
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support

Pathway of sperm
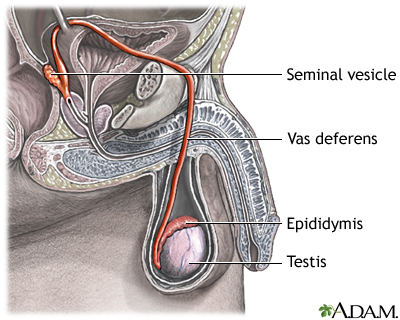
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through the deferent duct through up the spermatic cord into the pelvic cavity, over the ureter to the prostate behind the bladder. Here, the vas deferens joins with the seminal vesicle to form the ejaculatory duct, which passes through the prostate and empties into the urethra. When ejaculation occurs, rhythmic muscle movements propel the sperm forward.
Review Date 7/4/2022
Updated by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Multimedia Encyclopedia
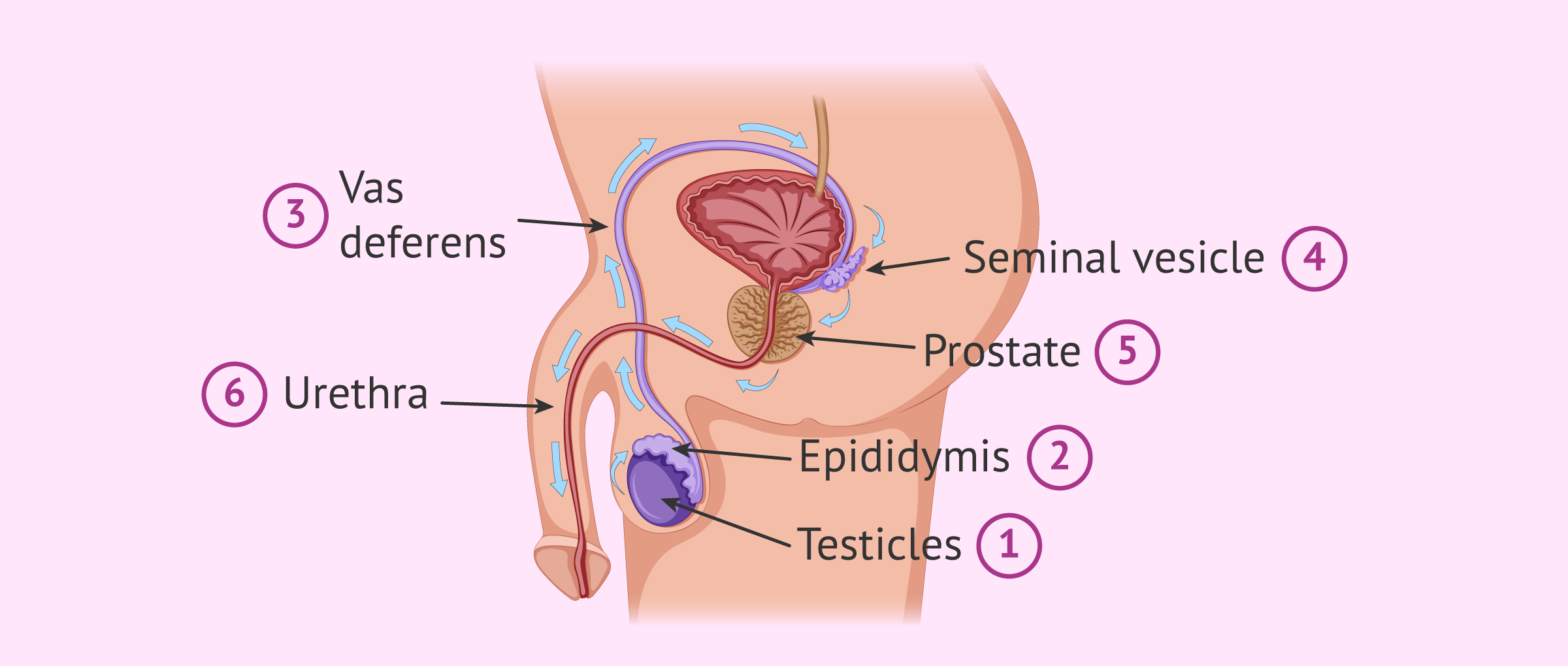
Sperm release pathway

The key male reproductive organs include the testes, epididymis, urethra, vas deferens, prostate gland, seminal vesicle, and penis.
The testes are composed of coiled structures called seminiferous tubules, which are the sites of sperm production. The structure on top of the seminiferous tubules in the testes is the epididymis. The sperm migrate from of the seminiferous tubules to the epididymis. Within the epididymis, the sperm mature while they are stored in this structure.
The ejaculation process begins as the penis fills with blood and becomes erect. With sufficient stimulation, mature sperm travel from the epididymis through the vas deferens, a muscular tube, which propels sperm forward through smooth muscle contractions. The sperm arrive first at the ampulla, where secretions from the seminal vesicle are added.
From the ampulla, seminal fluid is propelled forward through the ejaculatory ducts toward the urethra, passing first by the prostate gland, where a milky fluid is added to form semen. Finally, the semen is ejaculated through the far end of the urethra.
Email address:
Recipients Name:
Recipients address:
Message:
Review Date: 3/28/2016
Reviewed By: Scott Miller, MD, urologist in private practice in Atlanta, GA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.
