
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Overview, Symptoms, & Causes
- Diagnosis, Treatment, & Steps to Take

Diagnosis of Osteoarthritis
There is no single test for osteoarthritis. Diagnosing the condition may include the following:
- Providing to a doctor a medical history that includes your symptoms, any other medical problems you and your close family members have, and any medications you are taking.
- Having a physical exam to check your general health, reflexes, and problem joints.
- X-rays, which can show loss of joint space, bone damage, bone remodeling, and bone spurs. Early joint damage does not usually appear on x-rays.
- Magnetic resonance imaging (MRI), which can show damage to soft tissues in and around the joint. Generally, MRI helps health care providers evaluate a joint that is locking or giving out.
- Having blood tests to rule out other causes for symptoms.
- Taking joint fluid samples to look for other causes of joint pain, such as infection or gout .
Treatment of Osteoarthritis
The goals of your treatment for osteoarthritis include:
- Reducing pain and other symptoms.
- Improving joint function.
- Stopping the disease from progressing.
- Maintaining a health-related quality of life to help prevent disability.
Treating osteoarthritis usually begins with:
- Learning about osteoarthritis. Your doctor may recommend classes that you can attend or online programs you can join.
- Range-of-motion and stretching activities to keep your joints limber.
- Strengthening exercises performed with weights or exercise bands to strengthen muscles that support joints affected by arthritis.
- Exercises in the water to help lower the stress on the joints while exercising.
- Balance and agility exercises to help you maintain daily living skills.
- Low-impact activities that give you a moderate level of activity without putting stress on the joints. These may include walking, cycling, swimming, tai chi, water aerobics, or a low-impact aerobics class.
- Managing your weight can help reduce the stress on joints. In addition, if you are overweight or obese, losing weight can help to reduce pain, prevent more injury, and increase mobility in the joints. This can be especially helpful for weight-bearing joints such as your knees or hips.
- Using braces or orthotics that your doctor prescribes and that are fitted by a health care professional may be helpful to stabilize a joint affected by osteoarthritis.
Some people may need medications to help manage the symptoms of osteoarthritis, including:
- Oral pain relievers.
- Oral anti-inflammatory medications to treat pain and inflammation.
- Topical creams, rubs, or sprays that you apply to the skin over sore joints to relieve pain.
- Corticosteroids, strong inflammation-fighting drugs that are usually injected into the joint to temporarily relieve pain. Because they are potent drugs, your doctor will determine how many injections you should receive and how often to achieve the desired benefit.
- Hyaluronic acid substitutes (viscosupplements), which are injected into the knee to replace a normal component of the joint involved in lubrication and nutrition are sometimes recommended for knee osteoarthritis.
- Selective serotonin and norepinephrine reuptake inhibitors that you take orally to help control chronic (long-term) pain.
If other treatments are not helping and if the joint damage is extensive, some people may have surgery. When considering surgery, many factors may determine if it is the right option, including your age, pain intensity, the degree to which arthritis interferes with your lifestyle, level of disability, and occupation. Surgeries may include one or more of the following:
- Osteotomy: Surgical removal of a piece of bone.
- Partial or total joint replacement surgery : Removal of part of all of the damaged joint and replacing it with a new joint made of plastic, metal, or ceramic.
Other therapies such as massage can increase blood flow and bring warmth to the area. Some research shows that acupuncture may help relieve osteoarthritis pain. Doctors believe that the needles stimulate the release of natural, pain-relieving chemicals produced by the nervous system. Before using other therapies, talk to your doctor about the best options for your treatment.
Who Treats Osteoarthritis?
Treating osteoarthritis requires a team effort involving you and several types of health care professionals. These may include:
- Rheumatologists, who specialize in arthritis and other diseases of the bones, joints, and muscles.
- Primary care doctors, such as a family physician or internal medicine specialist, who coordinates care between the different health providers and treats other problems as they arise.
- Orthopaedic surgeons, who specialize in treatment and surgery for bone and joint diseases.
- Physical therapists, who help improve joint function.
- Occupational therapists, who teach ways to protect joints, minimize pain, perform activities of daily living, and conserve energy.
- Dietitians, who teach about nutrition and maintaining a healthy weight.
- Nurse educators, who help you understand your condition and help start treatment plans.
- Physiatrists (physical, medicine, and rehabilitation specialists), who supervise exercise programs.
- Psychologists or social workers, who help with psychosocial challenges caused by medical conditions.
- Chiropractors, who focus treatment on the relationship between the body's structure, mainly the spine, and its functioning.
Living With Osteoarthritis
There are many things you can do to help you live with osteoarthritis, including:
- Heat and cold therapies can reduce joint pain. Heat therapy increases blood flow, tolerance for pain, and flexibility. Cold therapy numbs the nerves around the joint to reduce pain and may relieve inflammation.
- Support or assistive devices such as a cane or walker can help you move around safely, provide stability, and lower pain. If you have arthritis in your hands, you may find it helpful to use devices to help you grip, such as jar openers.
- Try to avoid repetitive motions, such as frequent bending.
- Shoe inserts or braces can help support your joint and help lower pain and pressure on the area. This can be helpful when you stand or walk.
- Make appointments to see your health care provider. This allows you to participate in your treatment and talk about your symptoms. Some people find it helpful to join a class that provides information on osteoarthritis and how to manage the symptoms to allow you to live an active lifestyle.
- Support groups, both online and in your community, can help you cope and offer tips on how to emotionally manage having the disease and live a healthy lifestyle.
