Don’t need your labs collected yet?
Subscribe to receive a 10% off code and occasional promo codes in the future.

Type in the code we texted you.
You're all set, looks like you're already subscribed, need help booking or have a question.
Tap below to text or call us.
Book at-home lab collections.
How it works, 1. book your appointment, 2. we collect your samples, 3. get your lab results, simple and affordable pricing., we’ve redesigned the lab experience around you., comfortable, compassionate, partner with getlabs for at-home diagnostics., diagnostic services, nationwide coverage, technology platform, frequently asked questions, ready to book a visit with getlabs, in the news.

- Patient FAQ
- Labs Near Me
- Diagnostic Tests
- Partner FAQ
Getlabs® is the nationwide leader for at-home diagnostics. Healthcare organizations use our all-in-one technology platform to dispatch skilled medical specialists to their patients and collect labs, vitals, and advanced diagnostics. By partnering with us, providers can expand access to care, improve adherence, and make informed medical decisions remotely.
Better care starts at home. ®
- Labs Near Me
- CCPA Notice

Look out for your health
A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference.
Call 1-866-799-5895 ,
TTY 711, to schedule your visit.
HouseCalls brings yearly check-in care
To you at home.
Connect for up to a full hour of 1-on-1 time with a licensed health care practitioner. Every visit includes a physical, tailored recommendations on health care screenings and plenty of time to ask questions that matter to you.
After your visit, HouseCalls connects with your primary care provider (PCP) to help keep them informed about your health. It's a great way to feel confident knowing an extra set of eyes is looking out for you between regular PCP visits.
What is a HouseCalls visit?
[Text On Screen – SAY HELLO TO HOUSE CALLS]
Say hello to HouseCalls.
[Text On Screen- PAID ACTOR PORTRAYAL.]
HouseCalls is our way of looking out for your health, so you can focus on your future. Here’s what it’s all about.
[Text On Screen – HERE’S WHAT IT’S ALL ABOUT]
Once a year, a licensed health care practitioner can come to your home to spend up to an hour with you on your health and wellness.
[Text On Screen- EASY, CONVENIENT, INFORMATIVE]
It's designed to be easy, convenient and informative.
[Text On Screen- HEAD-TO-TOE EXAM]
[Text On Screen- IMPORTANT HEALTH SCREENINGS]
[Text On Screen- HEALTH GOALS DISCUSSION]
You'll get a head-to-toe exam, important health screenings and plenty of time to talk about your health goals.
We'll also provide guidance on managing your health and if you need it, give you referrals for other health plan resources and services.
HouseCalls is a great way to stay on top of your health between regular doctor's visits.
At the end of your visit, you'll get a personalized checklist so you can feel more confident in what to discuss with your regular doctor.
[Text On Screen- COST? NO EXTRA COST TO YOU]
[Text On Screen- INCLUDED IN YOUR HEALTH PLAN]
If you're wondering how much all of this is going to cost, the best part is, there is no extra cost to you. It's included in your health plan.
[Text On Screen- HOUSECALLS VIDEO VISITS ARE NOT AVAILABLE WITH ALL PLANS.]
A HouseCalls visit takes place in the comfort of your own home or by video if you prefer.
So, say hello to HouseCalls and invite us in for a visit today.
[Text On Screen – SAY HELLO TO HOUSE CALLS TODAY]
Access one of the most popular UnitedHealthcare offerings, at no cost to you
Schedule your visit
Call 1-866-799-5895 , TTY 711
Monday–Friday, 8 a.m.–8:30 p.m. ET
Your in-home health check-in
- Up to a full hour with a licensed health care practitioner
- Ask the questions that matter to you and get valuable health tips
- No cost — it's included in your health plan
Get rewarded
Meet your friendly housecalls medical staff.

Just like the professionals you see in your regular doctor’s office, our licensed health care practitioners may be nurse practitioners, physician assistants or medical doctors. They’re state licensed and maintain national certification.
We perform background checks on these professionals to provide additional peace of mind for our members. Your loved ones, caregivers or friends are welcome to be present during the visit — it’s up to you.
Ready to open the door to better health?
Getting ready for your housecalls appointment, tips to help you prepare: .
- Wear shoes that are easily removed to have your feet checked
- Make a list of upcoming appointments with your PCP and specialists
- Make sure all of your medications, both prescription and over-the-counter vitamins and supplements, are in their original bottles for our review
- If you record blood pressure readings, please have your results available for review
- If you have diabetes, please have your blood glucose meter handy
- Make a list of questions and concerns you’d like to discuss
During your appointment
- You'll have up to a full hour of 1-on-1 time with your health care practitioner for a physical, select lab tests, health screenings and more
- A HouseCalls visit can be completed while sitting at your kitchen table or in the living room, and you can use the time to ask any health-related questions
- The visit is tailored to your individual needs, so screenings and conversation topics can vary
After your appointment
Less travel time. more face time..
Think of HouseCalls as an extra layer of care — valuable 1-on-1 time you don't always get in the doctor's office. And it's tailored to your individual needs.
Schedule today
To secure your spot, call us at 1-866-799-5895 , TTY 711
Have a question?
Find answers to frequently asked questions.
If you have a specific question about your upcoming appointment or need to reschedule, call us at 1-866-799-5895, TTY 711 , Monday–Friday, 8 a.m.–8:30 p.m. ET
We're here to help.
- Skip to main content
- Clinical support programs
- Employee Assistance Program
- LGBTQ+ resources
- Maternity support
- Member support and advocacy resources
- Mental health programs
- Quit For Life
- Real Appeal
- Rewards programs
- Substance use
HouseCalls is check-in care that comes to you
Did you know you can set up a yearly preventive care visit at home.
UnitedHealthcare® HouseCalls — our yearly in-home health and wellness service — is a health plan feature for Medicare and Medicaid members, offered at no additional cost to you. It’s a way to help our members stay on top of their health between regular doctor visits.
Why is a HouseCalls visit a good idea?
Benjamin Franklin said it best, “An ounce of prevention is worth a pound of cure.” We agree. The goal of our preventive care visits is to help you maintain your independence and continue doing what you love long into the future. We know there’s no way to prevent all health emergencies and accidents, but we believe that by taking care of yourself, you may be able to improve your odds of avoiding them. That’s where HouseCalls comes in.
UnitedHealthcare® HouseCalls
Video transcript.
These days, you can have just about anything delivered to your door.
How about a home delivery of good health and wellness? It comes from UnitedHealthcare and is called HouseCalls.
HouseCalls is a yearly health and wellness visit that happens in the privacy of your very own home. No driving to an appointment. No sitting in a waiting room.
Here’s how it works.
Our HouseCalls team finds a time that’s convenient for you and schedules the visit. A health care practitioner, a physician’s assistant, medical doctor or nurse practitioner, comes to you at the scheduled time. The clinician completes a health evaluation, including a physical exam and other important screenings, then YOU decide what happens next.
You can discuss questions to ask your doctor at your next appointment, review instructions from your last doctor’s appointment or chat about other health concerns you haven’t had a chance to talk to your doctor about. Whatever you need.
The visit takes about 45-minutes to an hour – plenty of time to answer your important health questions.
Your practitioner will even send a summary of your HouseCalls visit to your doctor.
And unlike those other home deliveries – there’s no additional cost for a HouseCalls visit, it’s a feature of your medical plan. If you’re in good health or you already see your doctor regularly – you might not think HouseCalls is for you, but it is. Think of it as an extra layer of care – valuable one-on-one time you don’t always get in the doctor’s office.
So, when you get a phone call from our HouseCalls team – take advantage of this great program and schedule your HouseCalls visit. Or just call us and make an appointment!
It’s Easy. It’s Convenient. It’s UnitedHealthcare HouseCalls.
What to expect during a HouseCalls visit
During a HouseCalls visit, you’ll meet with the same types of professionals you’d see in a doctor’s office — a licensed physician or nurse practitioner. They’ll answer your health-related questions, perform a physical exam and offer a health screening in the comfort of your own home. If you choose, your family members, loved ones or caregivers are welcome to sit in on this visit and ask additional questions. A typical visit will range from 45 minutes to a full hour.
The results of your exam and screening will be forwarded to your primary care provider (PCP) and you’ll receive a summary of your visit in the mail.
During your visit, here are some typical topics you'll cover
- An overview of your medical history and prescription medications
- Conversations about overall well-being, like how to help you stay active, sleep well and manage stress
- Tips on to help you avoid trip hazards in your home
- Community resources and support
Open the door to the convenience of a medical visit in your home
Meet with licensed medical staff on your schedule, in the convenience of your home. Once they arrive, talk about health concerns at your pace (the visits are focused on you and you alone). Use the results to help coordinate care with your doctor.
- Be prepared to provide a urine sample during your visit—drink fluids in advance
- Wear shoes or slippers that are easy to remove (your feet will be checked)
- Know where to find medication bottles so they are ready to review
- If applicable, have blood pressure readings available for review
- If you have diabetes, please provide blood sugar test results, as well as your blood glucose meter
Remember, at the end of your visit, you’ll receive a personalized checklist of topics to discuss with your doctor at your next appointment. Plus, you and your doctor will receive a mailed summary of your visit.
Want more good news?
HouseCalls is included at no extra cost in most Medicare and Medicaid members as part of your health plan. 1 Schedule at a convenient time and we’ll come to you.
Call to request a visit 1-866-799-5895 , TTY 711 , Monday – Friday 8 a.m. – 8:30 p.m. ET
For medical emergencies, call 911.
Related Content
From simple to complex, we’ll help answer your Medicare questions. Learn more about Medicare
Explore Medicare Advantage Plans from UnitedHealthcare in your area. Shop for a Medicare plan
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Getting Test Results Quickly by Phone Call or Appointment
You may need to see your healthcare provider for results from blood tests and other exams
- Getting Results for Blood Tests
- Results by Phone Call
- Results Given in Person
- Results via Telehealth
- Results via Patient Portal
Setting Expectations
If you've recently had a medical test, such as blood work, you may wonder when to expect a call from your healthcare provider and how quickly you'll receive results.
The turnaround time for test results can depend on the type of test and why your doctor ordered it. Healthcare providers sometimes ask you to make an appointment to get the results of routine medical tests , especially when you're waiting for a new diagnosis or you're monitoring a chronic illness. Other times, you may be given the results by a phone call, telehealth, or online patient portal.
This article will look at how long it takes to get certain blood test results. It also covers when you might need an appointment to discuss results, when you don't, and what questions to ask your healthcare provider.
Getting Results for Common Blood Tests
After you get a blood test, the turnaround time for results can depend on the type of test and where the lab is based. If you're a patient in a hospital, test results from the hospital lab will usually take less time than an outside lab.
You may or may not be asked to come in for an in-person appointment depending on the type of test and why it's being done. For routine tests, you might receive a phone call or letter, or you may be able to access results through your patient portal.
Complete Blood Count (CBC)
A complete blood count measures the different parts of your blood, including red blood cells, white blood cells, and platelets, to detect different conditions like anemia and blood cancers.
CBC results are typically given to your healthcare provider by the following day. You may get a phone call or the results may be available on your online patient portal.
Basic Metabolic Panel (BMP)
A basic metabolic panel (BMP) gives information about your body's electrolytes, fluid levels, kidney health, and blood sugar.
BMP results are usually available by the next day. Your healthcare provider may call you or post the results on your online patient portal.
Comprehensive Metabolic Panel (CMP)
A comprehensive metabolic panel gives the same information as a BMP test in addition to information about your liver function and protein tests.
CMP results may be available after a few business days. You may get results from your healthcare provider by phone, mail, or through your online patient portal.
Lipid Panel
A lipid panel measures total cholesterol, HDL cholesterol, LDL cholesterol, and triglycerides to help determine your risk of heart disease.
Lipid panel results may be available the next day. You may get results from your healthcare provider by phone or through your online patient portal.
Thyroid Panel
The thyroid panel checks levels of hormones such as TSH and T4 in the blood. This helps determine how well the thyroid gland is working and diagnose any thyroid conditions.
Thyroid panel results usually take a few days. Your healthcare provider may have you come in for a follow-up appointment to get your results. They may also call you or put the information on your online patient portal.
Blood tests can be ordered to detect leukemia (cancer of the blood cells). They can also detect chemicals and proteins in your blood that could indicate different types of cancer.
Results for these blood tests may take a week or more. You may get results through an in-person appointment or a phone call with your healthcare provider.
Sexually Transmitted Infections (STIs)
Blood tests can help detect STIs such as HIV, syphilis, and herpes. Some of these blood tests, including HIV and herpes, look for antibodies that your body makes in response to the infection.
The turnaround time for the results may vary. For some rapid HIV tests, it may take just a few minutes. Other tests can take up to one to two weeks. You may have an in-person follow-up appointment or your healthcare provider may call you with the results.
Test Results Given by Phone Call
In some cases, an in-person appointment isn't all that necessary for getting results. Often, routine blood or imaging tests are part of preventive care. That includes things like cholesterol tests , mammograms , or Pap smears .
If results are normal, they can usually be delivered via a phone call. If results are abnormal, your healthcare provider may call you and ask to set up a separate follow-up appointment.
While healthcare providers can deliver results by phone, they have to verify it's you to ensure that they're not violating HIPAA privacy laws . They can also leave a voicemail message requesting you return the call. At a previous appointment, you may have been asked to sign a form verifying that they have your permission to leave a message.
Test Results Given in Person
Sometimes your healthcare provider will want to meet with you in person to discuss your results, whether it's blood work, a biopsy, or other medical tests. Even if the news is "good," it may be important for them to explain what the results do and don't mean. The test results may be simple and straightforward—say, positive or negative. Or they may be more nuanced or open to interpretation.
Your healthcare provider may have ordered tests to provide a diagnosis. Or they may want to monitor a condition, including tracking its progress or checking for a recurrence.
Getting test results may prompt new questions, which you can ask at this appointment.
Initial Diagnosis
News of a new diagnosis should usually be given face-to-face. That's because your health is at risk in some way. That could be from an infection , cancer , genetic disorder, or chronic health condition like heart disease or type 2 diabetes .
An appointment gives you an opportunity to talk about:
- The diagnosis
- What it means
- Your treatment options
It can also help avoid confusion over what the results mean. Sometimes you need to know more than just "positive" or "negative."
For example, if you test negative for HIV (human immunodeficiency virus) , you may assume you don't have it. All it really means, though, is that the test didn't detect the virus. You may have just been tested too early—before your immune system had a chance to make the antibodies the test detects.
At an appointment, your healthcare provider can explain options and tell you whether more testing is needed.
Plus, if a disease is contagious, your provider will want to talk in person about how to help you avoid future risks and protect other people.
Monitoring Chronic Illness
With chronic illness, follow-ups are often necessary to monitor the illness or see if a treatment is working.
For example, if you have prediabetes or hypertension (high blood pressure), you may not need treatment right away. The first steps may be to use diet and exercise to stop or reverse the disease.
Follow-up labs can tell you whether your strategies are working. Meeting in person to go over results helps you both see what's happening and figure out why. It's also an opportunity to discuss starting treatment.
If you're taking medications for chronic conditions, regular in-person appointments can help you stick to the treatment regimen. You can also discuss side effects and dosage changes that may be needed.
For diseases that can relapse, such as cancer and some autoimmune diseases , regular visits may help identify and treat a relapse early.
It is always okay to ask your healthcare provider about treatment guidelines or why a test or appointment is being recommended.
Test Results Given via Telehealth
Telehealth appointments may be a good compromise between delivering results in person versus a phone call, letter, or secure message. You still have to pay for it, but it can save you a lot of time.
Telehealth appointments allow you to meet with your healthcare provider over a video chat rather than an in-person appointment. Your healthcare provider might suggest this option if you've tested positive for an infectious disease, such as COVID-19, to limit the spread of the virus.
However, there may be some instances where you will need an in-person appointment instead. For instance, you may not be able to have a telehealth appointment if your healthcare provider needs you to have more tests done, or if they need to perform a physical examination.
Test Results Available via Patient Portal
Practices can send electronic messages (or post results to a patient portal) if they have a secure means of doing so. They're an easy way to view detailed test results as soon as they’re available.
While having access to your electronic medical records can ensure that you receive results, it may cause anxiety for those who get an abnormal result without a phone call. Your healthcare provider may prefer to send you a message about normal results through the patient portal and call you with abnormal results.
If your healthcare provider uses a patient portal, ask them about how you'll be receiving results and when you should check the patient portal.
When first meeting with a new healthcare provider, ask about their test result policies. In some cases, they want you to get tested a week or two before an appointment. Or you may be tested during or after your appointment and get the results later.
If you're tested during or after your appointment, ask:
- Do all test results require a follow-up appointment?
- How long does it take to get the test results?
- Does your staff contact patients regardless of results?
- If results are shared by phone, letter, or online patient portal, how does the office ensure they will only be shared with me or my designees?
Be wary of any office that says they only contact you "if there is a problem." First, you have the right to see the results of every test you undergo. Second, mistakes happen. You won't know whether you're fine or the results were somehow lost or not properly communicated to you.
You can also:
- Ask when the results will be ready and call that day or the next.
- Make a follow-up appointment beforehand if the results might be something you need to discuss.
- Double-check that the imaging center or lab has your provider’s correct information on file.
Remember there are many reasons why a healthcare provider will contact you after a medical test. If results are concerning, they may call you or have a receptionist call to schedule an appointment. A healthcare provider may also call to assure you everything is okay or discuss any needed follow-up tests.
The turnaround time for test results depends on the type of test, the location of the lab, and whether you need a follow-up appointment with your healthcare provider.
Your healthcare provider may suggest a follow-up appointment to go over test results. This could be if you're just being diagnosed or monitoring a chronic illness.
Your healthcare provider could also call or send a message through the online patient portal to let you know the results. You probably don't need an appointment for preventive tests or if your condition is well-controlled.
Ask your healthcare provider about how test results will be delivered. If follow-up appointments are expected, check with your health insurance to make sure they're covered.
MedlinePlus. Complete blood count (CBC) .
Labcorp Oklahoma, Inc. Complete blood count (CBC) .
Children's Minnesota. Blood test: Basic metabolic panel .
Testing.com. CMP blood test (Comprehensive metabolic panel) .
Children's Minnesota. Blood test: Lipid panel.
Testing.com. Thyroid panel test.
Nebraska Medicine. Can blood tests help detect cancer?
Norton Healthcare. How long does it take to get results of blood tests?
MedlinePlus. STD tests .
Delaney KP, Hanson DL, Masciotra S, Ethridge SF, Wesolowski L, Owen SM. Time until emergence of HIV test reactivity following infection with HIV-1: Implications for interpreting test results and retesting after exposure . Clin Infect Dis. 2017;64(1):53-59. doi:10.1093/cid/ciw666
Bazzano LA, Green T, Harrison TN, Reynolds K. Dietary approaches to prevent hypertension . Curr Hypertens Rep . 2013;15(6):694-702. doi:10.1007/s11906-013-0390-z
Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes . Cleve Clin J Med . 2017;84(7 Suppl 1):S15-S21. doi:10.3949/ccjm.84.s1.03
Health Resources and Services Administration. Telehealth and COVID-19 .
Giardina TD, Modi V, Parrish DE, Singh H. The patient portal and abnormal test results: An exploratory study of patient experiences . Patient Exp J . 2015;2(1):148-154.
Litchfield IJ, Bentham LM, Lilford RJ, Greenfield SM. Test result communication in primary care: clinical and office staff perspectives . Family Practice . 2014;31(5):592-597. doi:10.1093/fampra/cmu041
By Trisha Torrey Trisha Torrey is a patient empowerment and advocacy consultant. She has written several books about patient advocacy and how to best navigate the healthcare system.

