

Ob/Gyn Coding Guidelines 2023
Obstetrics and Gynaecology / Maternity care services; 1. Antepartum care 2. Delivery services 3. Postpartum care The two types of OB coding & billing guidelines are given below, 1. Global OB Care 2. Non-global OB care or partial services
Global OB Care
The total obstetric care package includes antepartum care, delivery services, and postpartum care. When the same group physician and/or other health care professional provides all components of the OB package, report the Global OB package code.
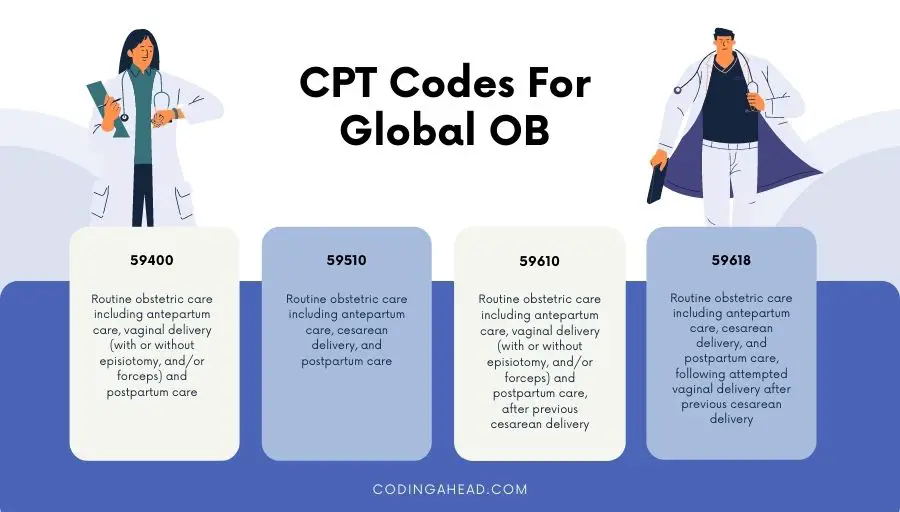
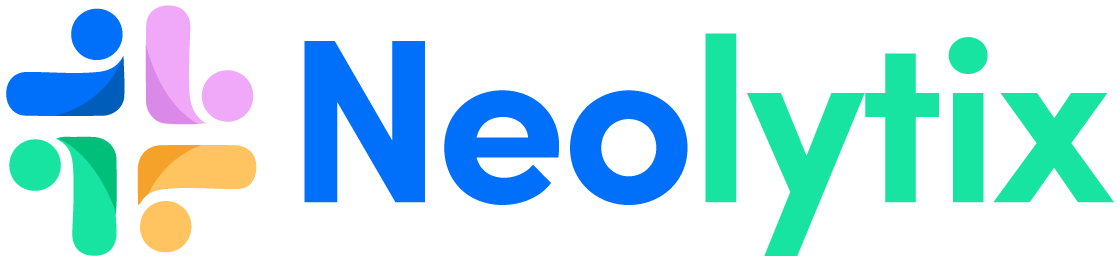
CPT Codes For Global OB
CPT code 59400 – Routine obstetric care, including antepartum care, vaginal delivery (with or without episiotomy, and/or forceps) and postpartum care.
CPT code 59510 – Routine obstetric care, including antepartum care, cesarean delivery , and postpartum care. CPT code 59610 – Routine obstetric care, including antepartum care, vaginal delivery (with or without episiotomy and forceps), and postpartum care after previous cesarean delivery. CPT code 59618 – Routine obstetric care, including antepartum care, cesarean delivery, and postpartum care, following attempted vaginal delivery after previous cesarean delivery.
OB Global Billing Guidelines
The global maternity allowance is a complete, one-time billing that includes all professional services for routine antepartum care, delivery services, and postpartum care. The fee is reimbursed to one provider for all of the member’s obstetric care. If the member is seen four or more times before delivery for prenatal care and the provider performs the delivery and postpartum care, the provider must bill the Global OB code. Global maternity billing ends with the release of care within 42 days after delivery. Global OB care should be billed after the delivery date/on delivery date.
Services Included In Global Obstetrical Package
- Routine prenatal visits until delivery, after the first three antepartum visits.
- Recording of weight, blood pressure, and fetal heart tones.
- Admission to the hospital, including history and physical.
- Inpatient Evaluation and Management (E/M) service is provided within 24 hours of delivery.
- Management of uncomplicated labor.
- Vaginal or cesarean section delivery.
- Delivery of placenta ( CPT code 59414 ).
- Administration/induction of intravenous oxytocin (CPT code 96365-96367).
- Insertion of a cervical dilator on the same date as delivery ( CPT code 59200 ).
- Repair of first or second-degree lacerations.
- A simple removal of cerclage (not under anesthesia).
- Uncomplicated inpatient visits following delivery
- Routine outpatient E/M services are provided within 42 days following delivery.
- Postpartum care after vaginal or cesarean section delivery ( CPT code 59430 ).
The above services are not reimbursed when reported separately from the global OB code. As per ACOG (American College of Obstetricians and Gynecologists) coding guidelines, reporting of third and fourth-degree lacerations should be identified by appending modifier 22 to the global OB code (CPT codes 59400 and 59610) or delivery only code (CPT codes 59409 , 59410 , 59612 and 59614 ).
Claims submitted with modifier 22 must include medical record documentation supporting the modifier’s use.
Services Excluded From The Global Obstetrical Package
The following services are excluded from the global OB package (CPT codes 59400, 59510, 59610, 59618) and may be reported separately.
- First three antepartum E&M visits
- Laboratory tests
- Maternal or fetal echography procedures (CPT codes 76801 , 76802 , 76805 , 76810 , 76811 , 76812 , 76813 , 76814 , 76815 , 76816 , 76817 , 76820 , 76821 , 76825 , 76826 , 76827 and 76828 )
- Amniocentesis, any method (CPT codes 59000 or 59001 )
- Amniofusion ( CPT code 59070 )
- Chorionic villus sampling ( CPT code 59015 )
- Fetal contraction stress test ( CPT code 59020 )
- Fetal non-stress test ( CPT code 59025 )
- External cephalic version ( CPT code 59412 )
- Insertion of cervical dilator (CPT code 59200) more than 24 hours before delivery
- E&M services unrelated to the pregnancy (e.g., UTI , Asthma) during antepartum or postpartum care.
- Additional E/M visits for complications or high-risk monitoring resulted in greater than 13 antepartum visits. However, these E/M services should not be reported until the patient delivers. Append modifier 25 to identify these visits separately from routine antepartum visits.
- Inpatient E/M services are provided more than 24 hours before delivery
- Management of surgical problems arising during pregnancy (e.g., Cholecystectomy , appendicitis, ruptured uterus)
Non-global OB Care, Or Partial Services
Non-global OB care, or partial services, refers to maternity care not managed by a single provider or group practice.
Billing for non-global OB or Partial care may occur if,
- A patient transfers into or out of a physician or group practice
- A patient is referred to another physician during her pregnancy
- A patient has the delivery performed by another physician or other health care professional not associated with her physician or group practice
- A patient terminates or miscarries her pregnancy
- A patient changes insurers during her pregnancy
The physician provides only partial services instead of global OB care To bill for that portion of maternity care only. Use the codes below for billing antepartum-only, postpartum-only, delivery-only, or delivery and postpartum-only services. Only one of the following options should be used, not a combination.