Learn About Research
Related information, view/download/order publications, news related to this health topic, niams hosts roundtable on regenerative medicine in knee oa, recharging cartilage after knee damage, engineered cartilage produces anti-inflammatory drug, machine learning detects early signs of osteoarthritis.
.twitter-f svg{fill:#ffffff;} About NIAMS Clinical Trials Grants & Funding Health Topics Labs @ NIAMS News Room NIAMS Multimedia Library Disclaimer FOIA Contact us Privacy Statement Accessibility HHS Vulnerability Disclosure Social Media Moderation Policy NIAMS Archives Subscribe to Our E-Newsletters Click the button to see different options to sign up for newsletters.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
INTRODUCTION
Osteoarthritis (OA) is a painful condition that can affect one or more joints. It involves loss of cartilage, often along with mild inflammation and changes to the bone closest to the joint, as well as weakness of muscles surrounding the joint ( figure 1 ). This results in pain, stiffness, and trouble easily moving the joint.
Different factors can contribute to the development of OA, including genetic factors, obesity, and joint injury. Although it is more common in older people, OA is not an inevitable part of aging. Any joint can be affected by OA, but it occurs most frequently in the hands, knees, hips, and spine.
OA is a chronic condition that has a variable outcome over time. Over time, symptoms can improve, stay the same, or gradually worsen, especially if contributing factors are not properly modified (particularly increased body weight and misalignment of the joint). There are no therapies available that can slow the progression of changes to the joint. However, treatment can help relieve symptoms, improve your ability to move, and allow you to stay active. The treatment of OA includes a combination of non-drug ("nonpharmacologic") therapies, drug therapy, and, in some cases, surgery.
OA treatment is tailored to you and based upon how severe your pain and stiffness are, which joints are affected, how much difficulty you are having with daily activities, and your preferences. It is important to work with your health care providers to create an effective long-term plan for living with OA that you are comfortable with.
This topic review discusses treatment options for OA. The symptoms and diagnosis of OA are discussed separately. (See "Patient education: Osteoarthritis symptoms and diagnosis (Beyond the Basics)" .)
OSTEOARTHRITIS TREATMENT WITHOUT MEDICATIONS
Non-drug ("nonpharmacologic") therapies are a key part of osteoarthritis (OA) treatment and are recommended for everyone with OA. These can improve arthritis symptoms and have minimal side effects, and they are usually the first treatments clinicians recommend. People who try these approaches often have varying degrees of improvement in their OA pain and ability to do their normal activities.
Weight loss — Obesity and overweight are strongly linked to the development of OA of the knee as well as worsening of the disease over time. Losing weight, even a small amount, appears to lower this risk; higher amounts (around 10 percent of your body weight) may decrease pain by up to 50 percent when achieved through a combination of diet and exercise. An example of 10 percent of body weight is a person who weighs 200 pounds (about 90 kg) losing 20 pounds (9 kg).
It is not well established if weight loss slows the worsening of arthritis in joints that are already affected. However, weight loss may significantly reduce joint pain in "weightbearing" joints, such as the hips and knees. Weight loss is recommended for people with OA with overweight or obesity and is usually combined with strengthening exercises to minimize loss of muscle mass and further improve your condition.
Losing weight can also help improve other health problems that many people with OA have, such as diabetes and high blood pressure. If you want to try to lose weight, your doctor or nurse can talk to you about how to do this in a healthy way. (See "Patient education: Losing weight (Beyond the Basics)" .)
Physical therapy and exercise programs — Physical therapy and exercise improve flexibility and strengthen the muscles surrounding the joints. People who exercise regularly despite their arthritis will typically have less pain and better function than those who are inactive. Even gentle forms of exercise, like walking, have health benefits.
A separate article discusses exercise and arthritis in more detail. (See "Patient education: Arthritis and exercise (Beyond the Basics)" .)
Orthoses — Orthoses are devices that help to keep the joints aligned and functioning correctly. There are different types of orthoses that can reduce symptoms and that can help maintain function in people with OA.
Splints that immobilize the joints (keep them from bending) can reduce pain and inflammation. Many splints can be worn throughout the day and night. Splints are commonly used for OA that affects the base of the thumb. Braces can help some people with knee OA by shifting some of the forces from the affected part of the knee.
Assistive devices — Canes, walkers, electric-powered seat lifts, raised toilet seats, and tub and shower bars can reduce the stress on joints and can make it easier to perform daily tasks. A physical or occupational therapist may suggest these and other assistive devices, depending upon the severity and location of your arthritis.
Arthritis education and support — OA symptoms may cause you to feel frustrated, dependent upon others for help, and even depressed. These factors may reduce your motivation to stick with OA treatment and may make the pain feel worse.
By learning more about OA and how to manage it, you can better participate in your own care. It is important to talk with your health care providers about the options for treating your OA, the effects your OA has on your daily activities, and strategies for coping with the limitations imposed by OA.
Some studies suggest that psychosocial support may be as effective as drug therapy for reducing the symptoms of OA. Some people find it helpful to join a support group or find other ways to connect with other people living with OA. Information about these groups is available below. (See 'Where to get more information' below.)
Some people find that coping strategies such as muscle relaxation, activity pacing (planning exercise and physical activity with regular rest breaks), and pleasant imagery can help with pain. A free pain coping skills training program is available online .