Using CPT code 99211 can boost your practice’s revenue and improve documentation .
EMILY HILL, PA-C
Fam Pract Manag. 2004;11(6):32-33

The requirements for most evaluation and management (E/M) codes have gotten more precise over the years. However, one notable exception to this is CPT’s level-I established patient encounter code, 99211. CPT defines this code as an “office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician.” It further states that the presenting problems are usually minimal, and typically five minutes are spent performing or supervising these services. Yet many physicians still struggle with when – or why – to report this code. This article describes how appropriately reporting 99211 can improve revenue and documentation, and provides specific guidelines and examples that can help physicians identify appropriate uses for the code.
The benefits of 99211
Reporting 99211 can bring additional revenue into your practice. Specific payment amounts will vary by payer, but the average unadjusted 2004 payment from Medicare for a 99211 service is $21. This means that only five 99211 encounters with Medicare patients in a week will result in over $5,000 per year for a practice. Although this may not sound like a lot of money, it is easy revenue. Most practices already provide a number of 99211 services but fail to capture those charges. Remember, all services have a cost associated with them, and practices need to recoup as much of these costs as is legitimately possible.
Appropriately reporting 99211 services can also improve documentation in a practice. Staff members who are cognizant of billing guidelines tend to pay increased attention to documentation, which, in turn, can result in a more useful medical record for all providers involved in the care of the patient.
Only five 99211 encounters with Medicare patients in a week will result in over $5,000 per year.
Physicians can report 99211, but it is intended to report services rendered by other individuals in the practice, such as a nurse or other staff member.
Unlike other office visit E/M codes, a 99211 office visit does not have any specific key-component documentation requirements.
Basic guidelines
The following guidelines can help you decide whether a service qualifies for 99211:
The patient must be established. According to CPT, an established patient is one who has received professional services from the physician or another physician of the same specialty in the same group practice within the past three years. Code 99211 cannot be reported for services provided to patients who are new to the physician.
The provider-patient encounter must be face-to-face. For this reason, telephone calls with patients do not meet the requirements for reporting 99211.
An E/M service must be provided. Generally, this means that the patient’s history is reviewed, a limited physical assessment is performed or some degree of decision making occurs. If a clinical need cannot be substantiated, 99211 should not be reported. For example, 99211 would not be appropriate when a patient comes into the office just to pick up a routine prescription.
Keep in mind that if another CPT code more accurately describes the service being provided, that code should be reported instead of 99211. For example, if a physician instructs a patient to come to the office to have blood drawn for routine labs, the nurse or lab technician should report CPT code 36415 (routine venipuncture) instead of 99211 since an E/M service was not required.
The service must be separate from other services performed on the same day. Services that are considered part of another E/M service provided on the same day should not be reported with code 99211. For example, if a nurse provides instructions following a physician’s minor procedure or takes a patient’s vital signs prior to an encounter with the physician, 99211 should not be reported for these activities because they are considered part of the E/M service already being provided by the physician.
The presence of a physician is not always required. Although physicians can report 99211, CPT’s intent with the code is to provide a mechanism to report services rendered by other individuals in the practice (such as a nurse or other clinical staff member). According to CPT, the staff member may communicate with the physician, but direct intervention by the physician is not required.
Medicare’s requirements on this point are slightly different: While the physician’s presence is not required at each 99211 service involving a Medicare patient, the physician must have initiated the service as part of a continuing plan of care in which he or she will be an ongoing participant. (To some carriers, this means that the physician must see the patient at least every third visit.) In addition, the physician must at least be in the office suite when each service is provided. The reason for this difference is that Medicare considers these services to be an integral although “incidental” part of the physician’s professional service. According to Medicare and most third-party payers, incidental services should generally be reported under the name and billing number of the physician or other professional in the office suite when the service is provided. Note, however, that the services can also be billed “incident-to” other health professionals, such as physician assistants or nurse practitioners. [For more on incident-to billing, see “The Ins and Outs of ‘Incident-To’ Reimbursement,” FPM, November/December 2001, page 23 .]
Most practices already provide a number of 99211 services but fail to capture those charges.
No key components are required. Unlike other office visit E/M codes – such as 99212, which requires at least two of three key components (problem-focused history, problem-focused examination and straightforward medical decision making) – the documentation of a 99211 visit does not have any specific key-component requirements. Rather, the note just needs to include sufficient information to support the reason for the encounter and E/M service and any relevant history, physical assessment and plan of care. The date of service and the identity of the person providing the care should be noted along with any interaction with the supervising physician. Some practices create templates for the nurse to use when documenting these encounters. The templates can be specific to the reason for the encounter, such as a template for a follow-up blood-pressure check, or they can be generic forms that provide space for the suggested documentation components. [For some examples of flow sheets that can be used for 99211 services, see “Coding Level-One Office Visits: A Refresher Course,” FPM, July/August 2000, page 39 .]
Examples of 99211 services
Code 99211 is commonly used for services such as patient education, simple rechecks and medication reviews. Some procedures can also appropriately be reported with this code. To gain a better sense of the kinds of services that would qualify as a 99211, consult appendix C of the CPT manual and consider the following examples:
An established patient comes to the office with complaints of urinary burning and frequency. The nurse takes a focused history, reviews the medical record, discusses the situation with the physician and orders a urinalysis. The nurse then presents the findings to the physician, who writes a prescription for an antibiotic. The nurse communicates the instructions to the patient and documents the encounter in the medical record. In this example, 99211 and the appropriate laboratory code for the urinalysis should be reported because the E/M service is distinct from the lab service and appropriate for the evaluation of the patient’s complaint.
A patient comes to the office for a blood-pressure check. If the visit was scheduled at the request of the physician, 99211 should be reported. If the visit was prompted by the patient, the use of 99211 depends on whether there are clinical indications for the visit. For example, 99211 should not be reported for the stable patient who decides to come in for a blood-pressure check while in the area, because the physician did not order the service and there were no clinical indications to validate the need for the visit. However, if the patient was experiencing problems (e.g., dizziness or headache) and the nurse took additional history, checked the patient’s blood pressure and talked with the physician, 99211 would be appropriate since clinical indications prompted the intervention.
A nurse performs a suture removal on a patient whose sutures were placed at a different practice. Code 99211 could be reported for this service, since it describes the service better than any other CPT code (there is no specific CPT code for suture removal). Note, however, that 99211 would not be appropriate for the suture removal if the sutures were placed and removed at the same practice, because the code reported for placing the sutures would also include the removal.
A nurse performs a simple dressing change to assess and dress open wounds or other injuries. Code 99211 would be appropriate as long as the dressing change wasn’t performed as part of burn treatment (because there are other specific CPT codes that should be used for burns) or routine post-procedure care (because some procedures have a global period during which associated care is considered part of the payment for the procedure).
Use good judgment
Because some services are more appropriately reported with a CPT code other than 99211, because not every encounter has a clinical indication that supports a separate visit code and because some patients may balk at the idea of being charged for some 99211 services (such as a blood-pressure check) be cautious about establishing a practice of billing an E/M service with every staff encounter. Instead, use these guidelines and examples to determine the appropriate uses of 99211. Many Medicare carriers and other third-party payers periodically issue examples and guidelines regarding the proper use of certain codes, including this one. Staying knowledgeable about these coding practices can improve your practice’s reimbursement and reduce potential audit liability.
Continue Reading
More in fpm, more in pubmed.
Copyright © 2004 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
At-home blood tests
Get an appointment within 48 hours in the comfort of your home, at work or elsewhere.
We keep your peaople healthy and working!
The financial health of your company is intimately linked to the health of your employees. Our dedicated team can help you make the best choices in this area.
Partner in your success
In a complex and changing environment, medical professionals need to surround themselves with partners who are committed, flexible, efficient and creative.
Take advantage of a convenient way to get your lab tests done.
Certified and experienced mobile nursing staff
All you need is your prescription and access to a quiet, comfortable location. Our qualified professionals will come to you with all the necessary equipment, starting at $40.
A full range of medical analysis, sample collection and screening tests at home:
- Blood sample collection and complete blood tests
- Urine tests
- Stool tests
- STI screening
- Throat culture
- And much more...
Book an appointment today
Find out why patients appreciate the flexibility of Biron's at-home blood collection services and enjoy a convenient way to get your tests done.
Why choose at-home blood testing?
- The visit usually lasts less than 15 minutes
- Fasting is not required for most tests
- The cost of the tests is covered by most insurance companies
- The staff is courteous and takes the time to address your needs
- Our processes are subject to the strictest quality standards, especially in the transportation and handling of samples.
An appointment according to your availability, wherever you are
Whether at home, at work or elsewhere, get an appointment quickly in the following regions
- Laurentians
- Eastern Townships
The cost of a home or work visit is based on distance from certain Biron service centers and starts at $40. The cost of laboratory tests depends on the medical prescription. A routine blood test costs between $150 and $200 and may be fully or partially covered by your private insurance. The Biron agent will confirm the details when you make your appointment. A travel cost réduction of $40 will be applied if total tests fees are $350 and over.
Fasting is not required for most tests. If we find that your specific tests require fasting, we will let you know when you make your appointment.
The Biron nurse's visit, including sample collection and payment, usually takes less than 15 minutes. To learn more on how does an at-home blood test work .
Certainly, you can schedule many sample collections during the same visit. It is imperative to schedule an appointment time for each person. Please note that adddional fees will apply (starting at $29 per person added).
At-home blood tests can be taken from the age of 12.