A. Antepartum Care Only
For 1 to 3 visits: Use E/M office visit codes.
For 4 to 6 visits: Use CPT 59425 ; this code must not be billed by the same provider in conjunction with one to three office visits or in conjunction with code 59426.
For seven or more visits: Use CPT 59426 – Complete antepartum care is limited to one beneficiary pregnancy per provider.
Billing Guidelines Of Antepartum Care Only
Suppose the patient is treated for antepartum services only. In that case, the physician should use CPT code 59426 if seven or more visits are provided, CPT code 59427 if 4-6 visits are provided, or each E/M visit if only providing 1-3 visits. As per ACOG and AMA guidelines, The antepartum care only codes 59425 or 59426 should be reported as described below,
A single claim submission of CPT code 59425 or 59426 for the antepartum care only, excluding the confirmatory visit that may be reported and separately reimbursed when the antepartum record has not been initiated.
The units reported should be one.
The dates reported should be the range of time covered,
E.g., If the patient had a total of 4-6 antepartum visits,, the physician should report CPT code 59425 with the from and to dates for which the services occurred.
CPT 59425 and 59426 – These codes must not be billed together by the same provider for the same beneficiary during the same pregnancy.
Pregnancy-related E/M office visits must not be billed with code 59425 or 59426 by the same provider for the same beneficiary during the same pregnancy.
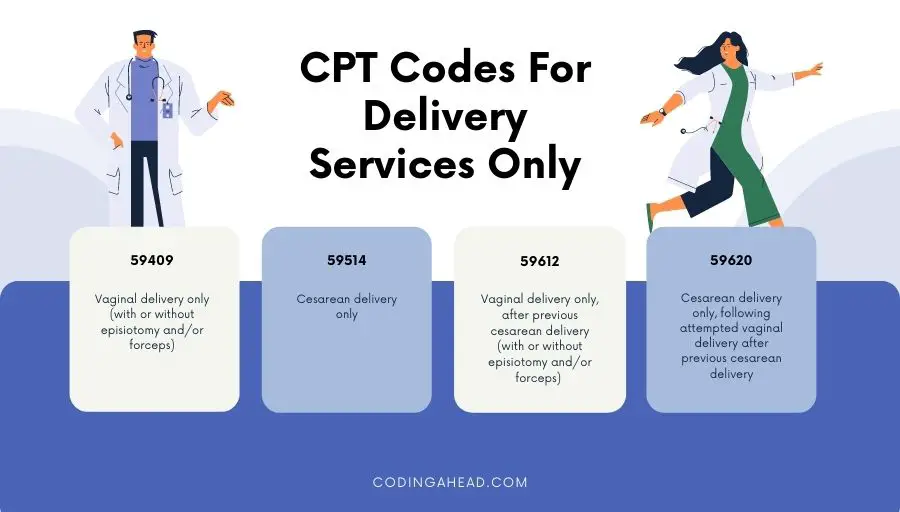
B. Delivery Services Only
The following are the CPT codes for delivery services only: CPT code 59409 – Vaginal delivery only (with or without episiotomy and/or forceps) CPT code 59514 – Cesarean delivery only CPT code 59612 – Vaginal delivery only, after previous cesarean delivery (with or without episiotomy and/or forceps) CPT code 59620 – Cesarean delivery only, following attempted vaginal delivery after previous cesarean delivery The delivery-only codes should be reported by the same group physician for a single gestation when,
The same physician or group practice does not provide the total OB package to the patient.
Only the delivery component of the maternity care is provided, and another physician or group of physicians performs the postpartum care.
Services Included In The Delivery Services
As CPT and ACOG guidelines, the following services are included in the delivery services codes and shouldn’t be reported separately.
- Admission to the hospital,
- The admission history and physical examination,
- Management of uncomplicated labor, vaginal delivery (with or without episiotomy, with or without forceps), or cesarean delivery, external and internal fetal monitoring provided by the attending physician
- Intravenous induction of labor via oxytocin (CPT code 96365-96367)
- Delivery of the placenta, any method
- Repair of first or second-degree lacerations
- Insertion of cervical dilator ( CPT 59200 ) to be included if performed on the same delivery date.
Billing Guidelines Of Delivery Services Only
Reporting of third and fourth-degree lacerations should be identified by appending modifier 22 to the global OB code (CPT codes 59400 and 59610) or delivery-only code (CPT codes 59409, 59410, 59612, and 59614) Claims submitted with modifier 22 must include medical record documentation supporting the modifier’s use.
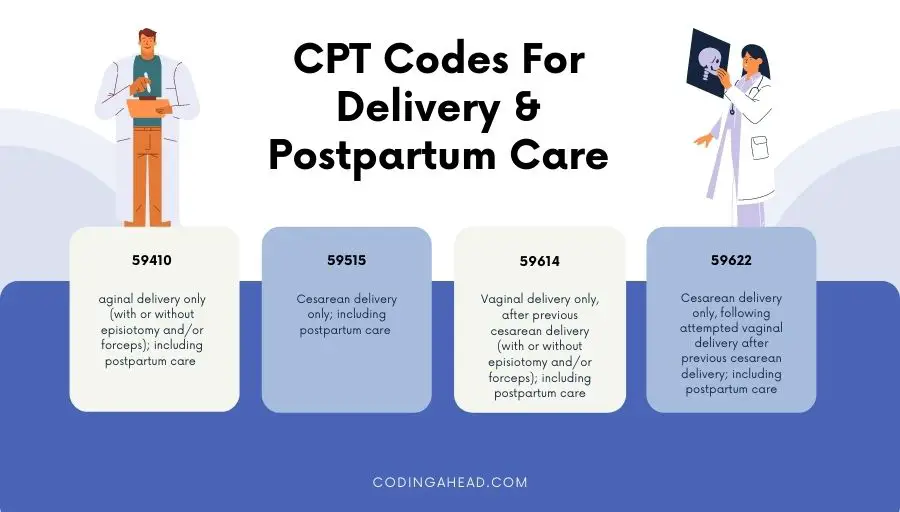
C. Delivery Only, Including Postpartum Care
Suppose the same individual or same group physician provided the delivery care and postpartum care; in these instances, few CPT codes encompass both of these services. In that case, The following are CPT-defined delivery and postpartum care. CPT code 59410 – Vaginal delivery only (with or without episiotomy and/or forceps), including postpartum care CPT code 59515 – Cesarean delivery only; including postpartum care CPT code 59614 – Vaginal delivery only, after previous cesarean delivery (with or without episiotomy and/or forceps); including postpartum care CPT code 59622 – Cesarean delivery only, following attempted vaginal delivery after previous cesarean delivery; including postpartum care
Services Included In The Delivery Only Including Postpartum Care Services
- Hospital visits related to the delivery during the delivery confinement
- Uncomplicated outpatient visits related to the pregnancy
- Discussion of contraception
D. Postpartum Care Only
The following is the CPT-defined postpartum care only, CPT 59430 – Postpartum care only (separate procedure)
Services Included In The Postpartum Care
- Uncomplicated outpatient visits related to the pregnancy
Services Excluded In The Postpartum Care
- E/M of problems or complications related to the pregnancy
Billing Guidelines For Postpartum Care Only
Postpartum care should only be reported by the same group physician who provides the patient with services of postpartum care only. Suppose a physician provides any component of antepartum along with postpartum care but does not perform the delivery. In that case, the services should be itemized using the appropriate counterpart and postpartum care codes.
Similar Posts
Primary Care Incentive Payment Program (PCIP)
According to Section 5501(a) of the Affordable Care Act the Primary Care Physicians (PCP) and NPPs who furnish specified primary care services will receive 10 percent of incentive payment for the services rendered on or after January 1, 2011 and continuing through December 31, 2015 Eligibility of New Providers for Payment under PCIP For primary…