OSTEOARTHRITIS TREATMENT WITH MEDICATIONS
Drug therapy can be started in combination with or after a trial of nonpharmacologic interventions. (See 'Osteoarthritis treatment without medications' above.)
The major medical therapies for osteoarthritis (OA) are described below. Note that opioids (drugs derived from morphine) are not recommended for chronic or long-term relief of OA pain. They have not been found to be more effective than other pain medications for this indication; additionally, they have a relatively high risk of side effects and the potential to cause harm with long-term use.
Topical therapies — Topical nonsteroidal antiinflammatory drugs (NSAIDs) applied to the skin over the joint can help relieve pain for OA involving the hands and knees. There are no major concerns about side effects from topical NSAIDs, although some people may experience local skin rashes that usually resolve by stopping the medication. They are usually tried before oral NSAIDs (pills or tablets).
Topical capsaicin is an over-the-counter cream that can help some people with hand and knee OA as well. The active substance in capsaicin is hot chili pepper, and it is thought to work by depleting a pain-causing substance in nerve endings, which ultimately lessens the OA pain. Some people experience side effects when using capsaicin cream; these include burning, stinging, and redness of the skin (especially if you get it on the skin near your eye).
Nonsteroidal antiinflammatory drugs — Oral NSAIDs help relieve pain and reduce inflammation. They include ibuprofen (sample brand names: Advil, Motrin), naproxen (sample brand name: Aleve), and celecoxib (brand name: Celebrex). Oral NSAIDs are usually used when other therapies (nonpharmacologic and topical therapies) do not adequately relieve symptoms. They should be used at the lowest effective dose for the shortest duration possible because of potential side effects, which include gastrointestinal ulcers, cardiovascular disease, and renal disease. Some people cannot take NSAIDs because of other health conditions that make these drugs unsafe.
NSAIDs are discussed in detail separately. (See "Patient education: Nonsteroidal antiinflammatory drugs (NSAIDs) (Beyond the Basics)" .)
Acetaminophen — Acetaminophen (sample brand name: Tylenol) may have some very small benefits but is usually not significantly effective to relieve OA pain. For this reason, and because it can cause side effects, especially in older adults, many health care providers do not recommend this medication for the treatment of OA. To avoid the possible side effects from acetaminophen, particularly liver damage, it is important to follow dosing instructions and avoid or limit alcohol.
Joint injections — Glucocorticoid (steroid) injections can provide short-term pain relief. They are occasionally recommended for some people who still have significant pain that has not responded to weight loss, exercise, and other medications, or for people who cannot use other medications. Glucocorticoid injections have few side effects, but there is a small risk of joint infection. (See "Patient education: Joint infection (Beyond the Basics)" .)
Glucocorticoids may damage certain joints when injected repeatedly. For this reason, clinicians recommend no more than three to four injections per year for each weightbearing joint, such as a knee, but even this frequency may be harmful to the cartilage if injections are performed routinely.
Injections of a substance called "hyaluronate" are generally not recommended because there is not a lot of good evidence to show that they are helpful, and they are expensive.
Other — Several other therapies have been evaluated to determine if they have any effect on OA. Glucosamine and chondroitin are dietary supplements that have received a lot of attention for their potential benefit in reducing pain without causing any significant side effects. However, there are conflicting results from clinical studies evaluating how well they work for pain from hip and knee OA, with some good-quality studies showing no benefit. As a result, many clinicians do not recommend them because they are costly and haven't been shown to be consistently beneficial in clinical trials. However, clinicians generally do not discourage patients from taking them if they want to try, as there are so few side effects and some people may find relief from them.
Several other OA therapies that are known to be ineffective or are of uncertain benefit are listed below. (See 'Osteoarthritis therapies of no (or uncertain) benefit' below.)
OSTEOARTHRITIS SURGERY
Surgery is usually reserved for severe osteoarthritis (OA) that significantly limits your activities and that did not respond to other treatments. (See "Patient education: Total knee replacement (Beyond the Basics)" .)
People who do get surgery should be in the best possible physical condition and should be prepared to commit to rehabilitation after surgery. Exercise and physical therapy are recommended before and after the surgery to accelerate recovery and increase the chances of having good results. There are a few different types of surgery for OA.
Realignment — Surgery may be used to realign bones and other joint structures that have become misaligned because of longstanding OA. For the knee, realignment may shift weightbearing to healthier cartilage to relieve arthritis pain. This type of alignment may be recommended for younger and more active people as an alternative to replacing the joint entirely.
Fusion — Surgery may be used to permanently fuse two or more bones together at a joint. This may be recommended for badly damaged joints for which joint replacement surgery is not appropriate. Fusion may be recommended for joints of the wrist and ankle and for the small joints of fingers and toes.
Joint replacement — Surgery may be used to replace a damaged joint with an artificial (prosthetic) joint. The most common reason for having joint replacement surgery is pain that is preventing you from doing your usual activities and having an active lifestyle and is not controlled by a combination of nonpharmacologic and drug treatments.
Joint replacement surgery dramatically relieves pain in most people with severe symptoms of hip or knee OA. However, it comes with the risk of potentially serious complications. If you are interested in learning more about joint replacement, talk with your health care provider.
Joint replacement surgery is discussed in more detail separately. (See "Patient education: Total knee replacement (Beyond the Basics)" and "Patient education: Total hip replacement (Beyond the Basics)" .)