Sperm Biology from Production to Ejaculation
- First Online: 01 January 2015
Cite this chapter

- Damayanthi Durairajanayagam 4 ,
- Anil K. Rengan BA 4 , 5 ,
- Rakesh K. Sharma 4 &
- Ashok Agarwal 4
2104 Accesses
3 Citations
21 Altmetric
Spermatogenesis is a sequence of highly intricate stages by which an undifferentiated diploid spermatogonium matures into a specialized, genetically unique haploid spermatozoon. Within the Sertoli cells, both mitosis and meiosis are responsible for transforming the diploid spermatogonial cells into unique haploid spermatids. This process requires the assistance of hormones regulated via the hypothalamus–pituitary–gonadal axis—namely, gonadotropin-releasing hormone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). However, not all spermatogonia are destined to mature. In fact, most undergo apoptosis and are phagocytosed. Through spermiogenesis, spermatids elongate to form spermatozoa, which then leave the Sertoli cells and enter the epididymis for final maturation. Here, they acquire motility and acrosomal function, which are necessary for successful fertilization. This entire process from production to ejaculation of mature spermatozoa takes, on average, 64 days to complete. Essentially, spermatogenesis and spermiogenesis create fully functional spermatozoa that can travel efficiently through the female reproductive tract to the ovum and allows for the contribution of exclusive male genes to the offspring genome. This chapter serves as a comprehensive overview of sperm biology from production to ejaculation.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Agger P. Scrotal and testicular temperature: its relation to sperm count before and after operation for varicocele. Fertil Steril. 1971;22(5):286–97.
CAS PubMed Google Scholar
Candas V, Becmeur F, Bothorel B, Hoeft A. Qualitative assessment of thermal and evaporative adjustments of human scrotal skin in response to heat stress. Int J Androl. 1993;16(2):137–42.
Article CAS PubMed Google Scholar
Middendorff R, Muller D, Mewe M, Mukhopadhyay AK, Holstein AF, Davidoff MS. The tunica albuginea of the human testis is characterized by complex contraction and relaxation activities regulated by cyclic GMP. J Clin Endocrinol Metab. 2002;87(7):3486–99.
Roosen-Runge EC, Holstein AF. The human rete testis. Cell Tissue Res. 1978;189(3):409–33.
Holstein AF, Schafer E. A further type of transient cytoplasmic organelle in human spermatids. Cell Tissue Res. 1978;192(2):359–61.
Davidoff MS, Breucker H, Holstein AF, Seidl K. Cellular architecture of the lamina propria of human seminiferous tubules. Cell Tissue Res. 1990;262(2):253–61.
Holstein AF, Maekawa M, Nagano T, Davidoff MS. Myofibroblasts in the lamina propria of human semi-niferous tubules are dynamic structures of heterogeneous phenotype. Arch Histol Cytol. 1996;59(2):109–25.
Holstein AF, Schulze W, Davidoff M. Understanding spermatogenesis is a prerequisite for treatment. Reprod Biol Endocrinol. 2003;1:107.
Article PubMed Central PubMed Google Scholar
Wang H, Xiong W, Chen Y, Ma Q, Ma J, Ge Y, et al. Evaluation on the phagocytosis of apoptotic spermatogenic cells by Sertoli cells in vitro through detecting lipid droplet formation by Oil Red O staining. Reproduction. 2006;132(3):485–92.
Holstein AF. Spermatogenese beim Menschen: Grundlagenforschung und Klinik. Ann Anat. 1999;181:427–36.
Cheng CY, Mruk DD. A local autocrine axis in the testes that regulates spermatogenesis. Nat Rev Endocrinol. 2010;6(7):380–95.
Article CAS PubMed Central PubMed Google Scholar
DeKretser DM, Kerr JB. The cytology of the testis. In: Knobill E, Neil JD, Editors. The physiology of reproduction. New York: Raven; 1994. p. 1177–290.
Google Scholar
Sharpe RM. Regulation of spermatogenesis. In: Knobill E, Neil JD, Editors. The physiology of reproduction. New York: Raven; 1994. p. 1363–434.
Jegou B. The Sertoli cell. Baillieres Clin Endocrinol Metab. 1992;6(2):273–311.
Clermont Y. Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and spermatogonial renewal. Physiol Rev. 1972;52(1):198–236.
Missell LM, Holochwost D, Boban D, Santi N, Shefi S, Hellerstein MK, Turek PJ. A stable isotop-mass spectrometric method for measuring human spermatogenesis kinetics in vivo. J Urol. 2006;175:242–6.
Culty M. Gonocytes, the forgotten cells of the germ cell lineage. Birth Defects Res C Embryo Today. 2009;87(1):1–26
Dym M, Fawcett DW. Further observations on the numbers of spermatogonia, spermatocytes, and spermatids connected by intercellular bridges in the mammalian testis. Biol Reprod. 1971;4(2):195–215.
Holstein AF, Roosen-Runge EC, Schirren C. Illustrated pathology of human spermatogenesis. Berlin: Grosse; 1988.
Izaurralde E, Kas E, Laemmli UK. Highly preferential nucleation of histone H1 assembly on scaffold-associated regions. J Mol Biol. 1989;210(3):573–85.
Adachi Y, Kas E, Laemmli UK. Preferential, cooperative binding of DNA topoisomerase II to scaffold-associated regions. EMBO J. 1989;8(13):3997–4006.
CAS PubMed Central PubMed Google Scholar
Giroux CN. Meiosis: components and process in nuclear differentiation. Dev Genet. 1992;13(6):387–91.
Auger J, Schoevaert D, Negulesco I, Dadoune JP. The nuclear status of human sperm cells by TEM image cytometry: nuclear shape and chromatin texture in semen samples from fertile and infertile men. J Androl. 1993;14(6):456–63.
Miller D, Brinkworth M, Iles D. Paternal DNA packaging in spermatozoa: more than the sum of its parts? DNA, histones, protamines and epigenetics. Reproduction. 2010;139(2):287–301.
Braun RE. Packaging paternal chromosomes with protamine. Nat Genet. 2001;28(1):10–2.
Balhorn R. The protamine family of sperm nuclear proteins. Genome Biol. 2007;8(9):227.