Medicare Wellness Visits Back to MLN Print November 2023 Updates

What’s Changed?
- Added information about monthly chronic pain management and treatment services
- Added information about checking for cognitive impairment during annual wellness visits
- Added information about Social Determinants of Health Risk Assessments as an optional element of annual wellness visits

Quick Start
The Annual Wellness Visits video helps you understand these exams, as well as their purpose and claim submission requirements.
Medicare Physical Exam Coverage
Initial Preventive Physical Exam (IPPE)
Review of medical and social health history and preventive services education.
✔ New Medicare patients within 12 months of starting Part B coverage
✔ Patients pay nothing (if provider accepts assignment)
Annual Wellness Visit (AWV)
Visit to develop or update a personalized prevention plan and perform a health risk assessment.
✔ Covered once every 12 months
Routine Physical Exam
Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
✘ Medicare doesn’t cover a routine physical
✘ Patients pay 100% out-of-pocket
Together we can advance health equity and help eliminate health disparities for all minority and underserved groups. Find resources and more from the CMS Office of Minority Health :
- Health Equity Technical Assistance Program
- Disparities Impact Statement
Communication Avoids Confusion
As a health care provider, you may recommend that patients get services more often than we cover or that we don’t cover. If this happens, help patients understand they may have to pay some or all costs. Communication is key to ensuring patients understand why you’re recommending certain services and whether we cover them.