OSTEOARTHRITIS THERAPIES OF NO (OR UNCERTAIN) BENEFIT
There are several approaches that have been used to treat patients with osteoarthritis (OA) that are generally not recommended due to lack of evidence showing benefit. In addition, there are other therapies in which the benefit remains uncertain. Some of these interventions include:
● Shoe insoles
● Platelet-rich plasma injections
● Transcutaneous electrical nerve stimulation
● Acupuncture
● Fish oil, curcumin (active ingredient of turmeric), Boswellia serrata , and other nutritional supplements
● Arthroscopy (minimally invasive or "keyhole" surgery)
While some of these approaches may not be harmful, and people sometimes feel that they help, doctors do not routinely recommend them for the treatment of OA.
WHERE TO GET MORE INFORMATION
Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our web site ( www.uptodate.com/patients ). Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below.
Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Patient education: Osteoarthritis (The Basics) Patient education: Deciding to have a hip replacement (The Basics) Patient education: Physical activity for people with arthritis (The Basics) Patient education: Calcium pyrophosphate deposition disease (The Basics) Patient education: Diffuse idiopathic skeletal hyperostosis (The Basics) Patient education: Paget disease of bone (The Basics)
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Osteoarthritis symptoms and diagnosis (Beyond the Basics) Patient education: Losing weight (Beyond the Basics) Patient education: Arthritis and exercise (Beyond the Basics) Patient education: Calcium and vitamin D for bone health (Beyond the Basics) Patient education: Nonsteroidal antiinflammatory drugs (NSAIDs) (Beyond the Basics) Patient education: Joint infection (Beyond the Basics) Patient education: Total knee replacement (Beyond the Basics) Patient education: Total hip replacement (Beyond the Basics)
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Approach to the adult with unspecified knee pain Approach to the adult with unspecified hip pain History and examination of the adult with hand pain Evaluation of the adult patient with neck pain Investigational approaches to the management of osteoarthritis Lumbar spinal stenosis: Pathophysiology, clinical features, and diagnosis Overview of the musculoskeletal complications of diabetes mellitus Pathogenesis of osteoarthritis Patient guidelines for weight-resistance training in osteoarthritis Epidemiology and risk factors for osteoarthritis Overview of surgical therapy of knee and hip osteoarthritis Clinical manifestations and diagnosis of osteoarthritis Clinical manifestations and diagnosis of osteoarthritis, section on 'Shoulder'
The following organizations also provide reliable health information.
● National Library of Medicine
( www.medlineplus.gov/arthritis.html , available in Spanish)
● National Institute of Arthritis and Musculoskeletal and Skin Diseases
(301) 496-8188
( www.niams.nih.gov/health-topics/arthritis )
● National Institute on Aging
( www.nia.nih.gov/health/osteoarthritis , available in Spanish)
● American College of Rheumatology
(404) 633-3777
( www.rheumatology.org/patients/osteoarthritis )
● The Arthritis Foundation
(800) 283-7800
( www.arthritis.org )
● Arthritis Australia
( www.myjointpain.org.au )
ACKNOWLEDGMENT
The editorial staff at UpToDate would like to acknowledge Kenneth C Kalunian, MD, who contributed to an earlier version of this topic review.

Treatments for Osteoarthritis
Learn about treatment options to ease OA pain and other symptoms.
By Mary Anne Dunkin | June 15, 2022
Managing osteoarthritis (OA) pain and maintaining your ability to do daily activities involves physical activity and exercise, weight loss, healthy lifestyle changes and over-the-counter (OTC) or prescription medications. When these don’t sufficiently relieve pain, surgery may be an option. Work closely with your doctor to determine the best treatment plan for you.
The goal of osteoarthritis treatment is to
- relieve pain and stiffness
- help you to maintain normal activities
Physical Therapy and Exercise
Regular physical activity may be the most important piece of your overall treatment plan. Being active can help you stay mobile, relieve pain, lose weight and reduce your risk of other health problems. Activities such as walking, biking, swimming, yoga and water aerobics are all helpful for your OA symptoms and overall health. If joint pain or stiffness makes activity difficulty, work with a physical therapist to develop an exercise plan and find modifications that work for you.
Weight Loss
If you are overweight or obese, losing weight is one of the kindest things you can do for your joints. Not only do fat cells contribute to inflammation, research has shown that every one pound lost results in four pounds less pressure on knees and other weight-bearing joints. One study found that losing 10% to 20% of body weight improved pain, function and quality of life for older adults with obesity and OA.
Medications
Although there are no medications that can slow or stop the progression of osteoarthritis, some can minimize or relieve pain so you can be more comfortable and active, and more activity can further reduce pain and improve fitness. Most medications used to ease osteoarthritis pain are taken by mouth. They include the following:
- Acetaminophen ( Tylenol ). Available over the counter, acetaminophen is an analgesic medication. Acetaminophen alone may be sufficient for mild to moderate OA pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). At over-the-counter doses, NSAIDs such as ibuprofen ( Advil , Motrin IB ) and naproxen sodium ( Aleve ), can ease pain to make physical activity easier. At higher, prescription doses, NSAIDs also relieve inflammation.
- Duloxetine ( Cymbalta ). Although it was developed as an antidepressant, duloxetine is also approved for treating chronic pain, including pain related to OA.
- Tramadol ( Ultram ). Available only by prescription, tramadol is a pain-relief option for OA pain that is not relieved by other medication. Tramadol is an opioid and carries a risk of addiction and abuse. Its use is tightly regulated.