Bedford JM, Calvin H, Cooper GW. The maturation of spermatozoa in the human epididymis. J Reprod Fertil Suppl. 1973;18:199–213.
Russell LD, Griswold MD. The Sertoli cells. Clearwater: Cache Press; 1993.
Breucker H, Schafer E, Holstein AF. Morphogenesis and fate of the residual body in human spermiogenesis. Cell Tissue Res. 1985;240(2):303–9.
Sharma R, Agarwal A. Spermatogenesis: An Overview. In: Zini A, Agarwal A, Editors. Sperm chromatin: biological and clinical applications in male. New York: Springer; 2011. p. 19–44.
Chapter Google Scholar
WHO. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 5. ed. Cambridge: Cambridge University Press; 2010.
Katz DF, Overstreet JW, Samuels SJ, Niswander PW, Bloom TD, Lewis EL. Morphometric analysis of spermatozoa in the assessment of human male fertility. J Androl. 1986;7(4):203–10.
WHO. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4. ed. Cambridge: Cambridge University Press; 1999.
Hafez ES. The human semen and fertility regulation in the male. International Conference in Andrology. J Reprod Med. 1976;16(2):91–6.
Menkveld R, Stander FS, Kotze TJ, Kruger TF, van Zyl JA. The evaluation of morphological characteristics of human spermatozoa according to stricter criteria. Hum Reprod. 1990;5(5):586–92.
Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, van Zyl JA, et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril. 1986;46(6):1118–23.
Langlais J, Roberts KD. A molecular membrane model of sperm capacitation and the acrosome reaction of mammalian spermatozoa. Gamete Res. 1985;12(2):183–224.
Article CAS Google Scholar
Osheroff JE, Visconti PE, Valenzuela JP, Travis AJ, Alvarez J, Kopf GS. Regulation of human sperm capacitation by a cholesterol efflux-stimulated signal transduction pathway leading to protein kinase A-mediated up-regulation of protein tyrosine phosphorylation. Mol Hum Reprod. 1999;5(11):1017–26.
Song X, Li F, Cao G, Zhang J, Han Y. Distribution of alpha-D-mannose residues on zona pellucida and their role(s) in fertilization in pigs. Sci China C Life Sci. 2007;50(2):170–7.
Benoff S, Hurley I, Cooper GW, Mandel FS, Hershlag A, Scholl GM, et al. Fertilization potential in vitro is correlated with head-specific mannose-ligand receptor expression, acrosome status and membrane cholesterol content. Hum Reprod. 1993;8(12):2155–66.
Heller CH, Clermont Y. Kinetics of the germinal epithelium in man. Recent Prog Horm Res. 1964;20:545–75.
Schulze W, Rehder U. Organization and morphogenesis of the human seminiferous epithelium. Cell Tissue Res. 1984;237(3):395–407.
Filippini A, Riccioli A, Padula F, Lauretti P, D’Alessio A, De Cesaris P, et al. Control and impairment of immune privilege in the testis and in semen. Hum Reprod Update. 2001;7(5):444–9.
Mahi-Brown CA, Yule TD, Tung KS. Evidence for active immunological regulation in prevention of testicular autoimmune disease independent of the blood-testis barrier. Am J Reprod Immunol Microbiol. 1988;16(4):165–70.
Sharpe RM. Environmental/lifestyle effects on spermatogenesis. Philos Trans R Soc Lond B Biol Sci. 2010;365(1546):1697–712.
Magelssen H, Brydoy M, Fossa SD. The effects of cancer and cancer treatments on male reproductive function. Nat Clin Pract Urol. 2006;3(6):312–22.
Yeung BH, Wan HT, Law AY, Wong CK. Endocrine disrupting chemicals: multiple effects on testicular signaling and spermatogenesis. Spermatogenesis. 2011;1(3):231–9.
Mathur PP, D’Cruz SC. The effect of environmental contaminants on testicular function. Asian J Androl. 2011;13(4):585–91.
Esteves SC, Zini A, Aziz N, Alvarez JG, Sabanegh ES, Jr., Agarwal A. Critical appraisal of World Health Organization’s new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012;79(1):16–22.
Article PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Center for Reproductive Medicine, Cleveland Clinic, Cleveland, OH, USA
Damayanthi Durairajanayagam, Anil K. Rengan BA, Rakesh K. Sharma & Ashok Agarwal
7 Setter Place, 08824, Kendall Park, NJ, USA
Anil K. Rengan BA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anil K. Rengan BA .
Editor information
Editors and affiliations.
Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine, Weill Cornell Medical College, New York, New York, USA
Glenn L. Schattman
Andrology and Human Reproduction Clinic Referral Center for Male Reproduction, ANDROFERT, Campinas, São Paulo, Brazil
Sandro C. Esteves
Andrology Center & Center for Reproductive Medicine, Lerner College of Medicine Case Western Reserve University, Cleveland, Ohio, USA
Ashok Agarwal
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer Science+Business Media, LLC
About this chapter
Durairajanayagam, D., Rengan, A., Sharma, R., Agarwal, A. (2015). Sperm Biology from Production to Ejaculation. In: Schattman, G., Esteves, S., Agarwal, A. (eds) Unexplained Infertility. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2140-9_5
Download citation
DOI : https://doi.org/10.1007/978-1-4939-2140-9_5
Published : 13 May 2015
Publisher Name : Springer, New York, NY
Print ISBN : 978-1-4939-2139-3
Online ISBN : 978-1-4939-2140-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Route of the sperm from formation to expulsion
Sperm are produces in the seminiferous tubules of the testis, in a process known as spermatogenesis or sperm production .