Initial Preventive Physical Exam
The initial preventive physical exam (IPPE), also known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. We pay for 1 IPPE per lifetime if it’s provided within the first 12 months after the patient’s Part B coverage starts.
1. Review the patient’s medical and social history
At a minimum, collect this information:
- Past medical and surgical history (illnesses, hospital stays, operations, allergies, injuries, and treatments)
- Current medications, supplements, and other substances the person may be using
- Family history (review the patient’s family and medical events, including hereditary conditions that place them at increased risk)
- Physical activities
- Social activities and engagement
- Alcohol, tobacco, and illegal drug use history
Learn information about Medicare’s substance use disorder (SUD) services coverage .
2. Review the patient’s potential depression risk factors
Depression risk factors include:
- Current or past experiences with depression
- Other mood disorders
Select from various standardized screening tools designed for this purpose and recognized by national professional medical organizations. APA’s Depression Assessment Instruments has more information.
3. Review the patient’s functional ability and safety level
Use direct patient observation, appropriate screening questions, or standardized questionnaires recognized by national professional medical organizations to review, at a minimum, the patient’s:
- Ability to perform activities of daily living (ADLs)
- Hearing impairment
- Home and community safety, including driving when appropriate
Medicare offers cognitive assessment and care plan services for patients who show signs of impairment.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), blood pressure, balance, and gait
- Visual acuity screen
- Other factors deemed appropriate based on medical and social history and current clinical standards
5. End-of-life planning, upon patient agreement
End-of-life planning is verbal or written information you (their physician or practitioner) can offer the patient about:
- Their ability to prepare an advance directive in case an injury or illness prevents them from making their own health care decisions
- If you agree to follow their advance directive
- This includes psychiatric advance directives
6. Review current opioid prescriptions
For a patient with a current opioid prescription:
- Review any potential opioid use disorder (OUD) risk factors
- Evaluate their pain severity and current treatment plan
- Provide information about non-opiod treatment options
- Refer to a specialist, as appropriate
The HHS Pain Management Best Practices Inter-Agency Task Force Report has more information. Medicare now covers monthly chronic pain management and treatment services .
7. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them to treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
8. Educate, counsel, and refer based on previous components
Based on the results of the review and evaluation services from the previous components, provide the patient with appropriate education, counseling, and referrals.
9. Educate, counsel, and refer for other preventive services
Include a brief written plan, like a checklist, for the patient to get:
- A once-in-a-lifetime screening electrocardiogram (ECG), as appropriate
- Appropriate screenings and other covered preventive services
Use these HCPCS codes to file IPPE and ECG screening claims:
Initial preventive physical examination; face-to-face visit, services limited to new beneficiary during the first 12 months of medicare enrollment
Electrocardiogram, routine ecg with 12 leads; performed as a screening for the initial preventive physical examination with interpretation and report
Electrocardiogram, routine ecg with 12 leads; tracing only, without interpretation and report, performed as a screening for the initial preventive physical examination
Electrocardiogram, routine ecg with 12 leads; interpretation and report only, performed as a screening for the initial preventive physical examination
Federally qualified health center (fqhc) visit, ippe or awv; a fqhc visit that includes an initial preventive physical examination (ippe) or annual wellness visit (awv) and includes a typical bundle of medicare-covered services that would be furnished per diem to a patient receiving an ippe or awv
* Section 60.2 of the Medicare Claims Processing Manual, Chapter 9 has more information on how to bill HCPCS code G0468.
Report a diagnosis code when submitting IPPE claims. We don’t require you to use a specific IPPE diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an IPPE when performed by a:
- Physician (doctor of medicine or osteopathy)
- Qualified non-physician practitioner (physician assistant, nurse practitioner, or certified clinical nurse specialist)
When you provide an IPPE and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
CPT only copyright 2022 American Medical Association. All rights reserved.
IPPE Resources
- 42 CFR 410.16
- Section 30.6.1.1 of the Medicare Claims Processing Manual, Chapter 12
- Section 80 of the Medicare Claims Processing Manual, Chapter 18
- U.S. Preventive Services Task Force Recommendations
No. The IPPE isn’t a routine physical that some patients may get periodically from their physician or other qualified non-physician practitioner (NPP). The IPPE is an introduction to Medicare and covered benefits, and it focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV during their IPPE. The Social Security Act explicitly prohibits Medicare coverage of routine physical exams.
No. The IPPE and AWV don’t include clinical lab tests, but you may make appropriate referrals for these tests as part of the IPPE or AWV.
No. We waive the coinsurance, copayment, and Part B deductible for the IPPE (HCPCS code G0402). Neither is waived for the screening electrocardiogram (ECG) (HCPCS codes G0403, G0404, or G0405).
A patient who hasn’t had an IPPE and whose Part B enrollment began in 2023 can get an IPPE in 2024 if it’s within 12 months of the patient’s Part B enrollment effective date.
We suggest providers check with their MAC for available options to verify patient eligibility. If you have questions, find your MAC’s website .
Annual Wellness Visit Health Risk Assessment
The annual wellness visit (AWV) includes a health risk assessment (HRA). View the HRA minimum elements summary below. A Framework for Patient-Centered Health Risk Assessments has more information, including a sample HRA.
Perform an HRA
- You or the patient can update the HRA before or during the AWV
- Consider the best way to communicate with underserved populations, people who speak different languages, people with varying health literacy, and people with disabilities
- Demographic data
- Health status self-assessment
- Psychosocial risks, including, but not limited to, depression, life satisfaction, stress, anger, loneliness or social isolation, pain, suicidality, and fatigue
- Behavioral risks, including, but not limited to, tobacco use, physical activity, nutrition and oral health, alcohol consumption, sexual health, motor vehicle safety (for example, seat belt use), and home safety
- Activities of daily living (ADLs), including dressing, feeding, toileting, and grooming; physical ambulation, including balance or fall risks and bathing; and instrumental ADLs (IADLs), including using the phone, housekeeping, laundry, transportation, shopping, managing medications, and handling finances
1. Establish the patient’s medical and family history
At a minimum, document:
- Medical events of the patient’s parents, siblings, and children, including hereditary conditions that place them at increased risk
- Use of, or exposure to, medications, supplements, and other substances the person may be using
2. Establish a current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including behavioral health care.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), and blood pressure
- Other routine measurements deemed appropriate based on medical and family history
4. Detect any cognitive impairments the patient may have
Check for cognitive impairment as part of the first AWV.
Assess cognitive function by direct observation or reported observations from the patient, family, friends, caregivers, and others. Consider using brief cognitive tests, health disparities, chronic conditions, and other factors that contribute to increased cognitive impairment risk. Alzheimer’s and Related Dementia Resources for Professionals has more information.
5. Review the patient’s potential depression risk factors
6. Review the patient’s functional ability and level of safety
- Ability to perform ADLs
7. Establish an appropriate patient written screening schedule
Base the written screening schedule on the:
- Checklist for the next 5–10 years
- United States Preventive Services Task Force and Advisory Committee on Immunization Practices (ACIP) recommendations
- Patient’s HRA, health status and screening history, and age-appropriate preventive services we cover
8. Establish the patient’s list of risk factors and conditions
- A recommendation for primary, secondary, or tertiary interventions or report whether they’re underway
- Mental health conditions, including depression, substance use disorders , suicidality, and cognitive impairments
- IPPE risk factors or identified conditions
- Treatment options and associated risks and benefits
9. Provide personalized patient health advice and appropriate referrals to health education or preventive counseling services or programs
Include referrals to educational and counseling services or programs aimed at:
- Fall prevention
- Physical activity
- Tobacco-use cessation
- Social engagement
- Weight loss
10. Provide advance care planning (ACP) services at the patient’s discretion
ACP is a discussion between you and the patient about:
- Preparing an advance directive in case an injury or illness prevents them from making their own health care decisions
- Future care decisions they might need or want to make
- How they can let others know about their care preferences
- Caregiver identification
- Advance directive elements, which may involve completing standard forms
Advance directive is a general term that refers to various documents, like a living will, instruction directive, health care proxy, psychiatric advance directive, or health care power of attorney. It’s a document that appoints an agent or records a person’s wishes about their medical treatment at a future time when the individual can’t communicate for themselves. The Advance Care Planning fact sheet has more information.
We don’t limit how many times the patient can revisit the ACP during the year, but cost sharing applies outside the AWV.
11. Review current opioid prescriptions
- Review any potential OUD risk factors
- Provide information about non-opioid treatment options
12. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them for treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
13. Social Determinants of Health (SDOH) Risk Assessment
Starting in 2024, Medicare includes an optional SDOH Risk Assessment as part of the AWV. This assessment must follow standardized, evidence-based practices and ensure communication aligns with the patient’s educational, developmental, and health literacy level, as well as being culturally and linguistically appropriate.
1. Review and update the HRA
2. Update the patient’s medical and family history
At a minimum, document updates to:
3. Update current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including those added because of the first AWV personalized prevention plan services (PPPS), and any behavioral health providers.
- Weight (or waist circumference, if appropriate) and blood pressure
5. Detect any cognitive impairments patients may have
Check for cognitive impairment as part of the subsequent AWV.
6. Update the patient’s written screening schedule
Base written screening schedule on the:
7. Update the patient’s list of risk factors and conditions
- Mental health conditions, including depression, substance use disorders , and cognitive impairments
- Risk factors or identified conditions
8. As necessary, provide and update patient PPPS, including personalized health advice and appropriate referrals to health education or preventive counseling services or programs
9. Provide advance care planning (ACP) services at the patient’s discretion
10. Review current opioid prescriptions
11. Screen for potential substance use disorders (SUDs)
12. Social Determinants of Health (SDOH) Risk Assessment
Preparing Eligible Patients for their AWV
Help eligible patients prepare for their AWV by encouraging them to bring this information to their appointment:
- Medical records, including immunization records
- Detailed family health history
- Full list of medications and supplements, including calcium and vitamins, and how often and how much of each they take
- Full list of current providers and suppliers involved in their care, including community-based providers (for example, personal care, adult day care, and home-delivered meals), and behavioral health specialists
Use these HCPCS codes to file AWV claims:
Annual wellness visit; includes a personalized prevention plan of service (pps), initial visit
Annual wellness visit, includes a personalized prevention plan of service (pps), subsequent visit
Report a diagnosis code when submitting AWV claims. We don’t require you to use a specific AWV diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an AWV if performed by a:
- Medical professional (including health educator, registered dietitian, nutrition professional, or other licensed practitioner) or a team of medical professionals directly supervised by a physician
When you provide an AWV and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
You can only bill G0438 or G0439 once in a 12-month period. G0438 is for the first AWV, and G0439 is for subsequent AWVs. Don’t bill G0438 or G0439 within 12 months of a previous G0402 (IPPE) billing for the same patient. We deny these claims with messages indicating the patient reached the benefit maximum for the time period.
Medicare telehealth includes HCPCS codes G0438 and G0439.
ACP is the face-to-face conversation between a physician (or other qualified health care professional) and a patient to discuss their health care wishes and medical treatment preferences if they become unable to communicate or make decisions about their care. At the patient’s discretion, you can provide the ACP during the AWV.
Use these CPT codes to file ACP claims as an optional AWV element:
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure)
Report a diagnosis code when submitting an ACP claim as an optional AWV element. We don’t require you to use a specific ACP diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
We waive both the Part B ACP coinsurance and deductible when it’s:
- Provided on the same day as the covered AWV
- Provided by the same provider as the covered AWV
- Billed with modifier 33 (Preventive Service)
- Billed on the same claim as the AWV
We waive the ACP deductible and coinsurance once per year when billed with the AWV. If we deny the AWV billed with ACP for exceeding the once-per-year limit, we’ll apply the ACP deductible and coinsurance .
We apply the deductible and coinsurance when you deliver the ACP outside the covered AWV. There are no limits on the number of times you can report ACP for a certain patient in a certain period. When billing this service multiple times, document changes in the patient’s health status or wishes about their end-of-life care.
SDOH is important in assessing patient histories; in assessing patient risk; and in guiding medical decision making, prevention, diagnosis, care, and treatment. In the CY 2024 Medicare Physician Fee Schedule final rule , we added a new SDOH Risk Assessment as an optional, additional element of the AWV. At both yours and the patient’s discretion, you may conduct the SDOH Risk Assessment during the AWV.
Use this HCPCS code to file SDOH Risk Assessment claims as an optional AWV element:
Administration of a standardized, evidence-based social determinants of health risk assessment tool, 5-15 minutes
Report a diagnosis code when submitting an SDOH Risk Assessment claim as an optional AWV element. We don’t require you to use a specific SDOH Risk Assessment diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
The implementation date for SDOH Risk Assessment claims is July 1, 2024. We waive both the Part B SDOH Risk Assessment coinsurance and deductible when it’s:
We waive the SDOH Risk Assessment deductible and coinsurance once per year when billed with the AWV.
If we deny the AWV billed with SDOH Risk Assessment for exceeding the once-per-year limit, we’ll apply the deductible and coinsurance. We also apply the deductible and coinsurance when you deliver the SDOH Risk Assessment outside the covered AWV.
AWV Resources
- 42 CFR 410.15
- Section 140 of the Medicare Claims Processing Manual, Chapter 18
No. The AWV isn’t a routine physical some patients may get periodically from their physician or other qualified NPP. We don’t cover routine physical exams.
No. We waive the coinsurance, copayment, and Part B deductible for the AWV.
We cover an AWV for all patients who’ve had Medicare coverage for longer than 12 months after their first Part B eligibility date and who didn’t have an IPPE or AWV within those past 12 months. We cover only 1 IPPE per patient per lifetime and 1 additional AWV every 12 months after the date of the patient’s last AWV (or IPPE). Check eligibility to find when a patient is eligible for their next preventive service.
Generally, you may provide other medically necessary services on the same date as an AWV. The deductible and coinsurance or copayment applies for these other medically necessary and reasonable services.
You have different options for accessing AWV eligibility information depending on where you practice. Check eligibility to find when a patient is eligible for their next preventive service. Find your MAC’s website if you have specific patient eligibility questions.
Know the Differences
An IPPE is a review of a patient’s medical and social health history and includes education about other preventive services .
- We cover 1 IPPE per lifetime for patients within the first 12 months after their Part B benefits eligibility date
- We pay IPPE costs if the provider accepts assignment
An AWV is a review of a patient’s personalized prevention plan of services and includes a health risk assessment.
- We cover an annual AWV for patients who aren’t within the first 12 months after their Part B benefits eligibility date
- We cover an annual AWV 12 months after the last AWV’s (or IPPE’s) date of service
- We pay AWV costs if the provider accepts assignment
A routine physical is an exam performed without relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury.
- We don’t cover routine physical exams, but the IPPE, AWV, or other Medicare benefits cover some routine physical elements
- Patients pay 100% out of pocket
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure .
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Health & Human Services (HHS).
CPT codes, descriptions and other data only are copyright 2022 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
- NEW - Vaginal Microbiome
- A-Z - Shows ALL Tests
- Health Screens (POPULAR)
- Gut Microbiome
- Testosterone Profiles
- Thyroid Blood Tests
- - - - - - - - -
- Adrenal Fatigue blood tests
- B12 and Anaemia blood tests
- Female health blood tests
- Finger-Prick Health Screens
- Genetic Trait Testing
- Hormone blood tests
- Immunity Blood Testing
- Immunology blood tests
- Male health blood tests
- Nutritional blood tests
- Phlebotomy Extras and Upgrades
- Pregnancy Blood Tests
- Sexual health blood tests
- Sport performance blood testing
- Basingstoke
- Bury St Edmunds
- Cheshire Oaks (Ellesmere Port)
- Chester Broughton
- Clifftonville
- Denton Crown Point
- Huddersfield
- Milton Keynes
- New! Membership
- About Finger-Prick Testing
- About Nurse Home Visits
- Frequently asked questions
- Pathology Points
- Discount Codes
- Our Laboratories
- Our other services
- Practitioner Information
- Corporate Testing Solutions
- Blood Test News
- 8 Postal Guarantees
- Charities we work with
- Terms and Conditions
Sign up and save
Entice customers to sign up for your mailing list with discounts or exclusive offers. Include an image for extra impact.
Nurse home visit service
Our nurses can visit you at your home or place of work to take your blood quickly, conveniently and professionally. All nurses are registered with the NMC and are a minimum Band 5 - simply choose the tests that you need, and select a nurse home visit at checkout. We charge a nominal fee of £55 for this extra service which is very convenient for those without the ability to travel to a clinic.
Once you have placed an order for your required blood tests online, selecting a nurse home visit as your collection option in checkout, we will send you out the relevant blood test kit by post. If you have supplied us with your mobile telephone number we will also send you a text message to confirm that we have passed your details to your local nurse.

Nurse Visit Procedure - How it Works
First contact.
The nurse will attempt to contact you in the following days after you confirm patient details and they will try to arrange a mutually convenient time to meet at your home or place of work to take your blood. A confirmation will also be sent to you by text message, along with a reminder text, generally the day before. Appointments will be made when a mutually convenient slot can be agreed on by yourself and the nurse. The lead time is on average about a week, but will depend upon factors such as current workload and geographical constraints.
We recommend Monday to Wednesday appointments, but see below for more details about Posting the Sample to the Laboratory.
Nurse Arrival
When you nurse arrives your blood will be taken professionally, and in some circumstances the nurse may also be able to post your blood to our Laboratory for you in a standard postbox, although if you wish to use a next day delivery service you will have to take it to the post office yourself.
You'll likely be asked for Photo-ID, so if you have a Passport or a Driving License Please have it ready.
Is Success Guaranteed?
A successful blood draw is not guaranteed - although each of the contract nurses that Blue Horizon use has been picked for their phlebotomy skills, blood draw can often be problematic (even in a hospital environment for instance). If the nurse fails to successfully take a sample you will not be charged.
We can either refund you in full for the Kit and the Phlebotomy Appointment, or you can choose to request another appointment. Although you don’t have to pay for this, in the event of a second collection failure you will not get the phlebotomy portion of your total payment refunded.
Posting Your Sample Back to The Laboratory.
It is your reponsibility to post the sample back in the supplied envelope to the Laboratory if your Nurse draws a successful sample - but when do I post it and should I upgrade to a Guaranteed Next Day Service at my own expense??
The Sample Should Be Taken on a Monday, Tuesday or Wednesday and Sent back to the Laboratory Using the Supplied Royal Mail Tracked 24 Envelope. Although it is not guaranteed, the Sample will usually arrive the next day – find a Priority Post-box if you can. If you want more reassurance then you should upgrade at your local Post Office to a Next Day Return Service at your own cost, in which case you can also send on a Thursday. As this is a Royal Mail Service you should factor in strikes, Bank Holidays and the lead up to Christmas in your personal assessment of needing to upgrade.
The Sample for this Test MUST arrive in the Laboratory the next day as delay may result in sample degradation. Take Sample on a Monday, Tuesday, Wednesday or Thursday and Post it on the Same Day. You will need to upgrade at your local Post Office to a Next Day Return Service at your own cost. As this is a Royal Mail Service you should factor in strikes, Bank Holidays and the lead up to Christmas in your personal assessment of when to send.
The Sample is Extremely Stable for many days. You are able to send using the supplied return envelope on any day of the week, although if you wish to upgrade to enable faster results or to take advantage of tracking then you may do so at your own cost. As this is a Royal Mail Service you should factor in strikes, Bank Holidays and the lead up to Christmas in your personal assessment of when to send.
Dr Johnson's Blood Test News

If this is the first time using our service and you're a little unsure as to how it works, please read this section, or contact us for further information.

Over half of our blood test requests are from repeat patients - find out here why our patients keep using Blue Horizon.

We're a small but mighty medical team committed to providing you with a personal private pathology service.