Because medications taken orally to relieve pain may have harmful side effects, your doctor may recommend other options that target only the affected joint(s). If oral medications alone don’t sufficiently relieve your pain, adding one or more of these topical and injectible medications may help.
Topical analgesics are rubbed into, sprayed on or applied as patches to the skin directly over the painful joint(s). They are most effective for joints that are close to the skin’s surface, such as the knees or joints of the hands. Active ingredients in topical analgesics include one or a combination of the following ingredients:
- Capsaicin. A chemical compound in hot chili peppers. When applied to the skin, capsaicin depletes the nerve cells of substance P, a chemical important for transmitting pain messages.
- Salicylates. The same pain-relieving ingredients in aspirin and aspirin-like drugs.
- Counterirritants. Substances such as menthol and camphor, which create a burning or cooling sensation that distracts your mind from your pain.
- Diclofenac. A prescription NSAID that may act similarly to oral NSAIDs to relieve pain.
Different types of injections may also be a part of your OA treatment plan. You may hear about “stem cells” as an alternative, but these have not been proven effective and safe and have not been approved by the Food and Drug Administration.
- Corticosteroids. A strong anti-inflammatory drug similar to the hormone cortisol made by our bodies. When injected into the knee, a corticosteroid can provide quick relief of pain and inflammation.
- Hyaluronic acid. A substance that bolsters joint fluid viscosity and cushioning. Injections of hyaluronic acid, which mimics the natural fluid in joints, are given a week apart in a series of three or four injections.
Other Pain-Relieving Therapies
Beyond medications and exercise, a number of different therapies are available that may help relieve your OA pain.
- Hot and cold. Heat, in the form of a heating pad, warm bath or paraffin wax bath (for hands or feet), can improve blood flow and ease joint stiffness. Using cold packs (such as bag of frozen vegetables placed on the painful joint,) reduces pain and swelling.
- Relaxation techniques. Techniques such as deep breathing, guided imagery and visualization can calm your mind, relax tight muscles and relieve pain.
- Acupuncture. An ancient Chinese medical technique that involves inserting needles into certain points in the body, acupuncture has been shown to help relieve OA pain.
- Massage. Rubbing and kneading of muscles and joints — including self-massage — can help reduce OA pain, improve joint function and ease stress.
- Braces, splints and orthotic devices . Devices such as braces and splints may be helpful for relieving joint pain by shifting weight away from the damaged area of the joint, reducing pressure on the joint and relieving swelling by compression. If you are interested in trying one, consult a physical or occupational therapist to ensure the right fit and proper use.
- Radiofrequency ablation. RFA is a procedure in which a doctor inserts a needle guided by X-ray into the painful area of an arthritic joint, and then passes a current through the needles to ablate or burn the nerve ending to relieve pain. RFA is reserved for people for whom less invasive treatments have failed to relieve pain.
A Healthy Lifestyle
Along with medications, physical activity and weight loss, healthy lifestyle changes can help you better manage osteoarthritis and reduce your risk of health problems that can go along with it.
- Stop Smoking. If you smoke, stop. Some research suggests that people who smoke may have more cartilage loss and pain than those who don’t. If you need joint surgery, smoking can interfere with healing. Of course, it also increases your risk of other health problems.
- Use Self-Help Devices. If arthritis makes it difficult to bend, reach, grasp, stand up or other daily activities, ask an occupational therapist about self-help devices that can make daily tasks easier.
- Seek Emotional Wellness. Pain and limited mobility can lead to anxiety and sadness. But you can learn to cope with arthritis, improve your mood and ease worries.
- Communicate with Your Partner. Arthritis symptoms can affect daily activities — and relationships. Ask for help when you need it and let people in your life know when you aren’t able to do activities you used to. The same is true of sex. Discussing your needs with your partner and finding modifications will help you overcome almost any difficulty.
- Consider Workplace Accommodations. Having osteoarthritis doesn’t have to affect your productivity at work but, depending on the demands of you job and the specific joint(s) involved, certain accommodations may make your job easier. Those may be as simple as adjusting the height of your desk or computer screen, taking breaks to get up and walk around or alternate sitting and standing while you work.
- Eat Well. There is no specific diet for OA . However, eating a diet rich in vegetables, fruit, fish and healthy fats like olive oil will help support an overall healthful lifestyle. A healthy diet can also help you lose weight if needed or maintain a healthy weight. Studies have shown that for people who are overweight, even modest weight loss can reduce OA pain.
- Nutritional supplements. Glucosamine and chondroitin sulfate nutritional supplements — both components of natural cartilage — have been widely promoted and used to treat OA pain. Studies in test tubes and laboratory animals have shown the two compounds may stimulate the production of new cartilage components, but whether that translates to stronger joint cartilage in people is unclear. However, the two supplements, which are available at pharmacies and health-food stores without a prescription — may be effective pain relievers for some people.
When medications and other treatment no longer ease pain, joint surgery is often an option. Hip and knee replacements are the most common surgical procedures for OA and can relieve pain and help restore function.
Osteoarthritis Related Content
Track your health, stay in the know. live in the yes..
Get involved with the arthritis community. Tell us a little about yourself and, based on your interests, you’ll receive emails packed with the latest information and resources to live your best life and connect with others.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The 4 Stages of Osteoarthritis
There are four stages of osteoarthritis (OA) : early, mild, moderate, and severe. You can also be diagnosed with a stage called pre-osteoarthritis.
OA is a progressive joint disease caused by cartilage breakdown. It is the most common form of arthritis. OA can affect any joint in the body but occurs most often in the knees .