To be able to leave the testis and come out in the form of semen, spermatozoa go through the seminiferous tubules of the testis to the epididymis in the first place. Then, they travel inside the vasa deferentia and the urethra. It is at this point when they will be ejected.
During their path inside the male reproductive system before ejaculation, they have to cover themselves with fluids secreted by the seminal vesicle and the prostate, which purpose is to nourish and protect the sperm once inside the woman's body.
Leave a Reply

Privacy Overview
- Search the site GO Please fill out this field.
- Newsletters
- Sexual Health
What Happens When You Don't Ejaculate (Release Sperm) for a Long Time?
Wendy Wisner is freelance journalist and international board certified lactation consultant (IBCLC). She has written about all things pregnancy, maternal/child health, parenting, and general health and wellness.
:max_bytes(150000):strip_icc():format(webp)/WendyWisner2022-d8111a5bfee84913ac464f394bc98516.jpeg)
- Side Effects
Benefits of Not Ejaculating
Benefits of ejaculating.
- Side Effects of Frequent Ejaculation
When To See a Healthcare Provider
FatCamera / Getty Images
Ejaculation refers to semen being released from the penis during orgasm. There are many reasons why someone may not ejaculate for a long time. Some people do it intentionally for personal or religious reasons. Some people abstain to increase their sperm count for fertility purposes. Other people may have a health condition that makes ejaculation difficult or impossible.
The effects of not ejaculating haven’t been studied extensively, but there is no evidence that doing so—even for extensive periods—is harmful. There are no known negative side effects of not ejaculating. That said, if you are unable to ejaculate, or are having trouble ejaculating, it’s important to see a healthcare provider to find out if you have an underlying health condition that may be causing this.
Reasons You're Not Ejaculating
There are several reasons why someone may not be ejaculating. Sometimes the reasons are intentional, and sometimes they are not.
Intentionally Abstaining
Whether or not to engage in sexual activity or masturbation is a personal choice. Some people make mindful choices not to ejaculate for specific periods or extended periods. For example:
- Many religions advise abstention from masturbation or sexual activity.
- Someone may also choose not to ejaculate for personal reasons or as a part of a spiritual journey.
- Healthcare providers might recommend abstaining from ejaculating for several days while trying to conceive or before fertility treatments .
Delayed Ejaculation
A sexual disorder called delayed ejaculation can be the cause of not ejaculating. Delayed ejaculation is defined as either a delay in the ability to ejaculate or a complete inability to ejaculate.
Delayed ejaculation is not common and experts aren’t sure what causes it. It used to be believed that relationship issues or psychological issues cause delayed ejaculation. It might be caused by endocrine, genetic, or neurobiological conditions, or it might be a medication side effect. Endocrine conditions are hormone-related, such as low testosterone.
Retrograde Ejaculation
Retrograde ejaculation is when semen is not expelled through the penis during orgasm, but enters the bladder instead. This is often referred to as a “dry orgasm” because you experience an orgasm, but you see a very low volume of semen or no semen at all.
Conditions like diabetes, previous pelvic surgeries, neurological conditions, and bladder malformations can cause retrograde ejaculation. It may also be a side effect of certain medications.
Anejaculation
Anejaculation is when you don’t ejaculate at all during sexual activity. A person with anejaculation experiences erections without ejaculation. However, they may ejaculate during nocturnal emissions (wet dreams) or while masturbating.
There are various potential causes of anejaculation, including health conditions like spinal cord injuries, diabetes, and multiple sclerosis. Potential psychological causes include a lack of body awareness, guilt or shame about sex, and performance anxiety .
People with male reproductive organs can ejaculate and produce sperm for their entire lives—there isn’t a particular age where this ability goes away. However, similarly to people with female reproductive organs, reproductive capacity decreases as they age. As such, it can be more difficult to experience erections and orgasms/ejaculations as they get older.
Side Effects of Not Ejaculating for a Long Time
There is nothing inherently harmful about not ejaculating for a long time. There are no known dangerous physical or psychological side effects. However, some general side effects are possible for certain individuals.
Physical Effects
Testes constantly produce sperm. If you don’t ejaculate it, the sperm becomes reabsorbed into the body. Some people are concerned that you will get “blue balls” if you don’t ejaculate, or pain due to sexual arousal that doesn’t end in orgasm. However, there are no known medical problems associated with this phenomenon, and any discomfort resolves without intervention.
Psychological Effects
The mental health effects of not ejaculating or abstaining from ejaculating aren’t well-researched at this time. However, many people report different emotions when they haven’t ejaculated for a long period of time. Some people might experience clarity or peace of mind , while others may report feeling more irritated or distressed.
People who experience ejaculated-related health problems, such as delayed ejaculation or anejaculation, may experience relationship stress, or anxiety surrounding sexual contact and sexual desire.
There are no reported benefits of not ejaculating, and the benefits of this practice have not been studied. Nevertheless, people who intentionally refrain may report benefits, such as mental and emotional balance, decreased fixation on sex, increased energy, and stress relief.
While many people abstain from ejaculating for several days while trying to conceive, or going through fertility treatments, the effectiveness of this practice is not clear. Research has found that abstaining from ejaculating for several days increases sperm count and semen volume. It’s less clear if this practice is helpful for other sperm aspects, such as motility (movement speed), vitality, and morphology (sperm shape).
Again, the mental health benefits of ejaculating or not ejaculating are not well studied. Still, there are some immediate benefits to experiencing orgasm, including reduced stress, improved mood, and even pain relief.
There is some evidence that ejaculation frequency might be protective against developing prostate cancer . For example, one 2016 study found that participants who reported higher rates of ejaculation were less likely to be diagnosed with prostate cancer.
Side Effects of Ejaculating Too Frequently
It’s normal to ejaculate frequently, and ejaculating daily or even several times a day has no known negative side effects. Ejaculating frequently may cause certain side effects, such as chafing of the skin (usually from masturbation specifically) or fatigue .