- No products in the cart.
Phlebotomy Home Visit for Patients
Do you or someone you know need a blood sample taker (known as a phlebotomist) to perform a blood test at home, or somewhere that suits you .
- Open access
- Published: 25 April 2024
Improving diagnostics using extended point-of-care testing during in-home assessments of older adults with signs of emerging acute disease: a prospective observational non-randomised pilot and feasibility study
- Siri Aas Smedemark 1 , 2 ,
- Christian B. Laursen 2 , 3 ,
- Dorte Ejg Jarbøl 4 ,
- Flemming S. Rosenvinge 5 , 6 &
- Karen Andersen-Ranberg 1 , 2
BMC Geriatrics volume 24 , Article number: 373 ( 2024 ) Cite this article
Delayed recognition of acute disease among older adults hinders timely management and increases the risk of hospital admission. Point-of-Care testing, including Focused Lung Ultrasound (FLUS) and in-home analysis of biological material, may support clinical decision-making in suspected acute respiratory disease. The aim of this study was to pilot test the study design for a planned randomised trial, investigate whether in-home extended use of point-of-care testing is feasible, and explore its’ potential clinical impact.
A non-randomised pilot and feasibility study was conducted during September–November 2021 in Kolding Municipality, Denmark. A FLUS-trained physician accompanied an acute community nurse on home-visits to citizens aged 65 + y with signs of acute respiratory disease. The acute community nurses did a clinical assessment (vital signs, capillary C-reactive protein and haemoglobin) and gave a presumptive diagnosis. Subsequently, the physician performed FLUS, venipuncture with bedside analysis (electrolytes, creatinine, white blood cell differential count), nasopharyngeal swab (PCR for upper respiratory pathogens), and urine samples (flow-cytometry). Primary outcomes were feasibility of study design and extended point-of-care testing; secondary outcome was the potential clinical impact of extended point-of-care testing.
One hundred consecutive individuals were included. Average age was 81.6 (SD ± 8.4). Feasibility of study design was acceptable, FLUS 100%, blood-analyses 81%, PCR for upper respiratory pathogens 79%, and urine flow-cytometry 4%. In addition to the acute community nurse’s presumptive diagnosis, extended point-of-care testing identified 34 individuals with a condition in need of further evaluation by a physician.
Overall, in-home assessments with extended point-of-care testing are feasible and may aid to identify and handle acute diseases in older adults.
Peer Review reports
The population of older adults is increasing, and healthcare sectors worldwide face capacity challenges [ 1 ]. In Denmark, acute community healthcare services (ACHCS) were established in 2018 to carry out initial in-home clinical assessments of vulnerable citizens suspected of emerging acute diseases. The purpose was to support early decision-making and triage to reduce the number of avoidable admissions and the pressure on the secondary healthcare sector [ 2 ]. However, diagnosing older adults is challenging as they may present with vague symptoms, e.g., coughing is a less prominent symptom in pneumonia [ 3 ], or atypical symptoms e.g., functional decline, delirium, and falls [ 4 , 5 ]. Delayed recognition of disease prevents timely management and increases the risk of hospital admission [ 6 ].
Point-of-care testing (POCT) is carried out bedside or near the patient, i.e., in-home [ 7 ], and increases timely diagnosis and decision-making in emergency departments and in primary care [ 8 ]. C-Reactive Protein (CRP), haemoglobin, international normalised ratio (INR), urine test strips, and blood glucose testing are widely implemented in primary care [ 9 ]. In recent years, new POCTs have been developed, such as white blood cell (WBC) differential count, hand-held point-of-care ultrasound, and urine flow-cytometry, but the tests are still not widely implemented in primary care nor validated among older adults [ 10 , 11 , 12 ]. The Danish ACHCSs use POCT for CRP and haemoglobin on capillary blood, but given the challenges of diagnosing older adults, a comprehensive approach is needed with additional clinical assessment, biochemical results, and imaging modalities [ 6 ]. By introducing extended POCT (ExtPOCT) during in-home assessment, we hypothesize that ExtPOCT improves diagnostic work-up and supports the primary care physicians’ clinical decision-making.
Prior to a planned randomised controlled trial (RCT), the primary objective was to investigate whether ExtPOCT during in-home assessments among older adults was feasible, and, secondly, to pilot-test the study design including the intervention consisting of ExtPOCT, defined by Focused Lung Ultrasound (FLUS) and in-home analysis of biological material (blood, nasopharyngeal swab, urine).
The secondary objective was to explore whether ExtPOCT had potential clinical impact by identifying conditions in need of clinical decision-making not identified by usual in-home assessments.
Trial design
This study was conducted as a prospective observational non-randomised pilot and feasibility study, adhering to the guidelines outlined by the CONSORT 2010 statement: extension to randomised pilot and feasibility studies [ 13 , 14 ].
Study setting
The study was conducted in 2021 from September 1 st to December 1 st , in Kolding Municipality, Denmark, covering an area of 604.5 km 2 with 93,161 inhabitants (65 + year olds: 18,453) [ 15 ]. The pilot study was conducted in collaboration with the ACHCS in Kolding Municipality.
The ACHCS is operated by acute community nurses (ACNs) trained in in-home assessment including vital signs and POCT for C-Reactive Protein (CRP) and haemoglobin on capillary blood ( usual care) [ 2 ]. All clinical information is communicated to the primary care physician (PCP) to support clinical decision-making. In-home assessment is performed after referral from PCPs or home care service personnel when an acute condition in vulnerable citizens is suspected and can be carried out at the place of residence, i.e., in own home, care home, or skilled nursing facility. Approximately five patients are referred each day to the ACHCS for an in-home assessment. Hospital physicians refer patients for in-home treatment with intravenous antibiotics carried out by ACNs.
Study participants
Participants eligible for this study were adults aged 65 years or older, referred to the ACHCS in Kolding Municipality for an acute in-home assessment, irrespective of their status as home care recipients or their place of residence, including own home, a care home, or a skilled nursing facility.
The participants had at least one of the following inclusion criteria: Cough, dyspnoea, fever (≥ 38 °C), chest pain, fall, or functional decline, defined as either subjective (not able to perform normal daily activities) or objective functional decline (increased need of home care service). Fall and functional decline are usually not perceived as symptoms of worsened or acute respiratory disease, but are known as atypical disease presentations [ 4 , 5 ]. Participants with known moderate to severe cognitive impairment were excluded from the study, due to Danish legislation and recommendations from the Regional Committees on Health Research Ethics for Southern Denmark.
A convenience sample of 100–150 participants was chosen to investigate feasibility and potential clinical impact. The pilot-study should not exceed 3 months, as inclusion rate was part of the feasibility assessment.
Intervention
The intervention was an add-on to the ACNs’ usual in-home assessment and included hand-held FLUS, biochemical analysis on venous blood samples, and microbiological analysis of nasopharyngeal swabs and urine samples (Fig. 1 ).
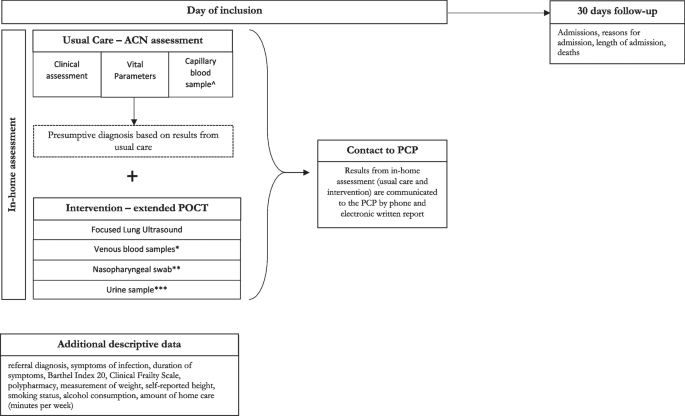
Overview of examination program and data collection. ^ POCT on capillary blood samples for C-reactive protein and Hemoglobin (using Quick-read PRO). *POCT on venous blood samples for creatinine and electrolytes (using i-STAT ®), and for Leucocytes with differential count (using Hemocue® WBF DIFF System). **POCT on nasopharyngeal swabs for 22 different viral and bacterial pathogens (using BioMérieux BioFire ® FilmArray ® Respiratory Panel 2.1). ***POCT on urine samples for flow-cytometry (using Sysmex UF-5000 ®). Abbreviations: ACN: Acute Community Nurse, POCT: Point-of-care Testing, PCP: Primary Care Physician, PCR: Polymerase chain reaction
FLUS examination was performed using a hand-held ultrasound scanner in the form of a Lumify® C5-2 Curved Array Transducer (Philips Medical Systems, Bothell, WA) (5–2 MHz, scan depth up to 30 cm) connected by USB-C to a FuturePAD® FPZ10-A tablet (CONCEPT International GmbH, Munich Germany). The standard Philips Lumify App version 4.0.1 software and its dedicated lung-preset was installed on the tablet and used for the examination. FLUS followed a standardised 14 scanning zone protocol using predefined questions regarding pneumothorax, pleural effusion, interstitial syndrome, and other obvious pathology [ 16 , 17 ].
Blood-samples were collected by venipuncture and analysed immediately during in-home assessment. Blood samples for creatinine and electrolytes (collected in lithium/heparin vacutainers) were analysed using CHEM8+ cassettes on i-STAT® (Abbott, Inc., NJ, U.S.A.). WBC differential count (collected in EDTA-vacutainers) was analysed using HemoCue® WBF DIFF System (HemoCue AB, Ängelholm, Sweden) with dedicated micro-cuvettes.
Nasopharyngeal swabs and urine samples were collected during in-home assessment, and carried to Hospital Lillebaelt, Kolding, within 2 h. Nasopharyngeal swabs were analysed on the BioMérieux BioFire ® FilmArray ® Respiratory Panel 2.1 (RP2.1) (BioFire Diagnostics, Salt Lake City, UT, USA). The BioFire ® FilmArray ® RP2.1 targets 22 respiratory pathogens [ 18 ]. Urine samples were analysed on urine flow-cytometer Sysmex UF-5000 ® (Sysmex Corporation, Kobe, Japan).
Feasibility was evaluated based on several criteria, including the average inclusion rate, acceptability of the intervention, and the utilization of ExtPOCT. The average inclusion rate was considered feasible if at least two participants a day, 4 days a week, were enrolled in the study. The acceptability of the intervention was determined by assessing the number participants who declined participation and by assessing the acceptance of the results from ExtPOCT by PCPs. Additionally, the feasibility of ExtPOCT and collection of other biological material during in-home assessment was defined and calculated as the percentage of completed examinations. The intervention procedure (ExtPOCT) was considered feasible if used in > 80% of participants.
To assess the potential clinical impact of ExtPOCT, we predefined specific conditions in participants that necessitated clinical decision-making by the PCP based on usual care results, and subsequently compared these with the findings from ExtPOCT. Conditions requiring clinical decision-making were defined as instances necessitating treatment initiations or adjustments (e.g., antibiotics, diuretics, or inhalation therapy), hospital admission, or increased need for home care. The identification of participants with conditions requiring further clinical decision-making, which were not detected by usual in-home assessment conducted by ACNs, was considered indicative of potential clinical impact of ExtPOCT.
The registration of conditions requiring clinical decision-making was derived by using predefined cut-offs and international standardised agreements [ 16 , 17 , 19 , 20 , 21 , 22 ]. Conditions identified by ExtPOCT were: Pneumothorax, pleural effusion, interstitial syndrome, pneumonia, elevated leucocytes (> 11*10 9 /L), elevated creatinine (> 150 µmol/L), abnormal electrolytes (K + : < 3 mmol/L or > 5 mmol/L, Na + : < 125 mmol/L or > 145 mmol/L), positive PCR for upper respiratory tract pathogens, positive urine flow-cytometry (> 10 5 BACT/ml).
Data collection
An overview of the data collection and examination program is illustrated in Fig. 1 .
The primary investigator, a physician certified and trained in thoracic ultrasound corresponding to European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) thoracic ultrasound competency level 1, accompanied the ACNs during in-home assessment [ 23 ]. The usual in-home assessment was made by the ACNs, after which the ACNs noted a presumptive diagnosis and whether a clinical decision by a physician was required. Subsequently the primary investigator performed ExtPOCT.
All results from the usual care and ExtPOCT were communicated by the ACN to the participants PCP both by telephone and by written electronic communication.
The primary investigator collected descriptive data from all study participants during the in-home assessment (Fig. 1 ), including symptoms, symptom duration, height, smoking status, and alcohol consumption. Functional level was assessed using the Barthel Index 20, while frailty among participants was evaluated using the Clinical Frailty Scale, both of which were assessed using validated Danish-translated assessment scales [ 24 , 25 ]. Additional data on the amount of home care received by participants was extracted from the municipal Electronic Social Care Record. Polypharmacy, defined as the use of 5 or more medications per day, was assessed using the Shared Medication Record (In Danish: FMK – Fælles Medicin Kort), a nationwide digital database at the Danish Health Data Authority, storing data on all Danish citizens’ current medication plans, electronic prescriptions, and medicine purchases [ 26 ].
The hospital Electronic Patient Journal (EPJ) was accessed after 30 days to register admissions, reasons for admission, length of admission, and deaths, as these variables are primary and secondary outcomes for the planned RCT. Adverse events and harms were also registered and served as safety assessment of the intervention.
Statistical methods
We used descriptive statistics to present demographic and baseline characteristics. Categorical data was reported as number and percentage. Continuous data was reported as means (SD), medians [IQR], and range. The primary outcome was assessed by calculating inclusion-rate, number of declining participants, and number of contacts to the PCPs. The feasibility of ExtPOCT was calculated as the percentage of completed examinations. The secondary outcome was reported as the number of participants in need of clinical decision-making not identified by the ACNs usual in-home assessment. All statistical analyses were carried out using STATA version 16 software (StataCorp LLC, Texas, USA).
Inclusion-flow
Totally, 139 older adults were assessed for eligibility during the study period, of which 35 could not be included due to cognitive impairment, two declined, and two required urgent hospitalisation, thereby including 100 participants in the study. For details, see Fig. 2 . Inclusion rate was 2.08 participants per day, 4 days a week, for 3 months. All participants were followed for 30 days.
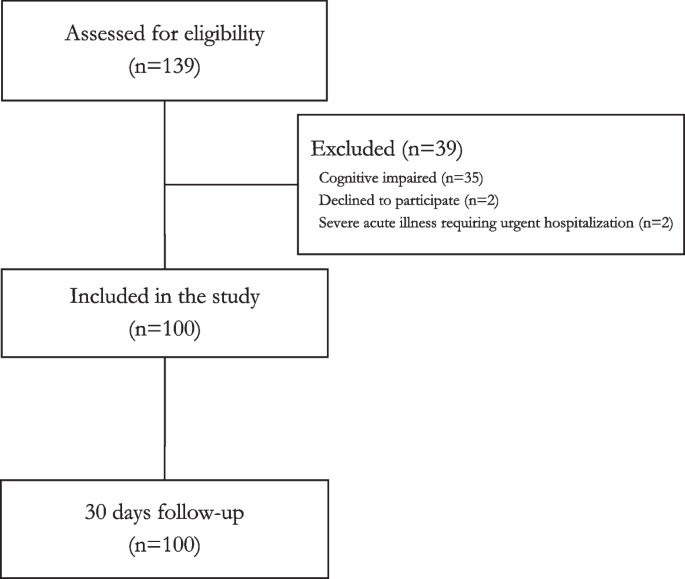
Study population
Mean age of included participants was 81.6 years (SD ± 8.4) and 54% were female. Most assessments were carried out in the participants own home (86%), of whom 71% received home care. The prevalence of polypharmacy (> 5 medications daily) was high (95%). Median Clinical Frailty Scale level was 5 (range 1–9). Less than four participants had chest pain. For details, see Table 1 .
Usual in-home assessment