It can take anywhere from several months to several years to reach an advanced stage of OA. Your medical provider will assess your symptoms, X-rays, blood tests, and other laboratory tests to define your OA stage and subsequent treatment plan.
This article explains more about the four stages of osteoarthritis and how each one is treated.
Ellen Lindner / Verywell
Stage 0 (Pre-Osteoarthritis)
Stage zero is considered pre-osteoarthritis (pre-OA) and describes a normal, healthy joint before the disease manifests. However, this stage can also describe an early stage of OA when damage is beginning to occur on a cellular level, without clinical signs or symptoms.
Symptoms and Signs
You usually wouldn't have any noticeable symptoms or detectable signs of OA during this stage. You may have experienced several healed or healing injuries of one or more of your joints at this stage, or you might be overusing one or more joints.
Changes to the joint lining that may lead to problems later could be happening at this stage.
The joint changes of pre-OA might not be apparent with imaging tests yet, but it may be possible for pre-OA to be diagnosed with an MRI examination.
Treatment of pre-OA will vary and depends on other health factors. Your healthcare provider may recommend over-the-counter (OTC) medications, supplements, and lifestyle changes.
Avoiding injury, overuse, and damage to your joints could prevent the progression of OA.
You should discuss all of the treatment options for pre-OA with your healthcare provider.
Stage 1 (Early or Doubtful)
Stage one of OA is considered early or doubtful. You may begin to lose some of the cartilage between your joints. However, the space between your joints wouldn't be getting smaller at this point. You may start to develop bone spurs, which are growths on the ends of the bones.
Some people do not have any symptoms or signs during stage one. Others may start to experience mild pain in the joints.
Your healthcare provider may do a physical exam and order an MRI, X-rays, and laboratory tests if there is a concern about your joints.
Most people do not seek treatment during stage one because they do not experience any symptoms. Treatment during stage one is not invasive and focuses on lifestyle changes, supplements, and over-the-counter medications. Lifestyle changes may include exercise, weight loss, yoga, and tai chi.
If you have pain, OTC medications may include nonsteroidal anti-inflammatory drugs (NSAIDs).
Stage 2 (Mild or Minimal)
During stage two of OA, bone spurs grow and become painful. The space between joints may begin to narrow a little. Enzymes can begin to break down the cartilage.
The symptoms of OA in stage two can vary. Some people may start to experience more pain during activity or after a period of increased activity. You may have trouble bending or straightening the affected joints. Sometimes, the pain and stiffness can impair movement.
Your healthcare provider may order X-rays to check for bone spurs and other problems. The X-rays may show bone spurs, but the cartilage may continue to look normal. Diagnosis relies on an assessment of your symptoms, a physical exam, and other tests.
Your practitioner may recommend OTC medications, such as NSAIDs, for pain. You may also need to make lifestyle changes, like losing weight and doing low-impact exercises.
Other treatment options may include strength training and supplements. You may need to wear a brace, shoe insert, wrap, or knee support.
Stage 3 (Moderate)
Stage three of OA is considered moderate, and the cartilage between the bones begins to show signs of wear. The space between joints becomes visibly narrower. More bone spurs may develop and they can enlarge.
Most people have frequent pain when moving, walking, or doing other activities that use the joints. Stiffness in the joints may be worse in the morning and after prolonged sitting. Swelling in the joints may also be visible.
Diagnosis during stage three relies on symptoms and a physical exam. You may also have X-rays and an MRI.
Arthroscopy, a minimally invasive procedure, may be used in the diagnosis as well. Diagnostic arthroscopy involves the insertion of a small scope into the joint to examine it.
Your healthcare provider may start treatment during stage three with OTC medications, like NSAIDs for pain. If they are not enough, your practitioner may prescribe pain medication for you. You may need hyaluronic acid or corticosteroid injections into the joints for pain relief .
Lifestyle changes, such as losing weight and exercising, continue to be important during stage three. You may also need physical therapy.
Stage 4 (Severe)
The amount of cartilage in the affected joints in stage four is much lower—and in some cases, it may be completely gone. The space between the joints is much smaller, and there is less synovial fluid to lubricate the joints. Bone spurs are much larger.
Most people have a lot of pain when using their affected joints. Daily activities may be difficult or impossible to do. Stiffness, swelling, and inflammation can also be severe.
During stage four, diagnosis relies on symptoms, physical exam, lab tests, X-rays, and MRI.
By stage four, non-invasive treatments and lifestyle changes may not be enough. Your healthcare provider may recommend an osteotomy or bone realignment surgery to reduce pain. Arthroplasty or knee replacement surgery is another option.
Osteoarthritis is a progressive disease that is generally broken down into four stages. The amount of time it takes to reach subsequent stages can vary from person to person.
At each stage of OA, it's important to discuss your symptoms and treatment options with a healthcare provider. Although you may begin treatment with noninvasive options, such as OTC medications and lifestyle changes, you may need stronger alternatives if symptoms continue to get worse.
Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee . Arthritis Care Res (Hoboken) . 2020;72(2):149-162. doi:10.1002/acr.24131
Ryd L, Brittberg M, Eriksson K, et al. Pre-osteoarthritis: definition and diagnosis of an elusive clinical entity . Cartilage. 2015;6(3):156-165. doi:10.1177/1947603515586048
Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee osteoarthritis: A primer . Perm J. 2017;21:16-183. doi:10.7812/TPP/16-183
By Lana Bandoim Bandoim has nearly 20 years of experience writing for a variety of outlets including health sites, scientific publishers, and academic medical centers.