Some people may be concerned that frequent ejaculation may cause sex addiction or other sexual disorders. While the exact causes of sex addiction haven’t been identified yet, it is not thought to be caused by excessive masturbation or sexual activity. On the other hand, excessive masturbation or sexual activity may be a symptom of a sex addiction.
Masturbating frequently might affect sexual function, leading to issues like sexual desensitization, where you become less sensitive to sexual stimulation. Some people who masturbate frequently experience trouble getting erections or reaching orgasm through other forms of sexual activity.
It’s normal for some people to not ejaculate for a long time. In most cases, it will not cause physical or psychological harm.
See a healthcare provider if you have any concerns about your ejaculation patterns. If you are intentionally not masturbating because of guilt or shame about sex or masturbation, you may want to speak to a therapist about your feelings and concerns.
Conditions like diabetes, multiple sclerosis, and sexual disorders can result in an inability to ejaculate. Endocrine disorders, neurological disorders, and medication side effects may also cause these symptoms. A healthcare provider can evaluate you for any underlying medical conditions and discuss treatment plans.
A Quick Review
Not ejaculating for several days, weeks, or even longer, is not damaging to your health. Some people abstain from ejaculating for religious reasons, personal reasons, or to increase sperm count while trying to conceive .
If you are unable to ejaculate, you may have an underlying medical condition causing these symptoms. It's important to visit your healthcare provider for an evaluation.
Albobali Y, Madi MY. Masturbatory guilt leading to severe depression . Cureus . 2021;13(3):e13626. doi:10.7759/cureus.13626
Hanson BM, Aston KI, Jenkins TG, et al. The impact of ejaculatory abstinence on semen analysis parameters: A systematic review . J Assist Reprod Genet . 2018;35(2):213-220. doi:10.1007/s10815-017-1086-0
Gopalakrishnan R, Thangadurai P, Kuruvilla A, et al. Situational psychogenic anejaculation: A case study . Indian J Psychol Med . 2014;36(3):329-331. doi:10.4103/0253-7176.135393
Abdel-Hamid IA, Ali OI. Delayed ejaculation: Pathophysiology, diagnosis, and treatment . World J Mens Health . 2018;36(1):22-40. doi:10.5534/wjmh.17051
Society for Male Reproduction and Urology. Treatment options for patients with ejaculatory dysfunction .
Gunes S, Hekim GN, Arslan MA, et al. Effects of aging on the male reproductive system . J Assist Reprod Genet . 2016;33(4):441-454. doi:10.1007/s10815-016-0663-y
MedlinePlus. Sperm release pathway .
Levang S, Henkelman M, Neish R, et al. “Blue balls” and sexual coercion: A survey study of genitopelvic pain after sexual arousal without orgasm and its implications for sexual advances . Sex Med . 2023;11(2):qfad016. doi:10.1093/sexmed/qfad016
Mascherek A, Reidick MC, Gallinat J, et al. Is ejaculation frequency in men related to general and mental health? Looking back and looking forward . Front Psychol . 2021;12:693121. doi:10.3389/fpsyg.2021.693121
MedlinePlus. Delayed ejaculation .
Gianotten WL. The Health Benefits of Sexual Expression . In: Geuens S, Polona Mivšek A, Gianotten W. (eds). Midwifery and Sexuality . doi:10.1007/978-3-031-18432-1_4
Rider JR, Wilson KM, Sinnott JA, et al. Ejaculation frequency and risk of prostate cancer: Updated results with an additional decade of follow-up . Eur Urol . 2016;70(6):974-982. doi:10.1016/j.eururo.2016.03.027
Fong TW. Understanding and managing compulsive sexual behaviors . Psychiatry (Edgmont) . 2006;3(11):51-58.
Huang S, Niu C, Santtila P. Masturbation frequency and sexual function in individuals with and without sexual partners . Sexes . 2022; 3(2):229-243. doi:10.3390/sexes3020018
Related Articles
All about sperm
Sperm Travel Path: Understanding the Route to Fertilization
Short answer sperm travel path: Sperm travel from the testes through the epididymis, vas deferens, and ejaculatory duct before being released through the urethra during ejaculation. The journey takes approximately 64-72 days to complete.
Exploring the Fascinating Journey: Sperm Travel Path
Understanding how sperm travel path affects conception: step by step guide, all you need to know about sperm travel path: frequently asked questions, the intriguing process of fertilization: an in-depth look at sperm travel path, breaking down the miracle of life: inside the male reproductive tract and its role in sperm travel path, discovering the unseen world of conception: the hidden secrets of sperm travel path.
Table of Contents
When it comes to the miracle of human life, there are plenty of fascinating facts and intricate details that often go unnoticed. One aspect of this journey that is particularly intriguing is the path that sperm travel during fertilization. Despite their tiny size, these cells embark on a complex and challenging journey in order to reach the egg.
To begin with, it’s important to understand the basic anatomy of sperm. Each one features a head, midpiece, and tail. The head contains genetic material (DNA) while the midpiece holds mitochondria needed for energy production. Finally, the tail – which resembles a whip-like structure – propels sperm towards its ultimate destination.
The first step in this journey begins when sperm cells are released from the testes. They enter into a part of the male reproductive system known as the epididymis where they mature over several weeks before being released during ejaculation. From here, they must travel through various ducts, including the vas deferens and urethra before exiting through the penis.
Once outside of the male body, sperm face further challenges as they navigate through cervix into uterine cavity via vaginal canal during intercourse or other artificial methods like IVF. Here, they must contend with acidic pH levels in female reproductive tract as well as immune cells that may see them as foreign invaders attempting to harm host (woman carrying embryo).
