps:
To finish fast ,
code by time and problems first ,
and save data for last .
By mastering the new coding rules and terminology and applying this four-step approach, you can code office visits more quickly, accurately, and confidently — and then spend more time with your patients and less time at the computer.
CPT Evaluation and Management (E/M) Office or Other Outpatient and Prolonged Services Code and Guideline Changes . American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
E/M Office Visit Compendium 2021. American Medical Association; 2020.
Table 2 – CPT E/M office revisions level of medical decision making. American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf
Continue Reading

More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Pre-operative outpatient medical evaluation can decrease the length of hospital stay as well as minimize postponed or cancelled surgeries. 1 To effectively provide this consultative service, the ...
The goal of the evaluation of the healthy patient is to detect unrecognized disease and risk factors that may increase the risk of surgery above baseline and to propose strategies to reduce this risk. The evaluation of healthy patients prior to surgery is reviewed here. Preoperative assessments for specific systems issues and surgical ...
The Preoperative Evaluation. Key Points to Start: *Remember, you can access Epic through the Ether website (ether.stanford.edu) whether on or off campus* *If there is no Pre-op done in Epic, do a chart biopsy, look up old records, and call the patient (if necessary) to gather this important information that is vital in developing a safe and effective anesthetic plan*
Sponsored in part through a grant from Perioperative Medicine Education, Inc. This guide is intended as a clinical resource for clinicians performing preoperative evaluations. The author has done his best to assure the information is current and based upon the available evidence. Recommendations which are based on the author's opinion only (due ...
RCRI Risk Score: _____ (High-risk surgical procedure, ischemic heart disease, heart failure, CVA/TIA, DM on Insulin, chronic renal insufficiency) The patient has a ( low / elevated ) risk of a £ major cardio vascular event. If elevated, please specify patient's Metabolic Equivalents (METs): >4 <4 Unable to assess. £ £ £.
Preoperative evaluation: A time-saving algorithm. J Fam Pract. 2016 October;65 (10):702-704,706-710. By. Michael J. Arnold, MD, CDR, USN. Joshua Beer, DO. Author and Disclosure Information. Our preop evaluation method combines the latest guidelines and tools to help you avoid unnecessary testing and complete the process in one visit. PDF Download.
The pre-operative assessment is an opportunity to identify co-morbidities that may lead to patient complications during the anaesthetic, surgical, or post-operative period.Patients scheduled for elective procedures will generally attend a pre-operative assessment 2-4 weeks before the date of their surgery. In this article, we shall look at the components of an effective pre-operative history ...
1. Fleisher LA, Fleischmann KE, Auerbach AD, et al: ACC/AHA 2014 guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery (executive summary); a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.Circulation 130:2215-2245, 2014. doi: 10.1161/CIR.0000000000000105
The Day of Your Surgery. Preparing at home. • Adult patients - Do not eat or drink anything up to six hours before you arrive at the medical center for your surgery. • Adult patients - If your surgery is after noon (12 p.m.), you may have 4 oz. of clear liquids up to three hours before your arrival time.
Phone: 1-866-742-4811. Fax: 650-320-9443. Monday-Friday, 8 a.m.-5 p.m. Stanford Health Care provides comprehensive services to refer and track patients, as well as the latest information and news for physicians and office staff. For help with all referral needs and questions, visit Referral Information.
Step 2. Ask the patient to draw a simple clock set to 10 minutes after 11 o'clock (11:10). A correct response is drawing of a circle with the numbers placed in approximately the correct positions ...
terized and investigated before elective surgery . LABORATORY TESTING Although laboratory testing is part of the pre-operative evaluation, it should be recognized as optional. Preoperative testing accounts for about $30 billion in health care costs each year.15 The value of routine testing before elective surgery is unclear,16 as most ...
Tests that look at the lining of your bowels or stomach, such as a colonoscopy or upper endoscopy. Heart stress test or other heart tests. Lung function tests. Imaging tests, such as an MRI scan, CT scan, or ultrasound test. Make sure the doctors who do your pre-op tests send the results to your surgeon.
Children presenting to the pre-op visit with a history of congenital anomalies require special attention. It is known that when there is one anomaly, more may potentially exist. Hence, collecting additional details about the patient's clinical condition is essential. In many cases, parents of children with rare disorders often know more about ...
Preoperative evaluation is a process of clinical assessment that precedes the delivery of anesthesia care for surgery and non-surgical procedures. At the very least, it includes a review of medical records and recent test results, a comprehensive medical history, and a physical examination of the cardiovascular system, the pulmonary system, and ...
See the "Diabetic Guidelines before Surgery" in the Patient Education section. n To find out my arrival time for surgery, I must call my surgical scheduler (see page 1) of Your Surgical Guide Book for specific surgical office. Revised: 2/2017 n I will bring this binder to all pre- and post-operative appointments AND day of surgery. n
Preoperative testing (e.g., chest radiography, electrocardiography, laboratory testing, urinalysis) is often performed before surgical procedures. These investigations can be helpful to stratify ...
Extr: Warm, no edema. Skin: No rashes, no significant lesions. Diagnoses: Presently Clinically Stable for Scheduled Surgery. Avoidance of; Aspirin, Ibuprofen, Naproxen, and other NSAIDS 5-7 days prior to surgery. To call with any changes in present status. Discussion-Plan:
Guiding Principle 2: Understand Your Patient's Needs. When developing a pre- and post-operative checklist for your practice, it is first and foremost about your patient. Your patient is entrusting the Surgeon with a procedure which is to improve or promote better health outcomes and your practice has a duty of care to ensure that the ...
In addition to the surgeon's discussion with the patient and family about indications for surgery, a preoperative evaluation is advised for all children and adolescents having elective surgery ...
Pre-Op Nurse. Tips: Start out your pre-op nurse job description by introducing your organization and the patient population you serve. Provide a brief description of the role and clarify the experience level you're looking for. Sharing information on any awards, accolades, or certifications garnered by your team can give candidates insight into the exceptional care your facility provides.
The Hulu docuseries Thank You, Goodnight offers a career retrospective, plus a view of his surgery and return to the stage. Jon Bon Jovi, shown here in 2011, says the band's 1986 hit "Livin' on a ...
Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to ...