- Patient Care & Health Information
- Diseases & Conditions
- Osteoarthritis
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time.
Although osteoarthritis can damage any joint, the disorder most commonly affects joints in your hands, knees, hips and spine.
Osteoarthritis symptoms can usually be managed, although the damage to joints can't be reversed. Staying active, maintaining a healthy weight and receiving certain treatments might slow progression of the disease and help improve pain and joint function.
Products & Services
- A Book: Mayo Clinic Guide to Arthritis
- A Book: Mayo Clinic on Healthy Aging
- Assisted Walking and Mobility Options at Mayo Clinic Store
- Mayo Clinic Sports Medicine
- Products for Mobility and Safety
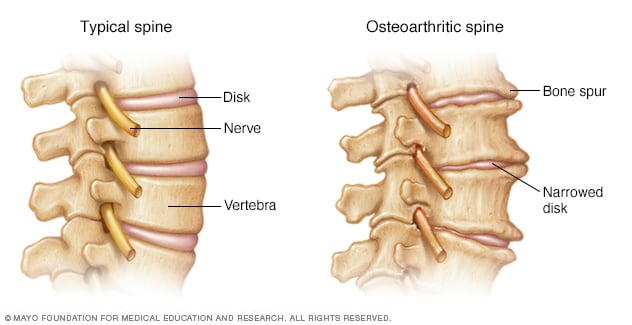
- Bone spurs on spine
In osteoarthritis of the spine, disks narrow and bone spurs form.
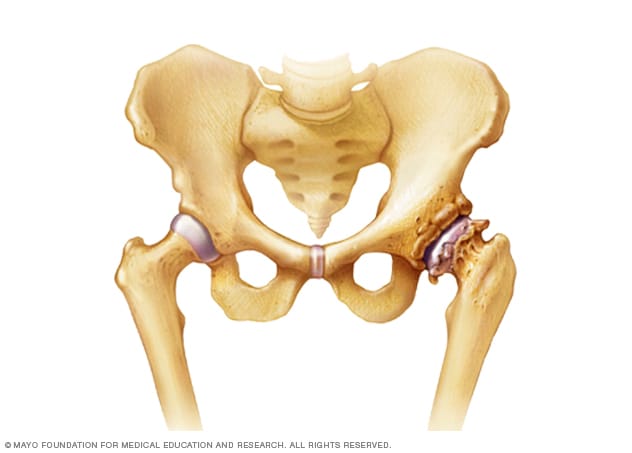
- Osteoarthritis of the hip
The hip joint shown on the left side of the image is healthy. But the hip joint shown on the right side of the image shows the wearing away of cartilage and the formation of bone spurs due to osteoarthritis.
Osteoarthritis symptoms often develop slowly and worsen over time. Signs and symptoms of osteoarthritis include:
- Pain. Affected joints might hurt during or after movement.
- Stiffness. Joint stiffness might be most noticeable upon awakening or after being inactive.
- Tenderness. Your joint might feel tender when you apply light pressure to or near it.
- Loss of flexibility. You might not be able to move your joint through its full range of motion.
- Grating sensation. You might feel a grating sensation when you use the joint, and you might hear popping or crackling.
- Bone spurs. These extra bits of bone, which feel like hard lumps, can form around the affected joint.
- Swelling. This might be caused by soft tissue inflammation around the joint.
When to see a doctor
If you have joint pain or stiffness that doesn't go away, make an appointment with your doctor.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Osteoarthritis occurs when the cartilage that cushions the ends of bones in your joints gradually deteriorates. Cartilage is a firm, slippery tissue that enables nearly frictionless joint motion.
Eventually, if the cartilage wears down completely, bone will rub on bone.
Osteoarthritis has often been referred to as a wear and tear disease. But besides the breakdown of cartilage, osteoarthritis affects the entire joint. It causes changes in the bone and deterioration of the connective tissues that hold the joint together and attach muscle to bone. It also causes inflammation of the joint lining.
Risk factors
Factors that can increase your risk of osteoarthritis include:
- Older age. The risk of osteoarthritis increases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn't clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight adds stress to weight-bearing joints, such as your hips and knees. Also, fat tissue produces proteins that can cause harmful inflammation in and around your joints.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, can increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Repeated stress on the joint. If your job or a sport you play places repetitive stress on a joint, that joint might eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective cartilage.
- Certain metabolic diseases. These include diabetes and a condition in which your body has too much iron (hemochromatosis).
Complications
Osteoarthritis is a degenerative disease that worsens over time, often resulting in chronic pain. Joint pain and stiffness can become severe enough to make daily tasks difficult.
Depression and sleep disturbances can result from the pain and disability of osteoarthritis.
- Osteoarthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/osteoarthritis. Accessed March 7, 2021.
- AskMayoExpert. Osteoarthritis (adult). Mayo Clinic; 2020.
- Kellerman RD, et al. Osteoarthritis. In: Conn's Current Therapy 2021. Elsevier; 2021. https://www.clinicalkey.com. Accessed March 2, 2021.
- Rakel D, ed. Osteoarthritis. In: Integrative Medicine. 4th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed March 2, 2021.
- Deveza, LA. Overview of the management of osteoarthritis. https://www.uptodate.com/contents/search. Accessed March 2, 2021.
- Osteoarthritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Osteoarthritis. Accessed March 2, 2021.