As if all this wasn’t difficult enough, sperm still have a long way yet to travel! They must then make their way through fallopian tube where fertilization occurs based on their fortunate meeting with an egg cell.
Sperm can remain viable for up to five days within female reproductive tract which provides extra opportunities for fertilization attempting at ovulation time – roughly midpoint menstrual cycle when ovary releases an egg cell into its respective Fallopian tube readying itself for fertilization.
Overall, exploring the fascinating journey undertaken by sperm cells provides us with insight into the incredible complexity involved in human reproduction. From their early maturation in the epididymis to their ultimate goal of reaching and fertilizing an egg, these tiny cells face a veritable obstacle course and yet still manage to achieve what amounts to nothing short of a miracle – when successful fertilization occurs! So let us honor this journey that we often overlooks as we get caught up with complexities of our lives!
When it comes to conception, understanding the process of sperm travel is essential. After all, it takes a single sperm to fertilize an egg and result in pregnancy. So, how does this little swimmer make its way up towards the egg? In this step-by-step guide, we’ll explore the complex journey that sperm must undertake in order to reach their ultimate destination.
The first step in understanding how sperm travel path affects conception is knowing where they come from. Sperm are produced in the testes of males and mature over approximately 72 days. Whenever a man ejaculates, he releases millions of these little swimmers which then navigate through several obstacles before they can reach their final goal.
The next critical step is for them to make their way into the cervix – the opening that separates a woman’s uterus from her vagina. This passage can prove challenging for many sperm as its narrow opening and acidic environment can be quite hostile. Only a relatively small proportion of these hardy cells will remain viable enough to make it through this initial challenge.
Once through the cervix, those swimmer’s that do survive are launched into even rougher waters, weaving their way upstream through thick mucus membranes located inside the female reproductive tract; One by one-many falling by wayside losing momentum along with movement- until only very few finally come close enough to take on and fertilize the coveted ovum or egg.
Fertilization happens when one lucky little guy makes it past all these hurdles and meets a waiting egg emerging around day 14 after ovulation within your fallopian tubes-enabling mothers await with pregnancy tests eagerly due for conception notice.
Overall factors such as age, lifestyle choices such as diet or smoking habits can play vital roles in altering what size or quality of sperms actually end up reaching these prized eggs much later on hence affecting fertility rates drastically causing recurring patterns of infertility rejections for some couples trying to conceive.
In conclusion, the journey of sperm travel is a complex, multi-step process that’s far from easy. However, understanding how it all works can help you boost your chances of conception. With proper planning regarding sexual timing and fertility wellness strategies like stress management or nutritional interventions advised by professionals, it is possible for many couples to overcome these hurdles and bring their family dream into fruition despite any challenges in the path~!
When it comes to reproduction, people often focus on the act of sex itself without giving much thought to what happens after ejaculation. However, understanding the journey that sperm cells take from release into the vagina to reaching their destination can be essential in ensuring successful conception. In this article, we’ll address some frequently asked questions about sperm travel path and give you all you need to know about reproductive biology.
Q: What is sperm? A: Sperm are tiny male reproductive cells that are produced by the testes and contain genetic material needed for fertilization. During sex, they swim through seminiferous tubules and gather in the epididymis before they’re ready for ejaculation.
Q: How does ejaculation work? A: When a man is sexually aroused, his parasympathetic nervous system takes over and signals his body to prepare for ejaculation. Once he reaches orgasm, the muscles surrounding his urethra contract and push semen out of his penis. The average man releases around 2-5 milliliters of semen per ejaculate, containing millions of sperm cells.
Q: Where do sperm go after ejaculation? A: After being released during ejaculation, sperm enter the vagina through semen. While their journey towards their final destination may seem short, it’s actually very intricate due to several variables including acidity levels in cervical mucus as well as vaginal fluctuation in pH.
Q: How long does it take for sperm to reach an egg? A: On average, it takes up anywhere between 30 minutes to three days for a single sperm cell to travel from the cervix up into one of a woman’s fallopian tubes where fertilization can occur with an available egg cell – but depending on conditions like distance between partners’ bodies or time since ovulation conception might never happen at all!
Q: What requirements do sperms have to meet so that they can successfully fertilize an egg? A: Before fertilizing an egg, sperm have to go through a series of tests such as the cervical mucus test and the penetration test. From there, if sperm find their way into the fallopian tubes where an egg is present then they can potentially meet up with waiting eggs for fertilization.
Q: What are some factors that could decrease sperm count or make them less mobile? A: There are several lifestyle habits that could worsen sperm health like smoking or excessive drinking, sedentary behavior and stress which reduces levels of testosterone in males. Poor nutrition, chronic illness, sexually transmitted infections (STIs), genetics, medications you take regularly for other conditions – such as antidepressants- poor sleep hygiene also negatively impacts reproductive function in both men and women.
In conclusion, there’s more to reproductive biology than just intercourse. Understanding the journey that sperms travel from ejaculation to fertilization is essential in ensuring successful conception. While various variables can come into play at times making it challenging for some couples to conceive according to expectations; taking care of yourself and reducing harmful lifestyle choices
Fertilization is a miraculous process that has fascinated researchers since the beginning of time. The combination of genetic material from two different organisms results in the creation of a totally unique being—a blend of traits and characteristics that make each individual distinct and special.
For conception to occur, a male’s sperm must travel through a complex maze before it meets with the female’s egg. This journey starts from the moment an ejaculation occurs and ends when fertilization takes place.
The path sperm take is nothing short of remarkable. It can take anywhere from five minutes to several days for them to reach their destination—a feat, given that sperm cells are minuscule compared to human beings and have to overcome several obstacles along the way.
Once released into the vagina during intercourse, sperm begin their arduous journey upwards into the fallopian tubes, where the female’s egg awaits fertilization. Sperm swim against gravity through multiple barriers such as cervical mucus, which can be difficult to penetrate even for healthy sperm cells.