Billing Guidelines for Vaccines (2021)
1. Effective with date of service July 1, 2011, the ONLY immunization administration codes covered for Medicaid recipients in the Health Check age range, 0 through 20 years of age, are CPT 90471 through CPT 90474. 2. Claims billed with CPT immunization administration codes CPT 90460 and CPT 90461 (effective for dates of service on and after…

Modifier for Vascular Access on Hemodialysis Claims
Modifier V5 must be entered if a vascular catheter is present even if it is not being used for the delivery of the hemodialysis. In this instance 2 modifiers should be entered, V5 (Any Vascular Catheter (alone or with any other vascular access)) for the vascular catheter and either V6 (Arteriovenous Graft (or other Vascular…

Medicare Uncompensated Care Payments (2021)
CMS distributes a prospectively determined amount of uncompensated care payments to “Medicare disproportionate share hospitals” based on their relative share of uncompensated care nationally. As required under law, this amount is equal to an estimate of 75 percent of what otherwise would have been paid as Medicare disproportionate share hospital payments, adjusted for the change…

Is their any modifier for repeated tests in laboratories?
Yes, Modifier 91 that denotes “Repeat Clinical Diagnostic Laboratory Test” should be appended to laboratory procedure(s) or service(s) to indicate a repeat test or procedure performed on the same day. This modifier indicates to the carriers or fiscal intermediaries that the physician had to perform a repeat clinical diagnostic laboratory test that was distinct or…

Centers for Medicare and Medicaid Services – Useful links
The below links gives you a quick reference on the CMS implementation / changes / revisions posted through Medicare Learning Network (MLN) and CMS Transmittals effective for the year 2010. Medicare contractors https://www.cms.gov/MedicareProviderSupEnroll/downloads/contact_list.pdf Emergency Update to the 2010 MPFSDB http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM6796.pdf New Place of Service (POS) Code for Walk-in Retail Health Clinic http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM6752.pdf 2010 Consultation services…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Sales: +1 224 529 4400
Maternity Obstetrical Care Medical Billing & Coding Guide for 2024
Coding and billing for maternity obstetrical care is quite a bit different from other sections of the American Medical Association Current Procedural Terminology (CPT).
Maternity care services typically include antepartum care, delivery services, as well as postpartum care. Depending on the patient’s circumstances and insurance carrier, the provider can either:
- Submit all rendered services for the entire nine months of services on one CMS-1500 claim form for full term deliveries for most private payers including Medicare.
- Submit claims based on an itemization of maternity care services. (e.g., most state Medicaid payers require claim submission per visit.)
Let us discuss what you need to know about maternity obstetrical care medical billing.

Maternity Obstetrical Care Medical Billing & Coding Guide for 2024
This article explores the key aspects of maternity obstetrical care medical billing and breaks down the vital information your OB/GYN practice needs to know. We will go over:
- Different types of services rendered
- The global maternity care package: what services are included and excluded?
- The split OB packages
- Complications of pregnancy
- High-risk patients
- CPT definitions
- And much more
Finally, always be aware that individual insurance carriers provide additional information such as modifier use.
We hope that this guide will assist you in maternity obstetrical care medical billing and coding for your practice. For more details on specific services and codes, see below.
Table of Contents

The Global Obstetrical Package
When discussing maternity obstetrical care medical billing, it is crucial to understand the Global Obstetrical Package .
Most insurance carriers like Blue Cross Blue Shield, United Healthcare, and Aetna reimburses providers based on the global maternity codes for services provided during the maternity period for uncomplicated pregnancies.
Currently, global obstetrical care is defined by the AMA CPT as “uncomplicated maternity cases which include antepartum, delivery, and postpartum care.” (Source: AMA CPT codebook 2024, page 450.)
If the services rendered do not meet the requirements for a total obstetric package, the coder is instructed to use appropriate stand-alone codes. These might include individual evaluation and management codes, antepartum care only, delivery only, postpartum care only, delivery and postpartum care, etc.
When billing for the global obstetrical package code, all services must be provided by one obstetrician, one midwife, or the same physician group practice provides all the patient’s routine obstetric care, which includes the antepartum care, delivery, and postpartum care.
Here a “physician group practice” is defined as a clinic or obstetric clinic that is under the same tax ID number . It uses either an electronic health record (EHR) or one hard-copy patient record. Each physician, nurse practitioner, or nurse midwife seeing that patient has access to the same patient record and makes entries into the record as services occur.
Individual Evaluation and Management (E&M) codes should not be billed to report maternity visits unless the patient presents for issues outside the global package for commercial payers.
All prenatal care is considered part of the global reimbursement and is not reimbursed separately. The provider will receive one payment for the entire care based on the CPT code billed
Services Bundled with the Global Obstetrical Package
A key part of maternity obstetrical care medical billing is understanding what is and is not included in the Global Package.
Services provided to patients as part of the Global Package fall in one of three categories. They are:
- Antepartum care: Care given from conception, up to (not including) the delivery of the fetus.
- Intrapartum care: Inpatient care of the passage of the fetus and placenta from the womb.
- Postpartum care: Care of the mother after delivery of the fetus.
Let us look at each category of care in detail.
Antepartum Care
Antepartum care comprises the initial prenatal history and examination, as well as subsequent prenatal history and physical examination. This includes:
- Monthly visits up to 28 weeks of gestation
- Biweekly visits up to 36 weeks of gestation
- Weekly visits from 36 weeks until delivery
- Recording of weight, blood pressures and fetal heart tones
- Routine chemical urinalysis (CPT codes 81000 and 81002)
- Education on breast feeding, lactation and pregnancy (Medicaid patients)
- Exercise consultation or nutrition counseling during pregnancy
IMPORTANT: Any other unrelated visits or services within this time period should be coded separately. Example: patient comes in with the flu for this visit a E/M visit should be used.
Intrapartum Care AKA Labor & Delivery
- Admission to the hospital including history and physical.
- Inpatient evaluation and management (E/M) services provided within 24 hours of delivery.
- Management and fetal monitoring of uncomplicated labor
- Administration/induction of intravenous oxytocin (performed by provider not anesthesiologist)
- Insertion of cervical dilator on same date as delivery, placement catheterization or catheter insertion, artificial rupture of membranes
- Removal of cerclage (if removed under anesthesia other than “local” it is a billable procedure)
- Vaginal, cesarean section delivery, delivery of placenta only (the operative report)
Postpartum Care
- Uncomplicated inpatient visits following delivery.
- Repair of first- or second-degree lacerations (for lacerations of the third or fourth degree, see “Services Bundled into Global Obstetrical Package”)
- Simple removal of cerclage (not under anesthesia)
- Routine outpatient E/M services that are provided within 6 weeks of delivery (check insurance guidelines for exact postpartum period)
- Discussion of contraception prior to discharge
- Outpatient postpartum care – Comprehensive office visit
- Educational services, such as breastfeeding, lactation, and basic newborn care
- Uncomplicated treatments and care of nipple problems and/or infection