The ACNs carried out in-home assessment in all participants. Median values of vital signs are shown in Table 2 . Median value of CRP and haemoglobin was 24 mg/L (IQR 5.3–57) and 7.4 mmol/L (IQR 6.6–8.1), respectively. ACNs presumptive diagnoses based on results from the usual in-home assessment suggested that 48 participants had conditions requiring clinical decision-making by a physician. The suggested diagnoses and conditions were pneumonia ( n = 20), acute exacerbation of chronic obstructive pulmonary disease ( n = 15), infection but unclear focus ( n = 6), urinary tract infection ( n = 5), and other ( n < 3). For details, see Table 2 .
Intervention – ExtPOCT
FLUS was performed in all participants (100%), venous blood-samples in 81%, nasopharyngeal swabs in 79%, and urine samples in 4%. Reasons for missing venous blood samples were practical difficulties in obtaining a blood sample. Reasons for missing nasopharyngeal swabs were acute admissions, and urine samples were missing due to permanent catheters (27%) or participants unable to provide a urine sample (73%) during the in-home assessment.
ExtPOCT identified additional 34 participants with acute conditions requiring clinical decision-making by a physician. This is illustrated in Fig. 3 . FLUS alone identified additional conditions in 21 participants needing further clinical decision-making by a physician: Pneumothorax, interstitial syndrome, moderate to large pleural effusions, and pneumonia. A significantly elevated creatinine (> 150 µmol/L) supporting a diagnosis of dehydration was identified in nine participants, which was not identified in the usual in-home assessment. Elevated WBC differential counts were identified in 16 participants, not suspected to have a bacterial infection in the usual in-home assessment. PCR for respiratory pathogens identified less than three viral infections. Only few urine samples were collected, and the potential clinical impact is therefore uncertain.
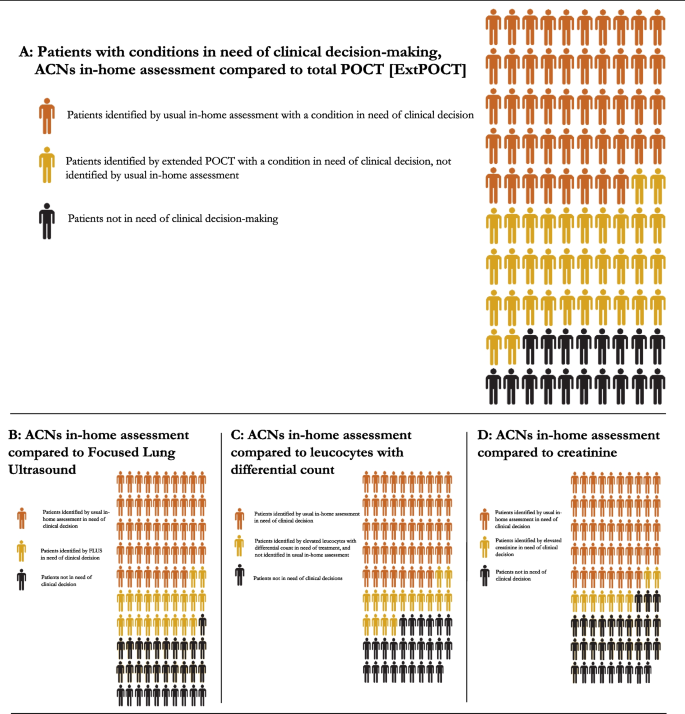
Potential clinical impact of extended point-of-care testing. Extended point-of-care testings’ potential for clinical impact by identifying additional participants with conditions in need of clinical decision-making compared to usual in-home assessments. A ACNs identified 48 out of 100 participants in need of clinical decision-making by a primary care physician. Extended POCT identified additional 34 participants with a condition in need of clinical decision-making, not identified by the usual in-home assessment. Each specific POCT is illustrated in B , C , D , except for PCR for upper respiratory tract infection and urine flow-cytometry, as results did not change clinical decision-making: B Focused Lung ultrasound identified 21 participants with a condition in need of clinical decision-making not identified by the ACNs in-home assessment. (Feasibility 100%). C POCT for leucocytes with differential count identified 16 participants with a condition in need of clinical decision-making not identified by the ACNs in-home assessment. (Feasibility 89%). D POCT for creatinine identified 9 participants with a condition in need of clinical decision-making not identified by the ACNs in-home assessment. (Feasibility 89%). Abbreviations: ACN: Acute Community Nurse, ExtPOCT: Extended point-of-care testing, FLUS: Focused Lung Ultrasound, POCT: Point-of-care Testing, PCR: Polymerase chain reaction
Healthcare contacts
In 62 of the in-home assessments, the PCP was contacted on the day of the visit directly by phone, and in 77% of the cases, the contact led to initiation of treatment, mainly oral antibiotics (37%), diuretics (6%), or hospital admission (21%). In total 42 participants (55 admissions) were admitted to hospital from the day of inclusion to 30 days follow-up. Median duration of hospital admission was 5 days (IQR 2–8).
Adverse events
No adverse events were reported to or observed by the research team. In total, 11 deaths occurred, and most deaths took place in hospital ( n = 7).
Key results and interpretation
The overall study design and use of ExtPOCT during in-home assessment of older adults were feasible. Our results suggest that FLUS and POCT on venous blood might supplement the usual in-home assessment of older adults suspected of acute respiratory disease by identifying additional conditions - potentially facilitating diagnostic work-up and early treatment.
The study design of the planned RCT has been modified based on the insights gained from the pilot study. As a result, the inclusion criteria were revised, which involved omitting chest as an eligibility symptom. This adjustment was informed by the observation that very few participants presented with chest pain. It is also important to note that in Denmark, chest pain as a standalone symptom typically warrants acute admission regardless of other factors. Therefore, including chest pain as a criterion in our study was deemed potentially confounding, and it was decided to exclude chest pain as a specific inclusion criterion for our study. We also omitted nasopharyngeal swab for PCR for upper respiratory pathogens and urine flow-cytometry from the intervention as explained in the following sections.
FLUS had the highest feasibility and did provide additional information to the clinical decision making. These findings are in line with other studies, showing that FLUS identifies missed conditions in need of treatment [ 16 , 27 , 28 ]. In general, only few studies on the use of FLUS have been conducted in primary care [ 29 ]. A recent study conducted in primary care investigated lung ultrasound performed by PCPs in patients suspected of community-acquired pneumonia found a higher prevalence of pneumonia compared to our findings (53% vs 25%) [ 30 ]. However, they used more specific inclusion criteria for community-acquired pneumonia, and patients were younger (median age of 47 vs 81.6 years). Only one participant in our study had classic dynamic bronchoaerograms, whereas most participants with pneumonia had unspecific findings with a thickened, fragmented visceral pleura, smaller sub-pleural consolidations, and focal B-lines [ 19 ]. Another notable finding from FLUS was pleural effusions: The identified moderate to large pleural effusions were among individuals without classic respiratory symptoms, but functional decline. In conclusion, FLUS is highly feasible, could have clinical impact, and will remain part of the intervention in the planned RCT.
Elevated creatinine level led to initiation of treatment or hospital admission in cases not identified by usual in-home assessment. Elevated leucocytes > 11*10 9 /L were interpreted as sign of bacterial infection, although cut-off points on different biomarkers of inflammation in older multimorbid adults have not reached international consensus and/or are still not validated [ 10 , 11 , 31 ]. In addition, systematic reviews and prospective studies have shown that older adults differ in biochemical presentation compared to younger adults [ 32 , 33 , 34 ]. This highlights the need for further research in diagnosing infections in older adults. Due to high feasibility and potential clinical impact, we chose to keep both creatinine, electrolytes, and WBC differential count in the planned RCT.
Nasopharyngeal swabs were feasible to collect, but PCR for upper respiratory pathogens did not add to the clinical decision-making. During the study period, rates of viral respiratory tract infections were very low probably as a consequence of general restrictions and recommendations to reduce and contain the COVID-19 pandemic in Denmark [ 35 ]. Because of the possible low number of positive samples, the uncertain clinical impact, and the high cost, POCT PCR was omitted from the RCT.
Urine samples were difficult to collect as many participants had catheters or were unable to provide a urine sample during the in-home assessment. Hence, the added clinical value of urine analysis is unknown and urine flow-cytometry is therefore excluded from the RCT.
The high rate of hospital admissions during the 30 days follow-up highlights the need for early detection of suspected disease in older adults. ExtPOCT might have added to the high rate by detecting pathologies in need of hospital admissions e.g., large pleural effusions. Additionally, ExtPOCT may yield false positive findings, or unclear results leading to unnecessary contacts to the secondary healthcare sector. However, it also has potential for early, relevant treatment decisions to prevent clinical deterioration and subsequent functional decline. Our planned RCT aims to investigate the effect of ExtPOCT on specific healthcare outcomes such as hospital admissions, in-hospital length of stay, and mortality, thereby addressing the effect of ExtPOCT on hospital admissions.
POCT for CRP, haemoglobin, blood glucose, and urine test strips, are widely implemented in primary care, but there is limited evidence of using other POCT in primary care especially among older adults and during in-home assessments [ 10 , 11 , 36 ]. A recent study from Germany highlighted that many PCPs rated only a limited number of POCT as useful [ 37 ], but without explaining why. Barriers towards POCT among PCPs, e.g., low economic benefit, over-reliance, increased risk of over-treatment, over-diagnostics, and unnecessary hospital admissions, can hinder implementations. We therefore plan to explore how citizens, ACNs, and PCPs experience ExtPOCT during in-home assessment, in a user-perspective evaluation after completion of the planned RCT.
Generalisability
The study sample was older adults with high rates of polypharmacy, frailty, and home-care dependency – a group of older adults who are at increased risk of hospital admission, and similar to the study population we aim to include for our planned RCT [ 1 , 38 ].
The ACHCS setup is common in Scandinavia, though organised differently between countries and municipalities [ 39 ]. Results from the present pilot-study and the planned RCT might not be applicable in other countries than Denmark, but the concept is applicable: By increasing competencies, e.g., introducing in-home POCT, to healthcare professionals caring for frail older adults, timely clinical decisions may be facilitated.
Limitations
Our study is classified as a pilot and feasibility study, as it aims to assess both the feasibility of the intervention and its potential clinical impact. Although our study lacked randomisation, we aimed to pilot-test the intervention and explore our hypothesis that ExtPOCT had potential to enhance the diagnostic work-up. Acceptability of the intervention was utilized as an outcome measure to assess feasibility. While acceptability traditionally focuses on participants’ and stakeholders’ attitudes towards an intervention, data collection process, or randomization, we followed the approach advocated by Eldridge et al. to explore acceptability as a means of informing the feasibility of a larger RCT [ 14 ]. Therefore, we utilized acceptability as a measure of feasibility to evaluate whether the intervention could be effectively implemented in a future RCT.
We had to exclude participants with cognitive impairment, and therefore we do not know whether ExtPOCT is feasible or have potential clinical impact in the diagnostic work-up among older adults with cognitive impairment.
We are well aware that it is not possible for us to determine the causal effect of ExtPOCT on clinical impact, and we do not have a final diagnosis on all participants. However, it was important to explore the potential clinical impact prior to the RCT: If the usual in-home assessments carried out by ACNs can identify most conditions in need of clinical decision-making, ExtPOCT is redundant.
The primary investigator performed ExtPOCT. Prior to the planned RCT, ACNs will complete an extensive training programme for collecting venous blood samples, handling POCT, and performing FLUS, and subsequently carry out ExtPOCT during the RCT.
Conclusions
The overall study design for the planned RCT is feasible, and in-home blood analyses and FLUS have a potential clinical impact by identifying acute conditions earlier in the diagnostic process, which suggests a potential for improving clinical decision-making during in-home assessment among older adults.
Availability of data and materials
The dataset generated and analysed during the current study is available from the corresponding author on reasonable request.
Abbreviations
Acute community healthcare service
Acute community nurse
Clinical Frailty Scale
C-reactive protein
Extended Point-of-care testing, including a focused lung ultrasound scan (FLUS), biochemical analysis on venous blood samples, and microbiological analysis of nasopharyngeal swabs and urine samples
Focused lung ultrasound scan
General Data Protection Regulation
International Normalised Ratio
Open Patient data Explorative Network
Polymerase chain reaction
Point-of-care
- Point-of-care testing
Randomised controlled trial
White blood cells
Oksuzyan A, Höhn A, Krabbe Pedersen J, Rau R, Lindahl-Jacobsen R, Christensen K. Preparing for the future: the changing demographic composition of hospital patients in Denmark between 2013 and 2050. PLoS One. 2020;15:e0238912.
Article CAS PubMed PubMed Central Google Scholar
Sundhedsstyrelsen. Kvalitetsstandarder for kommunale akutfunktioner i hjemmesygeplejen - krav og anbefalinger til varetagelse af særlige sygeplejeindsatser. Sundhedsstyrelsen; 2017. https://www.sst.dk . Accessed 3 Mar 2020.
Schoevaerdts D, Sibille FX, Gavazzi G. Infections in the older population: what do we know? Aging Clin Exp Res. 2021;33:689–701.
Article PubMed Google Scholar
Harper C, Newton P. Clinical aspects of pneumonia in the elderly veteran. J Am Geriatr Soc. 1989;37:867–72.
Article CAS PubMed Google Scholar
Berman P, Hogan DB, Fox RA. The atypical presentation of infection in old age. Age Ageing. 1987;16:201–7.
Struyf T, Boon HA, van de Pol AC, Tournoy J, Schuermans A, Verheij TJM, et al. Diagnosing serious infections in older adults presenting to ambulatory care: a systematic review. Age Ageing. 2021;50:405–14.
Schols AMR, Dinant GJ, Hopstaken R, Price CP, Kusters R, Cals JWL. International definition of a point-of-care test in family practice: a modified e-Delphi procedure. Fam Pract. 2018;35:475–80.
Rooney KD, Schilling UM. Point-of-care testing in the overcrowded emergency department–can it make a difference? Crit Care. 2014;18:692.
Article PubMed PubMed Central Google Scholar
Howick J, Cals JWL, Jones C, Price CP, Plüddemann A, Heneghan C, et al. Current and future use of point-of-care tests in primary care: an international survey in Australia, Belgium, The Netherlands, the UK and the USA. BMJ Open. 2014;4:e005611.
Boere TM, Hopstaken RM, van Tulder MW, Schellevis FG, Verheij TJM, Hertogh C, et al. Implementation and use of point-of-care C-reactive protein testing in nursing homes. J Am Med Dir Assoc. 2021;23(6):968–975.e3.
Smedemark SA, Aabenhus R, Llor C, Fournaise A, Olsen O, Jørgensen KJ. Biomarkers as point-of-care tests to guide prescription of antibiotics in people with acute respiratory infections in primary care. Cochrane Database Syst Rev. 2022;10:Cd010130.
PubMed Google Scholar
Nadim G, Laursen CB, Pietersen PI, Wittrock D, Sørensen MK, Nielsen LB, et al. Prehospital emergency medical technicians can perform ultrasonography and blood analysis in prehospital evaluation of patients with chronic obstructive pulmonary disease: a feasibility study. BMC Health Serv Res. 2021;21:290.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239.
Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLoS One. 2016;11:e0150205.
Statistics Denmark. FOLK1A: population at the first day of the quarter by region, sex, age and marital status. Statistics Denmark; 2022. www.statistikbanken.dk/FOLK1A . Accessed 2 Mar 2022.