Sperm’s motility, or ability to move quickly towards their destination, is also crucial in fertilization. They move like tiny propellers driven by a whip-like tail called flagellum, which helps them traverse through different kinds of fluids present throughout their journey.
As they progress further towards fallopian tubes, they encounter various natural filters such as immunity system cells protecting against foreign invaders trying to access eggs leading up to white blood cell towers defending these pathways along their long course “mountains”.
When finally reaching mature ovum awaiting them in its zone at the end of this journey in ampulla regions or points (depending on woman cycle), millions come close but only one makes it inside and fertilize egg marking beginning stages an embryo genesis phase; all others either die or get lost along this path filled with numerous biochemical obstacles preventing successful fertilization at every step (Incredible!).
The process of fertilization carried out by sperm is truly intriguing; it’s a testament to the amazing power and resilience of these tiny, yet mighty cells. It’s a fascinating journey that spans several days and involves crossing numerous barriers and obstacles.
It’s no wonder that researchers and scientists continue to study this complex process, hoping to unravel its mysteries further. Just imagine what other secrets could yet be hidden within the intricate processes of human pregnancy – who knows what new discoveries await us as we delve deeper into the world of reproductive biology!
The miracle of life is a fascinating phenomenon that never ceases to amaze us. We all know that the human reproductive system plays a vital role in bringing new life into this world, but have you ever wondered about the intricacies of the male reproductive tract and its role in sperm travel path? Let’s dive deeper and explore this miraculous journey.
The Male Reproductive Tract
The male reproductive system mainly comprises two organs, the testes and the penis. The testes are responsible for producing sperm cells, which are then transported out of the body by way of the penis. However, it is not as simple as it sounds; several structures and mechanisms ensure that sperm travel along their designated path.
Sperm Production
Sperm production takes place inside a network of tiny tubes called seminiferous tubules located within each testicle. Within these tubes, cells undergo meiosis – a special cell division mechanism – to produce mature, functional sperm cells with half the genetic material required for reproduction.
Transportation
Once produced, mature sperm cells move from seminiferous tubules toward epididymis (a duct situated above each testis). During that journey, they acquire motility from surrounding fluids secreted by accessory glands like prostate gland and seminal vesicle. The fluid also provides nutrients to sustain their energy needs while they swim to reach their ultimate destination — an egg inside female reproductive tract.
Ejaculation
When sexual stimulation or arousal occurs, muscles surrounding the epididymis contract, forcing sperm into vas deferens – muscular ducts that carry them upwards towards prostate gland. Here they mix with seminal fluid when ejaculation occurs—from here; millions of swimming soldiers commence their incredible race to find familiar eggs.
Travel Path
When semen shoots out through penis during ejaculation inevitably makes some contact with outsides surfaces before it enters female genitalia. Inclined vaginal walls help channel movement up toward cervix opening leading deeper into reproductive tract. There are more hurdles to overcome inside a female’s body than one would expect as the path is full of obstacles. This includes acidic environments in the vagina, and barriers produced by mucus on the cervix.
Final Thoughts
The male reproductive tract and its role in sperm travel can be viewed as a remarkable example of evolution at work. The closely coordinated response between organs & proteins secretion, advanced muscular contractions, transportation throughout several ducts – all these mechanisms adapted to enhance chance of fertilization success showcases nature’s brilliance. As humans, we must appreciate how our bodies have evolved over millennia to bring new life into this world. And now that you know just how incredible and fascinating the male reproductive system is let us take a moment to marvel at it.
Conception is one of nature’s most fascinating and intricate processes. It represents the merging of two cells, the sperm and the egg, which leads to a new life. This process has fascinated scientists for years, leading to numerous studies and research in an attempt to uncover all its mysteries. One particular area of discovery that continues to intrigue researchers is the path travelled by sperm during conception.
Sperm travel through a series of complex environments within the female reproductive system on their journey to fertilize an egg. To understand this journey, it’s essential first to know what happens when a male ejaculates.
When males ejaculate, semen – a mixture made up of sperm, enzymes, proteins and other substances – is released from the penis into the female reproductive system via intercourse or direct injection techniques such as artificial insemination. After entering into this environment created by a woman’s body temperature and hormones, some sperm die instantly due to unfriendly conditions like acidity.
The surviving sperms start their journey through different parts of the female reproductive system such as cervix-uterus-fallopian tubes over several hours or days depending on individuals’ anatomy and physiology before finding themselves in contact with an egg cell. This trip requires them first navigating against gravity’s pull entirely; once they reach the uterus at about 45mins/1hour after ejaculation, contractions of cervical mucus carry them further up into fallopian tubes where most successful healthy fertilisations take place under ideal ovulation timing.
While this process seems straightforward enough in theory: get from point A (ejaculation) to point B (an egg cell), there are no guarantees that any given sperm will reach its destination successfully fertilizing an egg cell ultimately. In fact, only about 300 million out of billions released sperm amount actually get close enough for chance encounter with unprotected eggs for natural conceptions: The vast majority wastes existing energy resources lingering around due unfavourable conditions and possible sperm anomalous health issues.
Overall, for conception to occur, the intricate symphony of events leading up to fertilization must work seamlessly together. Even slight disruptions in any of the stages could result in infertility or no viable pregnancies.
Discovering the secrets of sperm travel path is only part of our knowledge pool about reproductive health sciences- as there are still many things we do not know yet; however, it’s an exciting area of study that has vast potential implications for infertility treatments and fertility preservation efforts. It’s an undiscovered universe that presents much promise for improving human reproduction management in spite of its challenging terrain- uncovering more about this unseen world wouldn’t hurt!