Services Excluded from the Global Obstetrical Package
Certain maternity obstetrical care procedures are either overly complex and/or not required by every patient. As such, including these procedures in the Global Package would not be appropriate for most patients and providers. The American College of Obstetricians and Gynecologists (ACOG) has developed a list of procedures that are excluded from the global package. If the provider performs any of the following procedures during the pregnancy, separate billing should be done as these procedures are not included in the Global Package.
- This confirmatory visit (amenorrhea) would be supported in conjunction with the use of ICD-10-CM diagnosis code Z32.01.
- This is usually done during the first 12 weeks before the ACOG antepartum note is started. Use CPT Category II code 0500F.
- Examples include CBC, liver functions, HIV testing, Blood glucose testing, sexually transmitted disease screening, and antibody screening for Rubella or Hepatitis, etc.
- Maternal or fetal echography procedures
- Depending on the insurance carrier, all subsequent ultrasounds after the first three are considered bundled
- Cerclage, or the insertion of a cervical dilator more than 24 hours from admission.
- External cephalic version (turning of the baby due to malposition)
- Amniocentesis (any method)
- Amnioinfusion
- Chorionic villus sampling (CVS)
- Fetal contraction stress test
- Examples include cardiac problems, neurological problems, diabetes, hypertension, hyperemesis, preterm labor, bronchitis, asthma, and urinary tract infection
- NOTE: These encounters could be office visits, clinic visits, emergency room, or inpatient admission/observation.
- Inpatient E/M services provided more than 24 hours before delivery
- Examples include urinary system, nervous system, cardiovascular, etc.
- Per ACOG coding guidelines, this should be reported using modifier 22 of the CPT code used to bill.
- Contraceptive management services (insertions)
List of CPT Codes
The AMA categorizes Maternity care and delivery CPT codes. The following is a comprehensive list of all CPT codes for full term pregnant women.
IMPORTANT: Complications of pregnancy such as abortion (missed/incomplete) and termination of pregnancy are not included in this list.
The following codes can also be found in the 2024 CPT codebook.
Description
Routine obstetric care including antepartum care, vaginal delivery (with or without episiotomy, and/or forceps) and postpartum care, after previous cesarean delivery
Global Package Code Vaginal Delivery
Vaginal delivery only (with or without episiotomy and/or forceps);
Itemization Code
Vaginal delivery only (with or without episiotomy and/or forceps); including postpartum care
Antepartum care only; 1-3 visits
Antepartum care only; 4-6 visits
Antepartum care only; 7 or more visits
Postpartum care only (separate procedure)
Routine obstetric care including antepartum care, cesarean delivery, and postpartum care
Global Package Code C-Section Delivery
Cesarean delivery only;
Cesarean delivery only; including postpartum care
Global Package Code VBAC Delivery
Vaginal delivery only, after previous cesarean delivery (with or without episiotomy and/or forceps);
Vaginal delivery only, after previous cesarean delivery (with or without episiotomy and/or forceps); including postpartum care
Routine obstetric care including antepartum care, cesarean delivery, and postpartum care, following attempted vaginal delivery after previous cesarean delivery
Cesarean delivery only, following attempted vaginal delivery after previous cesarean delivery;
Cesarean delivery only, following attempted vaginal delivery after previous cesarean delivery; including postpartum care

Maternity Obstetrical Care Medical Billing for Twin Delivery/Multiple Gestation
Some pregnant patients who come to your practice may be carrying more than one fetus. In such cases, certain additional CPT codes must be used.
ACOG has provided the following coding guidelines for vaginal, cesarean section, or a combination of vaginal and cesarean section deliveries.
To ensure accurate maternity obstetrical care medical billing and timely reimbursements for work performed, make sure your practice reports the proper CPT codes.
Type of Service/Procedure
Type of twin, cpt codes reported.
Vaginal Delivery of Twins
C-Section Delivery of Twins
Twin A & Twin B
Repeat Cesarean Delivery
Delivery of Twins
VBAC Delivery of Twins
Vaginal & C-Section Delivery of Twins
VBAC + repeat Cesarean Delivery of Twins
If both twins are delivered via cesarean delivery, report code 59510 (routine obstetric care including antepartum care, cesarean delivery, and postpartum care). This is because only one cesarean delivery is performed in this case.
However, if the cesarean delivery is significantly more difficult, append modifier 22 to code 59510. When reporting modifier 22 with 59510, a copy of the operative report should be submitted to the insurance carrier with the claim.
Split Care Performed/Itemization Billing
Some patients may come to your practice late in their pregnancy. Others may elope from your practice before receiving the full maternal care package. In such cases, your practice will have to split the services that were performed and bill them out as is. Examples of situations include:
- The patient has received part of her antenatal care somewhere else (e.g. from another group practice).
- The patient leaves her care with your group practice before the global OB care is complete.
- Patient receives care from a midwife but later requires MD-level care.
- The patient has a change of insurer during her pregnancy.
In these situations, your practice should contact the insurance carrier and notify them of these changes. This will allow reimbursement for services rendered . If the patient has fewer than 13 encounters with the provider, your practice should contact the insurer to find out whether the insurer will honor the global package CPT code. Billings include:
- 59425: Antepartum care only, 4-6 visits
- 59426: Antepartum care only, 7 or more visits; E/M visit if only providing 1-3 visits
- Delivery only: CPT codes 59409, 59514, 59612, and 59620
- Postpartum care only: CPT code 59430


Maternity Obstetrical Care Medical Billing for High-Risk Pregnancies
In the case of a high-risk pregnancy, the mother and/or baby may be at increased risk of health problems before, during, or after delivery. In this case, special monitoring or care throughout pregnancy is needed, which may require more than 13 prenatal visits.
Examples of high-risk pregnancy may include:
- Advanced maternal age: pregnancy risks rise for mothers past the age of 35.
- Maternal health problems: pre-gestation medical complication such as hypertension, diabetes, epilepsy, thyroid disease, heart or blood disorders, poorly controlled asthma, and infections can increase pregnancy risk.
- Pregnancy-Related Complications: examples include gestation, diabetes and/or hypertension, poor fetal growth, premature rupture of membrane, abnormal placenta position, etc.
All these conditions require a higher and closer degree of patient care than a patient with an uncomplicated pregnancy.
As such, visits for a high-risk pregnancy are not considered routine. They should be reported in addition to the global OB CPT codes of 59400, 59510, 59610 or 59618.
If medical necessity is met, the provider may report additional E/M codes, along with modifier 25, to indicate that care provided is significant and separate from routine antepartum care. The claim should be submitted with an appropriate high-risk or complicated diagnosis code.
Examples of applicable ICD-10-CM codes:
Supervision of other high-risk pregnancies
Pre-existing hypertensive heart disease complicating pregnancy
Pre-existing hypertension with pre-eclampsia
Gestational [pregnancy-induced] edema and proteinuria without hypertension
Pre-eclampsia
Pre-existing type-1 diabetes mellitus, in pregnancy, childbirth, and the puerperium
Liver and biliary tract disorders in pregnancy, childbirth, and the puerperium
Anemia complicating pregnancy, childbirth, and the puerperium
NOTE: When a patient who is considered high risk during her pregnancy has an uncomplicated delivery with no special monitoring or other activities, it should be coded as a normal delivery according to ICD-10-CM guidelines.