Laursen CB, Sloth E, Lambrechtsen J, Lassen AT, Madsen PH, Henriksen DP, et al. Focused sonography of the heart, lungs, and deep veins identifies missed life-threatening conditions in admitted patients with acute respiratory symptoms. Chest. 2013;144:1868–75.
Laursen CB, Sloth E, Lassen AT, Christensen R, Lambrechtsen J, Madsen PH, et al. Point-of-care ultrasonography in patients admitted with respiratory symptoms: a single-blind, randomised controlled trial. Lancet Respir Med. 2014;2:638–46.
Biomérieux. The BioFire® Respiratory 2.1 (RP2.1) Panel. Biomérieux; 2021. https://www.biofiredx.com/products/the-filmarray-panels/filmarrayrp . Accessed 5 May 2023.
Laursen CB, Clive A, Hallifax R, Pietersen PI, Asciak R, Davidsen JR, et al. European Respiratory Society statement on thoracic ultrasound. Eur Respir J. 2021;57(3):2001519.
Rustad P, Felding P, Franzson L, Kairisto V, Lahti A, Mårtensson A, et al. The Nordic Reference Interval Project 2000: recommended reference intervals for 25 common biochemical properties. Scand J Clin Lab Invest. 2004;64:271–84.
Yahav D, Schlesinger A, Daitch V, Akayzen Y, Farbman L, Abu-Ghanem Y, et al. Presentation of infection in older patients—a prospective study. Ann Med. 2015;47:354–8.
Riley LK, Rupert J. Evaluation of patients with leukocytosis. Am Fam Physician. 2015;92:1004–11.
European Federation of Societies for Ultrasound in Medicine and Biology. Minimum training requirements for the practice of medical ultrasound in Europe. EFSUMB; 2008. https://efsumb.org/wp-content/uploads/2020/12/2009-04-14apx11.pdf . Accessed 4 Aug 2023.
Nissen SK, Fournaise A, Lauridsen JT, Ryg J, Nickel CH, Gudex C, et al. Cross-sectoral inter-rater reliability of the clinical frailty scale - a Danish translation and validation study. BMC Geriatr. 2020;20:443.
Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10:61–3.
The Danish Health Data Authority. Digital health solutions 2021. https://sundhedsdatastyrelsen.dk/da/english/digital_health_solutions . Accessed 16 Feb 2024.
Weile J, Laursen CB, Frederiksen CA, Graumann O, Sloth E, Kirkegaard H. Point-of-care ultrasound findings in unselected patients in an emergency department -results from a prospective observational trial. BMC Emerg Med. 2018;18:60.
Goffi A, Pivetta E, Lupia E, Porrino G, Civita M, Laurita E, et al. Has lung ultrasound an impact on the management of patients with acute dyspnea in the emergency department? Crit Care. 2013;17:R180.
Sorensen B, Hunskaar S. Point-of-care ultrasound in primary care: a systematic review of generalist performed point-of-care ultrasound in unselected populations. Ultrasound J. 2019;11:31.
Rodríguez-Contreras FJ, Calvo-Cebrián A, Díaz-Lázaro J, Cruz-Arnés M, León-Vázquez F, del Carmen L-A, et al. Lung ultrasound performed by primary care physicians for clinically suspected community-acquired pneumonia: a multicenter prospective study. Ann Fam Med. 2022;20:227–36.
Liu A, Bui T, Van Nguyen H, Ong B, Shen Q, Kamalasena D. Serum C-reactive protein as a biomarker for early detection of bacterial infection in the older patient. Age Ageing. 2010;39:559–65.
Gbinigie OA, Ordóñez-Mena JM, Fanshawe TR, Plüddemann A, Heneghan C. Diagnostic value of symptoms and signs for identifying urinary tract infection in older adult outpatients: systematic review and meta-analysis. J Infect. 2018;77:379–90.
Gbinigie OA, Onakpoya IJ, Richards GC, Spencer EA, Koshiaris C, Bobrovitz N, et al. Biomarkers for diagnosing serious bacterial infections in older outpatients: a systematic review. BMC Geriatr. 2019;19:190.
Edvardsson M, Sund-Levander M, Milberg A, Ernerudh J, Grodzinsky E. Elevated levels of CRP and IL-8 are related to reduce survival time: 1-year follow-up measurements of different analytes in frail elderly nursing home residents. Scand J Clin Lab Invest. 2019;79:288–92.
Statens Serums Institut. Uge 44/45-2021: Lav influenzaaktivitet 2021. https://www.ssi.dk/aktuelt/nyhedsbreve/influenza-nyt/2021-2022/44-45-2021 . Accessed 1 Mar2023.
Lhopitallier L, Kronenberg A, Meuwly JY, Locatelli I, Mueller Y, Senn N, et al. Procalcitonin and lung ultrasonography point-of-care testing to determine antibiotic prescription in patients with lower respiratory tract infection in primary care: pragmatic cluster randomised trial. BMJ. 2021;374:n2132.
Oehme R, Sandholzer-Yilmaz AS, Heise M, Frese T, Fankhaenel T. Utilization of point-of-care tests among general practitioners, a cross-sectional study. BMC Prim Care. 2022;23:41.
Rodrigues LP, de Oliveira Rezende AT, Delpino FM, Mendonça CR, Noll M, Nunes BP, et al. Association between multimorbidity and hospitalization in older adults: systematic review and meta-analysis. Age Ageing. 2022;51(7):afac155.
Fournaise A, Andersen-Ranberg K, Lauridsen JT, Espersen K, Gudex C, Bech M. Conceptual framework for acute community health care services – illustrated by assessing the development of services in Denmark. Soc Sci Med. 2023;324:115857.
Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Article Google Scholar
Download references
Acknowledgements
We would like to acknowledge Open Patient Explorative Network (OPEN) for support on data-management. We would also like to thank the Acute Community Healthcare Service in Kolding Municipality (Acute Team Kolding) and all Acute Community Nurses for their cooperation in the study. Peter Barkholdt and Anne-Mette Rottwitt contributed with their assistance to the implementation of the study and dedicated engagement in the Advisory Board. We would also like to thank all the primary care physicians in Kolding Municipality for their collaboration. The Emergency Department and Department of Biochemistry and Immunology, Lillebaelt Hospital, Kolding, and Department of Clinical Microbiology , Lillebaelt Hospital , Vejle , supported the study with their expertise in handling and analysing POCT samples.
Open access funding provided by University of Southern Denmark. This work was supported by Odense University Hospital, Innovationspuljen [A4848], Hartmann Foundation [A36257], Grosserer L. F. Foghts Foundation, and the University of Southern Denmark [20/15107]. None of the funding bodies had any role in the conceptualization of design, data collection, analysis, interpretation, peer-review, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark
Siri Aas Smedemark & Karen Andersen-Ranberg
Department of Clinical Research, University of Southern Denmark, Kløvervænget 2D, Indgang 112, 7. Sal, Odense, 5000, Denmark
Siri Aas Smedemark, Christian B. Laursen & Karen Andersen-Ranberg
Department of Respiratory Medicine, Odense University Hospital, Odense, Denmark
Christian B. Laursen
Research Unit of General Practice, Department of Public Health, University of Southern Denmark, Odense, Denmark
Dorte Ejg Jarbøl
Department of Clinical Microbiology, Odense University Hospital, Odense, Denmark
Flemming S. Rosenvinge
Research Unit of Clinical Microbiology, University of Southern Denmark, Odense, Denmark
You can also search for this author in PubMed Google Scholar
Contributions
SAS, CBL, DEJ, FSR and KAR designed the study. SAS conducted the study, collected data, analysed data, prepared manuscript, figures, and tables. CBL, DEJ, FSR, and KAR provided constructive feedback on the draft and manuscript. SAS, CBL, FSR, DEJ, and KAR interpreted findings and read and approved the final manuscript.
Corresponding author
Correspondence to Siri Aas Smedemark .
Ethics declarations
Ethics approval and consent to participate.
The ethical principles for medical research as stated by the Declaration of Helsinki, were applied throughout the study [ 40 ]. The study is reported in line with CONSORT 2010 statements for pilot and feasibility trials [ 13 ]. The study was approved by the Regional Committees on Health Research Ethics for Southern Denmark (S-20210046). Methods have followed guidelines and regulation given by the Regional Committees on Health Research Ethics for Southern Denmark. Consent forms and process have been ethically reviewed by the Regional Committees on Health Research Ethics for Southern Denmark. All participants provided written informed consent. Written informed consent was obtained from all participants by the principal investigator.
The pilot-study was registered at the Research & Innovation Organisation (RIO), University of Southern Denmark, record of data processing activities, (Project identification number: 11.404). Data was processed and stored in accordance with EU General Data Protection Regulation (GDPR) and the Danish Data Protection Act.
Consent for publication
Not applicable.
Competing interests
SAS declare no competing interest.
CBL has in the past 36 months received speaker’s honoraria for lectures at educational events / symposia / courses organised by AstraZeneca, royalties as author of book chapters or as editor of books / web publications by Munksgaard.
DEJ declare no competing interest.
FSR declare no competing interest.
KAR declare no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Smedemark, S.A., Laursen, C.B., Jarbøl, D.E. et al. Improving diagnostics using extended point-of-care testing during in-home assessments of older adults with signs of emerging acute disease: a prospective observational non-randomised pilot and feasibility study. BMC Geriatr 24 , 373 (2024). https://doi.org/10.1186/s12877-024-04914-5
Download citation
Received : 05 September 2023
Accepted : 21 March 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12877-024-04914-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Focused lung ultrasound
- Primary care
- In-home assessments
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government.
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- American Rescue Plan
- Coronavirus Resources
- Disability Resources
- Disaster Recovery Assistance
- Equal Employment Opportunity
- Guidance Search
- Health Plans and Benefits
- Registered Apprenticeship
- International Labor Issues
- Labor Relations
- Leave Benefits
- Major Laws of DOL
- Other Benefits
- Retirement Plans, Benefits and Savings
- Spanish-Language Resources
- Termination
- Unemployment Insurance
- Veterans Employment
- Whistleblower Protection
- Workers' Compensation
- Workplace Safety and Health
- Youth & Young Worker Employment
- Breaks and Meal Periods
- Continuation of Health Coverage - COBRA
- FMLA (Family and Medical Leave)
- Full-Time Employment
- Mental Health
- Office of the Secretary (OSEC)
- Administrative Review Board (ARB)
- Benefits Review Board (BRB)
- Bureau of International Labor Affairs (ILAB)
- Bureau of Labor Statistics (BLS)
- Employee Benefits Security Administration (EBSA)
- Employees' Compensation Appeals Board (ECAB)
- Employment and Training Administration (ETA)
- Mine Safety and Health Administration (MSHA)
- Occupational Safety and Health Administration (OSHA)
- Office of Administrative Law Judges (OALJ)
- Office of Congressional & Intergovernmental Affairs (OCIA)
- Office of Disability Employment Policy (ODEP)
- Office of Federal Contract Compliance Programs (OFCCP)
- Office of Inspector General (OIG)
- Office of Labor-Management Standards (OLMS)
- Office of the Assistant Secretary for Administration and Management (OASAM)
- Office of the Assistant Secretary for Policy (OASP)
- Office of the Chief Financial Officer (OCFO)
- Office of the Solicitor (SOL)
- Office of Workers' Compensation Programs (OWCP)
- Ombudsman for the Energy Employees Occupational Illness Compensation Program (EEOMBD)
- Pension Benefit Guaranty Corporation (PBGC)
- Veterans' Employment and Training Service (VETS)
- Wage and Hour Division (WHD)
- Women's Bureau (WB)
- Agencies and Programs
- Meet the Secretary of Labor
- Leadership Team
- Budget, Performance and Planning
- Careers at DOL
- Privacy Program
- Recursos en Español
- News Releases
- Economic Data from the Department of Labor
- Email Newsletter
News Release
Department of Labor investigation into visiting nurse’s death finds home care agency failed to protect workers against workplace violence
HARTFORD, CT – A federal workplace safety investigation following the death of a licensed practical nurse during an Oct. 28, 2023, home visit in Willimantic, Connecticut, found one of the nation’s largest home-based care providers did not provide adequate safeguards to protect the nurse, Joyce Grayson, and other employees from the dangers of workplace violence .
The U.S. Department of Labor’s Occupational Safety and Health Administration determined that on or about Oct. 28, 2023, and at times prior, Elara Caring exposed home healthcare employees to workplace violence from patients who exhibited aggressive behavior and were known to pose a risk to others.
Following its investigation, OSHA cited Jordan Health Care Inc. and New England Home Care Inc., both doing business as Elara Caring, for one willful violation under the agency’s general duty clause. OSHA cited the employer for not developing and implementing adequate measures to protect employees from the ongoing serious hazard of workplace violence. The agency also cited the employer for one other-than-serious violation for not providing work-related injury and illness records to OSHA within four business hours, as required.
Elara Caring faces $163,627 in proposed penalties. View the citations .
“Elara Caring failed its legal duty to protect employees from workplace injury by not having effective measures in place to protect employees against a known hazard and it cost a worker her life,” said OSHA Area Director Charles D. McGrevy in Hartford, Connecticut. “For its employees’ well-being, Elara must develop, implement and maintain required safeguards such as a comprehensive workplace violence prevention program. Workplace safety is not a privilege; it is every worker’s right.”
To address workplace violence, employers should have in place a comprehensive workplace violence prevention program. Elements of a plan should include management commitment and employee involvement; implementation of a written program including the establishment, membership and role of a Workplace Violence Safety Committee; analysis of home environments upon new patient admission; hazard prevention and control; training and education, including resources for impacted employees; recordkeeping; and solicitation of employee feedback during the review process.
OSHA also found that Elara Caring could have reduced the hazard of workplace violence by, among other ways, performing root cause analyses on incidents of violence and near misses, providing clinicians with comprehensive background information on patients prior to home visits, providing emergency panic alert buttons to clinicians and developing procedures for the use of safety escorts for visits to patients with high-risk behaviors.
Elara Caring provides home-based care with over 200 branches in 17 states, including five branches in Connecticut. Its services include skilled home health, hospice care, personal care service, palliative care and behavioral health.
The company has 15 business days from receipt of its citations and penalties to comply, request an informal conference with OSHA’s area director, or contest the findings before the independent Occupational Safety and Health Review Commission.
The Bureau of Labor Statistics reports 849 U.S. workers died in workplace violence incidents in 2022 . Learn more about OSHA and protecting employees against workplace violence , including Guidelines for Preventing Workplace Violence for Healthcare and Social Service Workers , Workplace Violence in Healthcare: Understanding the Challenge and Preventing Workplace Violence: A Road Map for Healthcare Facilities .