IMAGES
VIDEO
COMMENTS
Sperm production in the testes takes place in coiled structures called seminiferous tubules. Along the top of each testicle is the epididymis. This is a cordlike structure where the sperm mature and are stored. The release process starts when the penis fills with blood and becomes erect. Continuing to stimulate the penis will cause an ejaculation.
The journey through the female reproductive system. In the process of ejaculation, sperm cells leave the man and enter the vagina. This is where the sperm cells begin the second part of their journey to fertilization. During this second part of the journey the sperm again encounter an large number of obstacles.
The journey begins when millions of tiny sperm cells are ejaculated from the penis during sexual intercourse or masturbation. These sperm cells are produced in the testicles and stored in the epididymis until they are ready to be released. 2. What is the next step for the sperm after ejaculation? After ejaculation, the sperm start their race ...
Transport of sperm via erection and ejaculation. This video explores the journey of sperm from the male reproductive system to the female reproductive system. It details the two-step process of erection and ejaculation, explaining the role of the brain and blood vessels in achieving an erection. The video also delves into the anatomy of the ...
Pathway of sperm. The testes are where sperm is manufactured. The epididymis is a long coiled structure topping the testis, and it receives immature sperm from the testis and stores them as they mature. When ejaculation occurs, sperm are forcefully expelled from the tail of the epididymis into the vas deferens. Sperm then travel through the vas ...
Let' uncover the fascinating science behind male reproduction, exploring the basics of anatomy of the male reproductive system, puberty, the ejaculation mech...
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through ...
Sperm release pathway. The key male reproductive organs include the testes, epididymis, urethra, vas deferens, prostate gland, seminal vesicle, and penis. The testes are composed of coiled structures called seminiferous tubules, which are the sites of sperm production. The structure on top of the seminiferous tubules in the testes is the ...
The ejaculate, or semen, is freshly produced at the time of ejaculation. Ejaculation normally occurs in a definite sequence. First, a small amount of Cowper's gland fluid is extruded followed by prostatic fluid and the sperm-rich fraction from the ampulla, and finally secretions from the seminal vesicle (Table 5.3 ).
ejaculation, the release of sperm cells and seminal plasma from the male reproductive system. Ejaculation takes place in two phases: in the first, or emission, stage, sperm are moved from the testes and the epididymis (where the sperm are stored) to the beginning of the urethra, a hollow tube running through the penis that transports either ...
5 Sperm Biology from Production to Ejaculation 31 androgen receptors whereas the Sertoli cells have androgen receptors. The binding of ABP to testosterone may assist tes-tosterone movement toward the lumen of the seminiferous tubule onwards to the epididymis. FSH also induces the con-version of testosterone to 5α-dihydrotestosterone (5α-DHT)
Transcript. Explore the male reproductive system with a focus on the testes' role in sperm production and testosterone creation. Discover the importance of temperature regulation for sperm production, the journey of sperm from the epididymis to the urethra, and the role of accessory glands in supporting sperm's journey. Created by Vishal Punwani.
The pathway of sperm is the journey that sperm cells take from the testes to the female reproductive tract during fertilization. The journey involves a series of steps, including production, maturation, and transport. Sperm cells are produced in the testes through a process called spermatogenesis that begins at puberty and continues throughout ...
Prior literature has shown that opacity and sperm concentration of the semen will progressively decrease if the ejaculation occurs shortly after a prior ejaculation and every additional recent ejaculation before that . It should also be noted that colorless mucus-like ejaculate is likely to be pre-ejaculatory fluid from the bulbourethral glands.
Route of the sperm from formation to expulsion. 12. Sperm are produces in the seminiferous tubules of the testis, in a process known as spermatogenesis or sperm production. To be able to leave the testis and come out in the form of semen, spermatozoa go through the seminiferous tubules of the testis to the epididymis in the first place.
People with male reproductive organs can ejaculate and produce sperm for their entire lives—there isn't a particular age where this ability goes away. However, similarly to people with female ...
testicles, make a journey through the male reproductive system, and leave the male's body. When the sperm leave the penis, it is called an erection. ejaculation. On the day in question, it just so happened that the sperm got to be released from the body. First, the penis became larger, longer and firmer until it stuck out from the body. When the
The full cycle for sperm development from production to ejaculation of new mature spermatozoa takes average of 64 days to complete (with a range of 42-76 days) [30,31]. ...
Abstract. Mammalian fertilization comprises sperm migration through the female reproductive tract, biochemical and morphological changes to sperm, and sperm-egg interaction in the oviduct. Recent gene knockout approaches in mice have revealed that many factors previously considered important for fertilization are largely dispensable, or if they ...
Abstract. Millions or billions of sperm are deposited by artificial insemination or natural mating into the cow reproductive tract but only a few arrive at the site of fertilization and only one fertilizes an oocyte. The remarkable journey that successful sperm take to reach an oocyte is long and tortuous, and includes movement through viscous ...
Short answer sperm travel path: Sperm travel from the testes through the epididymis, vas deferens, and ejaculatory duct before being released through the urethra during ejaculation. The journey takes approximately 64-72 days to complete. Exploring the Fascinating Journey: Sperm Travel Path When it comes to the miracle of human life, there are plenty of fascinating […]
The journey of sperm begins inside the testicles. Males begin to produce sperm at the start of puberty at around 12 or 13 years old. It is a process that requires a slightly cooler temperature, which is why testicles hang outside men's bodies. Nor is it a quick process: the production of sperm takes about 70 days.
sperm moves into the epididymis where they are stored and are able to mature. Step 3. travel through the vas deferens, where the sperm mix with other fluids to create semen. Step 4. seminal vesicles secrete thick fluid to keep the sperm healthy and help them move around easily. Step 5. prostate gland secretes a milky liquid that would help ...