Maternal-Fetal Medicine (MFM) Care
Maternal-fetal medicine specialists, also known as perinatologists , are physicians who subspecialize within the field of obstetrics. They focus on managing the health concerns of the mother and fetus prior to, during, and shortly after pregnancy.
Per ACOG, all services rendered by MFM are outside the global package. Unless the patient sees the provider during their entire pregnancy then a global package is appropriate . An MFM is allowed to bill for E/M services along with any procedures performed (such as ultrasounds, fetal doppler, etc.) with a modifier 25.
Make sure you double check all insurance guidelines to see how MFM services should be reported if the provider and MFM are within the same group practice.
Ultrasound Billing
When reporting ultrasound procedures, it is crucial to adhere closely to maternity obstetrical care medical billing and coding guidelines.
It is necessary to keep a written report from the provider and have images stored on file . As per AMA CPT and ultrasound documentation requirements, image retention is mandatory for all diagnostic and procedure guidance ultrasounds.
Appropriate image(s) and reports demonstrating relevant anatomy/pathology for each procedure coded should be retained and available for review. CPT does not specify how the images should be stored or how many images are required . However, in your documentation the provider should document where to find the images and report.
Modifiers may be applicable if there is more than one fetus and multiple distinct procedures performed at the same encounter. Incorrectly reporting the modifier will cause the claim line to be denied.
The following CPT codes cover ranges of several types of ultrasound recordings that might be performed. Make sure your practice follows correct guidelines for reporting each CPT code.
- 76801–76810: maternal and fetal evaluation (transabdominal approach, by trimester)
- 76811–76812: above and detailed fetal anatomical evaluation
- 76813–76814: fetal nuchal translucency measurement
- 76815: limited trans-abdominal ultrasound study
- 76816: follow-up trans-abdominal ultrasound study
- 76817: trans-vaginal ultrasound study
- 76818–76819: fetal biophysical profile
- 59025: fetal non-stress test
It is essential to read all the parenthetical guidelines that instruct the coder on how to properly bill the service for multiple gestations and more than one type of ultrasound.
Trimesters of Pregnancy
- 1 st trimester: less than 14 weeks 0 days
- 2 nd trimester: 14 weeks 0 days, to less than 28 weeks 0 days
- 3 rd trimester: 28 weeks 0 days, to delivery
NOTE: For ICD-10-CM reporting purposes, an additional code from category Z3A.- (weeks of gestation) should ALWAYS be reported to identify the specific week of pregnancy. (e.g., 15-week gestation is reported by Z3A.15).

Diagnosis Codes for Deliveries and Related Services
- Reporting Routine Prenatal Visits: routine prenatal visits are reported with a code from category Z34.- It should always be the first-listed diagnosis code unless the patient has other medical conditions affecting the pregnancy. Note that Z34.- codes should never be reported with an O code.
- Outcome of Delivery: should be included when a delivery has occurred (ICD-10-CM Z37.-).
- If O80 is not appropriate, the primary diagnosis should reflect the main circumstances or complications of the delivery.
- If the patient is admitted with condition resulting in cesarean, then that is the primary diagnosis.
- If admitted for other reason, the admitting diagnosis is primary for admission and reason for cesarean linked to delivery.
- If multiple conditions prompted the admission, sequence the one most related to the delivery as the principal diagnosis.
- O Codes: An O code from ICD-10-CM Chapter 15 – “Pregnancy, Childbirth & the Puerperium” should always be reported for the delivery when the patient has experienced any current complication in the antepartum period, during the delivery, or in the postpartum period.
- All conditions treated or monitored can be reported (e.g., gestation diabetes, pre-eclampsia, prior C-section, anemia, GBS, etc.)
Who Is Eligible to Provide Patient Care?
The following is a comprehensive list of eligible providers of patient care (with the exception of residents, who are not billable providers):
- Obstetrician, Maternal Fetal Specialist, Fellow
- Certified Nurse Midwife (CNM)
- Nurse Practitioner Midwife (NPM)
- Certified Professional Midwife (CPM)
Depending on your state and insurance carrier (Medicaid), there may be additional modifiers necessary to report depending on the weeks of gestation in which patient delivered. Before completing maternity obstetrical care billing and coding, always make sure that the latest OB guidelines are retrieved from the insurance carrier to avoid denials or short pay.
To ensure proper maternity obstetrical care medical billing, it is critical to look at the entire nine months of work performed to properly assign codes.
Pay special attention to the Global OB Package. The coder should have access to the entire medical record (initial visit, antepartum progress notes, hospital admission note, intrapartum notes, delivery report, and postpartum progress note) to review what should be coded outside the global package and what can be bundled in the Global Package.
The key is to remember to follow the CPT guidelines, correctly append diagnoses, and ensure physician documentation of the antepartum, delivery and postpartum care and amend modifier(s).
At Neolytix, we’re here to support your practice with medical billing services for OBGYN , coding, EMR templates, and more.
Reach out to us anytime for a free consultation by completing the form below.
American College of Obstetricians and Gynecologists
- Coding for Postpartum Services (The Fourth Trimester)
Stanford Children’s Help
- Fetal Ultrasound
- From Antepartum to Postpartum
Get Help with Billing, Credentialing, & Virtual Assistants - Work With A Team of Experts
- Your Name First Last
- Name of the Practice * Practice Name
- Text Message
- Specialty *
- EHR system being used What EHR are you using to bill claims to Insurance companies, store patient notes.
- <$50,000
- $50,000- $250,000
- $250,000-$1,000,000
- $1,000,000-$5,000,000
- >$5,000,000
- What State(s) do you operate in?
- Comments This field is for validation purposes and should be left unchanged.
Popular Posts

Proven Strategies to Improve Patient Collections

Benefits Of Remote Patient Monitoring For Healthcare Providers

Successful CAQH credentialing for healthcare providers

New Add-On CPT Code 99459 for Pelvic Exams

All You Need to Know About Outsourcing Revenue Cycle Management

2024 CMS Update: Modifiers for Rural Health Clinics & FQHCs
Posts by category.
- All Posts (134)
- Billing & Coding Guides
- Covid Impact
- Credentialing
- Freelancing
- Medical Billing
- Medical Licensing
- Medical Virtual Assistant
- Medicare Chronic Care Management
- Press Release
- Remote Patient Monitoring
- Revenue Cycle Management
- Uncategorized
Stay ahead of the curve & join our provider community to get updated on the latest industry trends.
Newsletter (active).

- Why work with us
- Job Openings
- HOSPITALS & HCO'S
- Revenue Transformation
- Value Based Care Programs
- Patient Access
- Coding Audits
- CLINICS & MULTI PROVIDER GROUPS
- Virtual Assistant Services
- Payor Contract Negotiation
- Credentialing & Maintenance
- Website & Marketing
- F&A Services
- Recruitment Outsourcing
- NEWS & RESOURCES
- Neo News Hub

Request A Quote
Get your free intuitive, fast facts for maternity obstetrical care coding flash guide now.
An OB/GYN Coding Cheat Sheet to Make Your Billing Process Easier
Melanie Graham
It seems the world of medical billing gets more complicated every year, doesn’t it? The intricacies of coding can be particularly complex — especially in the obstetrics and gynecology field.
While OB/GYN medical billing may be a lot to manage, having a solid understanding of Current Procedural Terminology (CPT) codes influences one critical piece of your practice: getting paid.
Unfortunately, changes to these codes and their interpretation can be challenging to track. Having an OB/GYN billing cheat sheet (like the one below) and a solid medical billing software partnership can help.
What Is a CPT Code?
A CPT code, or Current Procedural Terminology code , is a number that corresponds with a particular medical service or procedure. CPT codes are a standardized system and a way for payers and insurers to speak the same language about medical services. Providers submit claims with these CPT codes to receive payment from insurers.
In general, OB billing codes range from 56405 to 59899, but you may use other codes outside that range for routine gynecologic care and well-woman visits.
>> Claim Scrubbing: What it Is and Why It’s Important
OB/GYN Coding Cheat Sheet
Keeping track of OB/GYN CPT codes and billing best practices is far from easy. We’ve put together this cheat sheet with a few basics for OB/GYN billing. You can download the full cheat sheet with CPT codes here or check out a short preview below.