IMAGES
VIDEO
COMMENTS
1. Book your appointment. Pick a time for a Getlabs specialist to come to your home or office. 2. We collect your samples. We draw your labs for Labcorp and Quest and provide them your insurance information. 3. Get your lab results. Receive your lab results from your doctor, laboratory, or via Apple Health.
While your local Labcorp locations remain open and available, Getlabs for Labcorp can now come to your home or office. Starting at $35, a trained Getlabs phlebotomist will draw your labs and deliver them directly to Labcorp. Getlabs takes care of providing your insurance information to Labcorp, and the results get delivered back to you and your ...
Quest Blood Draw and Diagnostics At-Home Services. Get a blood draw in the comfort of your own home by requesting an appointment from the National Phlebotomy Provider Network. We will draw your blood at home and deliver it to Quest Diagnostics. Note: Quest does not offer its own home blood draw services. We are a 3rd party company that helps ...
Some common at-home blood tests include: Cholesterol and lipid panel: Measures total cholesterol, LDL, HDL and triglyceride levels. Hemoglobin A1c: Measures average blood sugar levels over the ...
Look out for your health. A UnitedHealthcare® HouseCalls visit is a no-cost, yearly health check-in that can make a big difference. Call 1-866-799-5895, TTY 711, to schedule your visit.
needs before starting the visit. This data informs the APC of the patient's medical history, previous and current medications, and previous tests or screenings. HouseCalls visit. HouseCalls. Frequently asked questions. PCA-1-24-0019-Clinical-A03072024.
How it works? If time or mobility is a problem we can organise for a nurse to visit you at your home or office to take your blood sample. Simply choose Nurse Visit as your collection method when making your purchase, and we'll arrange for a nurse to call you and make a convenient appointment. A nurse visit will cost an additional £45.
With the service, individuals can now schedule a home blood draw or specimen collection when it's convenient for them. Appointments are available through Labcorp.com.Getlabs provides at-home lab appointments performed by its full-time phlebotomists and charges a convenience fee starting at $25.Getlabs for Labcorp is available in 50 U.S. markets reaching more than 50% of the U.S. population ...
Also, the majority of activities underlying the home visits could, to some degree, be linked to long‐term illnesses: medication (57%), blood samples (23%), wound care (17%) or measurement of blood pressure (14%). Only a few observations of acute care activities were seen (acute bleeding, rash; congested urinary or pleura drainage).
HouseCalls is included at no extra cost in most Medicare and Medicaid members as part of your health plan. 1 Schedule at a convenient time and we'll come to you. Call to request a visit 1-866-799-5895, TTY 711, Monday - Friday 8 a.m. - 8:30 p.m. ET. For medical emergencies, call 911.
Final Verdict. While each visiting nurse service on this list has its strengths, AccentCare is our top pick due to its wide variety of specialized programs and high quality rating. The caretakers at AccentCare are skilled and experienced. Plus, home care visits are supplemented with an advanced tele-monitoring system.
To get you preventive care in home, we work with the experienced team at Signify Health®. They'll answer all your health questions. And share a visit summary with your doctor to keep them in the loop. Hear from one member, Nancy*, about how a Healthy Home Visit found a blood flow issue — and alerted her doctor to get her the care she needed.
Lab-in-a-Box allows home health care providers to draw blood using plasma tubes and send it directly to the lab without centrifuging (spinning). How do clients use Lab-in-a-Box? After completing the custom Lab-in-a-Box test request form, clients collect specimens using the tubes inside the Lab-in-a-Box kit and then package the kit for drop-off.
Healthcare providers sometimes ask you to make an appointment to get the results of routine medical tests, especially when you're waiting for a new diagnosis or you're monitoring a chronic illness. Other times, you may be given the results by a phone call, telehealth, or online patient portal. This article will look at how long it takes to get ...
Using CPT code 99211 can boost your practice's revenue and improve documentation. The requirements for most evaluation and management (E/M) codes have gotten more precise over the years. However ...
The cost of a home or work visit is based on distance from certain Biron service centers and starts at $40. The cost of laboratory tests depends on the medical prescription. A routine blood test costs between $150 and $200 and may be fully or partially covered by your private insurance.
Pre-Departure testing now available from the comfort of your home with MyVisit (Currently Greater Toronto Area only) Order your FlyClear test and receive your FlyClear test requisition.; Book your Home Visit appointment with the MyVisit portal or, if your flight is within the next five days, contact a MyVisit coordinator 1-416-993-9579 (Monday - Friday, 9am-5pm EST)
Annual Wellness Visit (AWV) Visit to develop or update a personalized prevention plan and perform a health risk assessment. Covered once every 12 months. Patients pay nothing (if provider accepts assignment) Routine Physical Exam. Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
Nurse Home Visit. Arrange to have your blood test taken from your veins by a nurse, in the comfort of your own home or office. Venous tests have a higher success rate than finger prick blood tests and we have nurses across the UK who can help you have your blood tested. £ 70.00. Buy.
Blood test. Change of NGT tube. Change of urine catheter. Immunization. Nasogastric tube insertion. Others. Removal of stitches. Sleep disorder. Snoring. Wound dressing. ... Our home nurse visit service starts from $91.56 and $130.80 (inclusive of GST) for visits between 08:00 to 19:59 and 20:00 to 07:59 respectively. This includes a 30-minute ...
Nurse home visit service. Our nurses can visit you at your home or place of work to take your blood quickly, conveniently and professionally. All nurses are registered with the NMC and are a minimum Band 5 - simply choose the tests that you need, and select a nurse home visit at checkout. We charge a nominal fee of £55 for this extra service ...
I understand a fee will be charged once the booking is confirmed. All fees are discussed before appointments are completed. If you are a human seeing this field, please leave it empty. Phlebotomy Home Visit for Patients Do you or someone you know need a blood sample taker (known as a phlebotomist) to perform a blood test at home, or.
Step 2: Pass the National Council Licensure Examination (NCLEX)® to Become a Registered Nurse. After completing their nursing program, graduates can sit for the NCLEX, an adaptive test that ...
Delayed recognition of acute disease among older adults hinders timely management and increases the risk of hospital admission. Point-of-Care testing, including Focused Lung Ultrasound (FLUS) and in-home analysis of biological material, may support clinical decision-making in suspected acute respiratory disease. The aim of this study was to pilot test the study design for a planned randomised ...
HARTFORD, CT - A federal workplace safety investigation following the death of a licensed practical nurse during an Oct. 28, 2023, home visit in Willimantic, Connecticut, found one of the nation's largest home-based care providers did not provide adequate safeguards to protect the nurse, Joyce Grayson, and other employees from the dangers of workplace violence.