OB Billing and Coding Best Practices
OB coding can certainly cause some headaches, but remembering a few key essentials will help you with more accurate claims:
- Make sure you understand the payer’s billing guidelines for deliveries, antepartum care and global codes. Every plan is different. For example, Medicaid HMO plans require you to bill for deliveries with non-standard codes.
- Create an “OB contract” for patients to pay their portion of the delivery claim before delivery. Patients will have a lot of medical bills from the delivery experience. They’ll have a better sense of security and overall experience with price transparency, up-front estimates and the option to make payments before delivery.
- Use global codes for maternity care. Avoid billing separately for services already included in these codes.
- Don’t forget to use separate E/M codes when appropriate. You can use these codes for services that aren’t related to maternity care
Get more best practices in our full OB/GYN Coding Cheat Sheet.
Global Codes for OB/GYN Billing
You’ll notice that we’ve outlined some maternity care global codes in this OB/GYN billing cheat sheet. You can use these codes when the same physician or physician group provides all maternity services for a patient.
OB global codes include 59400, 59510, 59610 and 59618. These include all care from antepartum through delivery and postpartum care.
- 59400 – Routine obstetric care for vaginal delivery (with or without episiotomy and/or forceps), including antepartum and postpartum care.
- 59510 – Routine obstetric care for cesarean section delivery, including antepartum and postpartum care.
- 59610 – Routine obstetric care for vaginal delivery (with or without episiotomy and/or forceps) after cesarean delivery, including antepartum and postpartum care.
- 59618 – Routine obstetric care for cesarean delivery following attempted vaginal delivery after previous cesarean delivery, including antepartum and postpartum care.
It’s important to note when you use a global code, you can’t bill separate evaluation and management (E/M) codes for individual parts of maternity care. However, you can bill separately if the mother’s insurance coverage changes during the pregnancy or if another physician cares for the mother before you complete all the services in the global code.
You can also separately bill the initial visit to confirm pregnancy.
You can bill E/M codes if the mother seeks care for a problem not related to her pregnancy, such as treatment for a yeast infection or a postpartum discussion about birth control. You will also bill separate codes for most lab tests you do during the pregnancy.
Gynecology Coding Best Practices
If you’re working on the ‘GYN’ side of OB/GYN, there are other best practices you’ll need to keep in mind.
Hysterectomies
A hysterectomy is surgery to remove the uterus. Although this procedure may sound relatively straightforward, there are some unique coding and billing best practices to keep in mind:
- The approach to the surgery will determine the CPT code. There are three main approaches: abdominal, vaginal and laparoscopic.
- The weight of the uterus can also influence which CPT code you should use.
- The extent of the surgery (how much of the uterus is removed) may influence which CPT code you should use.
- Some CPT codes factor in additional services or procedures with the hysterectomy.
- Abdominal hysterectomy codes range between 58150 and 58210.
- Vaginal hysterectomy codes range between 58260 and 58291.
- Laparoscopic hysterectomy codes range between 58541 and 58573.
Well-Woman Visits
Well-woman exams are yearly check-ups women have with their OB/GYN. These appointments can include a general health screening as well as cervical cancer screening.
It’s important to remember that you’ll code well-woman exams based on two factors: the age of the patient and whether they are a new or returning patient. New patient codes range from 99385-99387 and existing patient codes range from 99395-99397.
What About Modifiers?
OB/GYN CPT codes often include modifiers on the end. Modifiers are two-digit codes that show you’ve somehow altered the service in the original five-digit CPT code. For example, if a woman delivers twins, you may use the “22” modifier to indicate additional or increased services. For a full list of common OB/GYN modifiers, download our coding cheat sheet.
Find a Partner Who Can Modernize Your OB/GYN Billing Process
Efficient and accurate coding is one piece of healthy revenue cycle management and crucial to the success of your OB/GYN practice. So, why waste resources on an outdated, clunky billing process?
With Gentem’s AI-powered revenue cycle management (RCM) platform , you can:
- Easily manage all your OB patients in one spot. This helps you track all your patients and the services you provide, so you’re not leaving money on the table.
- Catch high-deductible patients so you can optimize when to bill your claim.
- Streamline OB/GYN patient estimates, so you can increase up-front payments and improve the patient experience.
Whether you need complete RCM support or state-of-the-art software to boost your medical billing team, we have you covered. Our platform has helped OB/GYN practices achieve record collections , allowing them to expand staff and care for more patients.
Learn more about our powerful RCM and billing tools by booking a demo today .
Increase Revenue & Collection Rates
Gentem’s tech platform and team of billing experts increase practice revenue by an average of 20%.

WATCH: Revenue Cycle Tips for Staying Independent
Many physicians are leaving private practice due to rising costs, lower reimbursement rates and staffing shortages. But staying independent is possible with a healthy revenue cycle.
Learn how to run a successful private practice with tips from this 20-minute webinar session.
5 Must-Know Metrics To Build A Thriving Medical Practice
With this free guide, you’ll learn the key metrics that inform your practice’s financial performance and how best to optimize them to support practice growth.
Subscribe To Our Newsletter
Related articles.

What Is Healthcare Revenue Cycle Management (RCM)?

Revenue Cycle KPI Glossary: Definitions and Benchmarks You Should Know

7 Ways to Prevent Medicaid Claim Denials
Eliminate your medical billing headaches today..

Is it possible to make OB coding less complicated?
The sheer number of code options can be intimidating, but mastering a few concepts can alleviate some of the stress.

CPT codes discussed in this article
Just like our patients, proper coding and billing for obstetric patients can be…complicated. As a coding instructor and compliance auditor, I field a lot of questions from new students and experienced billers alike. In this article, I’ll break down a few of the most important concepts you need to understand to master obstetric coding.
The global period
Billing codes for maternity care and delivery are used to report antepartum care, vaginal or cesarean delivery, and postpartum care in uncomplicated pregnancies. Antepartum care includes the initial prenatal history and examination, subsequent prenatal history and examinations, recording of weight, blood pressures, fetal heart tones, routine chemical urinalysis, and monthly visits up to 28 weeks’ gestation; biweekly visits to 36 weeks’ gestation; and weekly visits until delivery. Delivery services include the hospital admission, management of uncomplicated labor, and cesarean or vaginal delivery (including episiotomy and repair if needed). Postpartum care includes visits in the hospital and a 6-week follow-up in the office following delivery. It may also include services related to a cesarean delivery, such as an incision check.
When billing for maternity care and delivery, codes exist to bill the global package (antepartum care, delivery, and postpartum care) or for specific components in the event you are billing for a provider who performed the antepartum care only, delivery only, or postpartum care only.
Note that pregnancy confirmation during a problem-oriented or preventive visit is not considered part of antepartum care and should be reported separately using the appropriate E/M code (for example an Outpatient Office Visit Code, 99201-99215 ). Also, remember that medical complications of pregnancy (eg, cardiac problems, neurological problems, diabetes, hypertension) and medical problems complicating labor and delivery management may require additional resources and should be billed separately – they are not included in the “global OB package.”
Delivery coding
When it comes to billing for maternity care and delivery, the number of code options can be confusing. Simply put, there are codes to report the global package, or components of it (as discussed above) depending on the method of delivery. For example, 59400 is used to report Routine OB care including antepartum care, vaginal delivery , and postpartum care. Codes immediately following 59400 report individual components of the global package. Code 59510 reports Routine OB care including antepartum care, cesarean delivery , and postpartum care.
However, there’s one more wrinkle that confuses some coders: Patients who have had a previous cesarean delivery and now present with an expectation of vaginal delivery have their own set of delivery codes, depending on the outcome. 59610 reports routine OB care including antepartum care, vaginal delivery, and postpartum care after a previous cesarean delivery. 59618 is used when the same patient with a previous cesarean attempts a vaginal delivery but delivers again via cesarean section .
ICD-10 concepts
With ICD-10 OB coding came a new set of billing guidelines that can be complicated, especially for newer coders trying to get acclimated to coding. The first important consideration when selecting a diagnosis code is to read the guidelines for each section. The ICD-10 guidelines state that codes for chapter 15 ( Complications of Pregnancy, Childbirth, and the Puerperium ) have sequencing priority over other codes from other chapters and are to be listed first unless the pregnancy is completely incidental and has nothing to do with the reason for the visit.
Another important consideration is the fact that in ICD-10, most of the diagnoses in chapter 15 include the concept of trimester. The guidelines state that not only should you select the code with the appropriate trimester for the current encounter, but a separate code (Z3A.--) should be used to report the weeks gestation for the encounter. For example, a patient in her 16 th week of pregnancy should be assigned a code from chapter 15, followed by the code Z3A.16 to indicate 16 weeks’ gestation.
Routine vs problem visits
For a routine outpatient prenatal visit when no complications are present, select a diagnosis code from range Z34, Encounter for Supervision of Normal Pregnancy, as the primary diagnosis. Remember that on average, the global OB package encompasses 13 routine visits during pregnancy, which includes routine visits in uncomplicated cases, and 6 weeks postpartum care. This may include H&Ps, routine measurements, and educational services such as breastfeeding or basic newborn care. Services that are not part of the global OB package may be billed separately, such as an initial evaluation and management service to diagnose pregnancy, amniocentesis, cephalic version, additional E&M services for unrelated reasons (e.g., asthma or urinary tract infection) or greater frequency of visits due to a high-risk pregnancy. Sometimes coders get confused and either miss out on billing a service that isn’t included in the global OB package or they mistakenly try to bill for a visit that is included in the package.
Sometimes our patients (and our coding) can be routine, but other times things can get complicated. Having a good understanding of what is included can help you be prepared so that when you encounter a situation that isn’t included, you don’t forget to bill for it. It always helps to have your ( heavily marked up and highlighted ) coding manuals and/or cheat sheets nearby, and reimbursement policies from your office’s biggest payers on your computer.
Disclosures:
The author reports no potential conflicts of interest with regard to this article.

Multitasking: Operational imperative or efficiency fallacy?
S2E2: Overcoming Racism and Unconscious Bias in OB/GYN
Senior Editor Angie DeRosa and Associate Editor Lindsey Carr sat down with Drs. Vanessa Rogers and Shawna Nesbitt to discuss racism and unconscious bias in ob/gyn practice.

How to have difficult discussions
What are the key factors of communication with a patient who is fearing symptom progression or near death?

Feedback: Valuable to give and receive
Effective leadership hinges on adeptly delivering and receiving feedback to foster engagement, enhance performance, and cultivate a thriving organizational culture.
Using artificial intelligence in your practice
AI's role in healthcare: From diagnostics to communication, and the path forward.

Payment models put the value in value-based care
In this month's Practice Matters column, James D. Keller, MD, MHSA; and Brian K. Iriye, MD, explore the world of value-based care and how it can benefit your practice.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
- Company Information
- Network Participation
- How to Join Our Networks
- Update Your Information
- Change of Ownership
- Claims and Eligibility
- BlueCard Program
- Electronic Commerce
- Eligibility and Benefits
- Prior Authorization Services For Fully Insured and ASO
- Prior Authorizations Lists for Blue Cross Medicare Advantage (PPO) and Blue Cross Medicare Advantage (HMO)
- Prior Authorizations Lists for Designated Groups
- Recommended Clinical Review Option
- Prior Authorization Exemptions (Texas House Bill 3459)
- Claims Filing Tips
- Claim Status
- Claim Review Process
- Interactive Voice Response (IVR) System
- Medicare Advantage Private Fee For Service
- Eligibility and Benefits Inquiry (HIPAA 270/271)
Education and Reference
- Education and Reference Center
- 2024 Blue Review
- Identification Cards
- 2024 News and Updates
- Provider Tools
- Provider Training
- Blue Review Archive
- Fraud and Abuse
- Clinical Resources
- Behavioral Health Care Management Program
- Clinical Practice Guidelines
- Quality Care – Partner With Your Patients
- eviCore Prior Authorization Program
- Special Beginnings - Maternity Program
- Preventive Care Guidelines/Patient Wellness Guidelines
- Quality Improvement Tip Sheet
- Telemedicine and Telehealth Services
- Health Equity and Social Determinants of Health (SDoH)
- Pharmacy Program
- Dispensing (Quantity vs. Time) Limits
- Medicare Part D Pharmacy Updates
- Prescription Drug List and Prescribing Guidelines
- Specialty Pharmacy Programs
- Prior Authorization and Step Therapy Programs
- Split Fill Program
- Standards and Requirements
- Affordable Care Act (ACA)
- Clinical Payment and Coding Policies
- Consolidated Appropriations Act and Transparency in Coverage Final Rule
- 2024 Disclosure Notices
- Federal Employee Program (FEP)
- General Reimbursement Information
- Medical Policies
- Medical Policy and Pre-certification/Pre-authorization Information for Out-of-Area Members
- Physician Efficiency, Appropriateness, & Quality (PEAQ) Program
Supporting Maternal Quality Care
Prenatal and postpartum care contributes to the long-term well-being of new mothers and their infants, according to the American College of Obstetricians and Gynecologists . We encourage you to talk with our members about the importance of attending all care visits during and after pregnancy.
We track the following Healthcare Effectiveness Data and Information Set (HEDIS ® ) measures related to our members’ maternal health:
Prenatal and Postpartum Care measures the percentage of deliveries in which members:
- Had a prenatal care visit in the first trimester, on or before the enrollment start date or within 42 days of enrollment with Blue Cross and Blue Shield of Texas.
- Had a postpartum visit on or between seven and 84 days after delivery.
Prenatal and Postpartum Depression Screening and Follow-Up measures the percentage of deliveries in which members:
- Were screened for clinical depression during pregnancy and the postpartum period using a standardized instrument, and
- Received follow-up care within 30 days if the screening was positive.
Tips to Close Gaps in Prenatal and Postpartum Care
- Check with our members to ensure that initial prenatal visits are scheduled in the first 12 weeks of pregnancy with an OB-GYN, primary care physician or other prenatal practitioner.
- A postpartum visit must take place on or between seven and 84 days after delivery. Be aware that post-operative visits within six days after discharge don’t count as a postpartum visit. Members who have cesarean sections should be reminded to schedule their postpartum care visit during the C-section post-op visit.
- Data for this measure is collected from claims and chart review for services performed by an OB-GYN, midwife, family practitioner or other PCP. Services provided during telehealth visits, e-visits and virtual check-ups are eligible for reporting to meet the measure.
Tips to Close Gaps in Prenatal and Postpartum Depression Screening and Follow-Up
- Ask members during their pregnancy and postpartum to complete an age-appropriate depression screener, such as the Patient Health Questionnaire (PHQ)-9 or -2 , or the Edinburgh Postnatal Depression Scale.
- If the depression screening is positive, follow up within 30 days with one or more of the following, as appropriate:
− Additional evaluation for depression
− Suicide risk assessment
− Referral to a practitioner qualified to diagnose and treat depression
− Pharmacological interventions
− Other interventions or follow-up for the diagnosis or treatment of depression
- Coordinate care between behavioral health and other health care providers. Consider case management.
- Preventive Care Guidelines for providers
- Perinatal Wellness Guidelines for members
- Earn continuing education credit : Watch a recording of our webinar Maternal Mental Health: Pregnancy and Postpartum. Sign in here (registration required) to access the recording.
HEDIS is a registered trademark of the National Committee for Quality Assurance.
The above material is for informational purposes only and is not a substitute for the independent medical judgment of a physician or other health care provider. Physicians and other health care providers are encouraged to use their own medical judgment based upon all available information and the condition of the patient in determining the appropriate course of treatment. The fact that a service or treatment is described in this material is not a guarantee that the service or treatment is a covered benefit and members should refer to their certificate of coverage for more details, including benefits, limitations and exclusions. Regardless of benefits, the final decision about any service or treatment is between the member and their health care provider.

IMAGES
COMMENTS
If a provider assists the patient's primary OB/GYN with the delivery, and is claiming no antepartum or postpartum care, report the appropriate delivery-only CPT® code and append modifier 80 Assistant surgeon. Example: Dr. A is the patient's primary OB/GYN. The patient presents to the hospital in labor. The delivery appears to be ...
59426: Antepartum care only, 7 or more visits; E/M visit if only providing 1-3 visits; Delivery only: CPT codes 59409, 59514, 59612, and 59620; Postpartum care only: CPT code 59430; Diagnosis Codes for Deliveries and Related Services. Reporting Routine Prenatal Visits: routine prenatal visits are reported with a code from category Z34.- It ...
CPT Codes For Global OB . CPT code 59400 - Routine obstetric care, including antepartum care, ... Routine prenatal visits until delivery, after the first three antepartum visits. Recording of weight, blood pressure, and fetal heart tones. ... CPT code 59427 if 4-6 visits are provided, ...
As such, visits for a high-risk pregnancy are not considered routine. They should be reported in addition to the global OB CPT codes of 59400, 59510, 59610 or 59618. If medical necessity is met, the provider may report additional E/M codes, along with modifier 25, to indicate that care provided is significant and separate from routine ...
Modifiers are two-digit codes that show you've somehow altered the service in the original five-digit CPT code. For example, if a woman delivers twins, you may use the "22" modifier to indicate additional or increased services. For a full list of common OB/GYN modifiers, download our coding cheat sheet.
them correctly. The primary CPT code for routine obstetric care, including antepartum care, vaginal delivery, and postpartum care, is 59400. This code includes the services like initial prenatal visits, monthly visits through 28 weeks, biweekly visits from 29-36 weeks, weekly
Many obstetrics/gynecology (OB/GYN) practices are coding deliveries incorrectly or failing to submit claims for "problem visits" during a prenatal or postpartum visit. Common mistakes such as these not only fail to capture payment for services rendered but also the meaningful data that ultimately support patient outcomes.
With understanding comes passion for this ob-gyn niche. Obstetrics and gynecology (ob-gyn) coding is one of those specialties you either love or just Learn about maternal-fetal medicine, an often misunderstood ob-gyn niche. ... The obstetric package includes prenatal visits, delivery, and postpartum care. The CPT® codes for these services ...
Coding for Path and Lab Screenings • 88141-88158 • Cervical or vaginal • Differ by screening method(s) used. • Methods - Thin layer - Slides - Smears • physician interpretation services. • 88142 -specimen collected in fluid medium with automated thin layer preparation -examined using any system of reporting (Bethesda or non ...
CPT Codes for Global OB. CPT code 59400 - Routine obstetric care including antepartum care, vaginal delivery (with or without episiotomy, and/or forceps) and postpartum care. ... Routine prenatal visits until delivery, after the first three antepartum visits. Recording of weight, blood pressure, and fetal heart tones. ... CPT code 59427 if 4-6 ...
conditions that could affect a future pregnancy, and that may be amenable to intervention. • Dx code V26.49: Other procreative management, counseling and advice • CPT code 99401CPT code 99401-99404 Pregnancy - But Before OB Global • How to bill for encounter to diagnose pregnancy - Patient presents with symptomsPatient presents with ...
Coding Spotlight — Pregnancy A provider's guide to diagnosis coding for pregnancy Early and regular prenatal care is vital to the health of the baby and the mother. Pregnancy facts: In 2016, 7.2 percent of women who gave birth smoked cigarettes during pregnancy. Prevalence of smoking during pregnancy was highest for women aged 20-24 (10.7
APEC Guidelines for Routine Prenatal Care . Alabama Perinatal Excellence Collaborative . This document should not be construed as dictating an exclusive course of treatment or procedure to be followed. Guideline 1, version 7 Page 3 of 7 6/30/2015. Subsequent Prenatal Care Visits . At . each. prenatal care visit, routine assessments include: ,
With ICD-10 OB coding came a new set of billing guidelines that can be complicated, especially for newer coders trying to get acclimated to coding. ... For a routine outpatient prenatal visit when no complications are present, select a diagnosis code from range Z34, Encounter for Supervision of Normal Pregnancy, as the primary diagnosis ...
2 factors determine whether you should code a regular antepartum visit If a new patient arrives at your practice in later stages of pregnancy, should you use an initial-visit E/M code or an antepartum visit (four-seven prenatal visits) and delivery only? The choice depends on two factors - the patient's previous care or lack thereof, and payer recommendation, according to the American College ...
visit code. Confirmation of pregnancy visit. The initial E/M visit to determine whether a pregnancy has occurred is not included in the global OB package because it occurs before the beginning of maternity care. Use Z32.01, encounter for pregnancy test, result positive, as principal diagnosis for this visit.
Visits 0502F Subsequent prenatal care visit (Prenatal) [Excludes: patients who are seen for a condition unrelated to pregnancy or prenatal care (e.g. An upper respiratory infection; patients seen for consultation only, not for continuing care)] Postpartum Visits 0503F Postpartum care visit NOTE: The clinical information provided is intended to ...
The global OB care period begins on the date of the initial prenatal visit. Global OB billing methodology will apply only to customers with primary TPL. ... Baby #1: Submit using the global OB CPT code appropriate for vaginal delivery, as well as the initial prenatal care code 0500F with no modifier and $0 charge on the same claim. b. Baby #2 ...
These coverage changes have implications for medical billing and coding. The current mechanisms to bill for obstetric care include billing each office visit as an appropriate Evaluation & Management (E/M) service and billing the delivery CPT codes (59409, 59514, 59612, 59620), or utilizing the global maternity codes.
" For 1-3 antepartum care visits see appropriate E/M codes). 59425 is Antepartum care only 4-6 visits and 59426 is 7 or more visits." I also read the category II codes "0500f Initial prenatal care, 0501F Prenatal flow sheet documented in medical record, and 0502F Subsequent prenatal visits"
• ACOG recommends a minimum of 14 prenatal visits for a 40-week pregnancy. To ensure regular care, members need to get reminders to schedule all required visits, including: o One visit every four weeks until 28 weeks' gestation (at least six visits) o One visit every two weeks until 36 weeks' gestation (at least four visits)
Tips to Close Gaps in Prenatal and Postpartum Care. Check with our members to ensure that initial prenatal visits are scheduled in the first 12 weeks of pregnancy with an OB-GYN, primary care physician or other prenatal practitioner. A postpartum visit must take place on or between seven and 84 days after delivery.
9 likes, 0 comments - drdoneevanrooyenApril 2, 2024 on : "Prenatal visits with your obstetrician are an essential part of a successful pregnancy journey, as they allow you to monitor both your ow..." Prenatal visits with your obstetrician are an essential part of a successful pregnancy journey, as they allow you to monitor both your ow ...
A patient came in for initial prenatal visit and all initial documentation was completed. The physician also added that patient needed annual GYN done and pap smear. The insurance pays for OB visits globally at end of pregnancy. The physician codes V22.0 V72.31 99213 My questions is, shouldn't...