- Arthritis creams
- Degenerative changes in the spine: Is this arthritis?
- Glucosamine: Does it protect cartilage in osteoarthritis?
- Knee osteotomy
Associated Procedures
- Cortisone shots
- Elbow replacement surgery
- Hip replacement
- Knee replacement
- Shoulder replacement surgery
News from Mayo Clinic
- Mayo Clinic Q and A: Spinal arthritis June 06, 2023, 01:30 p.m. CDT
- Mayo Clinic expert offers tips on how to keep joints healthy as you age Oct. 11, 2022, 04:00 p.m. CDT
- Mayo Clinic Q and A: Managing osteoarthritis for hips and knees Sept. 29, 2022, 12:32 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Coronavirus
- Co-pay Cards and Financial Assistance
- Insurance Issues
- Life with Arthritis
- Pain Management
- Depression & Emotional Wellness
- #CreakyChats
- Patient Stories
- Find a Support Group
- Arthritis Clinic
- All Arthritis Types
- Arthritis Treatments
- Arthritis Diet
- What is the Healthcare Team?
- Joint Replacements
- Patient Guidelines
- Back Pain Awareness
- Creakyjoints Podcast Network
- Patient Education Initiatives
- The 50 State Network
- Fail First Hurts
- Healthy Biologics
- The Congressional Arthritis Caucus
- Patient Sentiment toward Non-Medical Drug Switching
- About ArthritisPower
- Other CreakyJoints Research
- Latest Research News
- Participating in Clinical Trials
6.7.22 12:15PM
Rachel Ellis
Home Living with Arthritis Patient Stories
Will’s Osteoarthritis and Psoriatic Arthritis Story: I Learned to Measure Myself Against My Own Baseline
PUBLISHED 06/07/22 BY Rachel Ellis
“I think because this kind of disability is, in most part, an invisible one, people think we should just plow through,” says Will Taylor, who lives with osteoarthritis and psoriatic arthritis. “I don't think there's much public understanding of what it does to the body.”

This story was told to CreakyJoints by Will Taylor, a 53-year-old husband and father on medical leave from his work as a business manager in a special needs school in the UK. Will tells his diagnosis story and shares his experience with the mental toll of chronic disability and how he’s moving forward.
I’ve always been a big chap. In my earlier life, I really enjoyed doing martial arts, playing squash two or three times a week, and going to the gym every day. I was consistent with these types of things up until my early forties when work and life got in the way, and I became more infrequent with my physical activities.
Around age 42, my flexibility seemed to start really slipping. I used to be able to do all the above-the-head kicks in martial arts, but no longer could. I figured it was because I wasn’t practicing as regularly anymore, and I’d just let myself go. But I noticed that I was hurting more after other types of exercise, too. I wasn’t overly concerned. I carried on and assumed my aches and pains were due to my bigger size and older age.
Then when I was 47, I decided to recommit myself to a regular fitness routine. I spent two weeks doing sessions on my elliptical machine and ended up with really bad pains in my shins. I thought I must have given myself shin splints with the exercise, so I gave them a few weeks to heal. But six weeks later, they still weren’t getting better.
“Everyone At Midlife Gets Arthritis”
I went to see my general practitioner, who sent me for X-rays. Right away upon reading them they diagnosed me with osteoarthritis of the hips . It wasn’t a condition on my radar — I had no experience with arthritis, personally or in my family. But the doctors acted like it wasn’t anything to worry about, saying, “Well, everyone at midlife gets arthritis. It’s not such a big deal.”
But the pain kept increasing more and more, and soon started radiating down my legs. So I finally got a referral to an orthopedic physiotherapist. After an MRI, he told me that my arthritis was moderate. That didn’t seem so bad — how serious could “moderate” be? What I didn’t realize was that moderate is only one small rung away from severe.
I kept wondering why I was hurting so much if it was “just” moderate arthritis. I went through treatments of X-ray dye injections to try and get some relief. I started on light painkillers but soon escalated to opioids. The doctors insisted I was “too young” for hip surgery since they have to be replaced every 15 years or so — a fact that I’ve since learned I should have pushed back on — and so they advised me to try to just deal with it as best I could.
Revealing the Full Extent of My Condition
So I put on my best British stiff upper lip, plodding through the pain. But then it just got to be too much. I was having new pains in my lower back. I started to have absences from work. I saw another consultant, and this time they did a full MRI of my spine. It showed bulging discs at all levels, plus degeneration and osteophytes (bone spurs).
It was at that point that they told me my osteoarthritis had spread into my spine. I asked about surgery, but the number of discs that needed treatment meant that surgery might cause more problems than it would fix. But I was able to get in for a left hip replacement soon after. By the time I had the hip surgery, I’d also seen a pain clinic, where I was able to get a steroid injection into my back. It was amazing. It gave me five weeks relief and made me think I might be fixed.
But five weeks’ relief was all I got. I started to get pain in the middle of my back and upper back as well, in my neck. It was also time for my second hip replacement surgery. In addition to that surgery, the pain clinic consultant did ablation therapy on three of the facet joints on the left side of my spine. I pinned a lot of hope on that procedure. I thought it would be the thing that would get me “back to normal.” But it didn’t have any impact. I felt deflated.
Back to the pain clinic I went. At that point my neck was killing me all the time and I was starting to experience numbness in my arms and feet. My feet would feel cold and turn blue. I felt like a real whinger, complaining all the time.
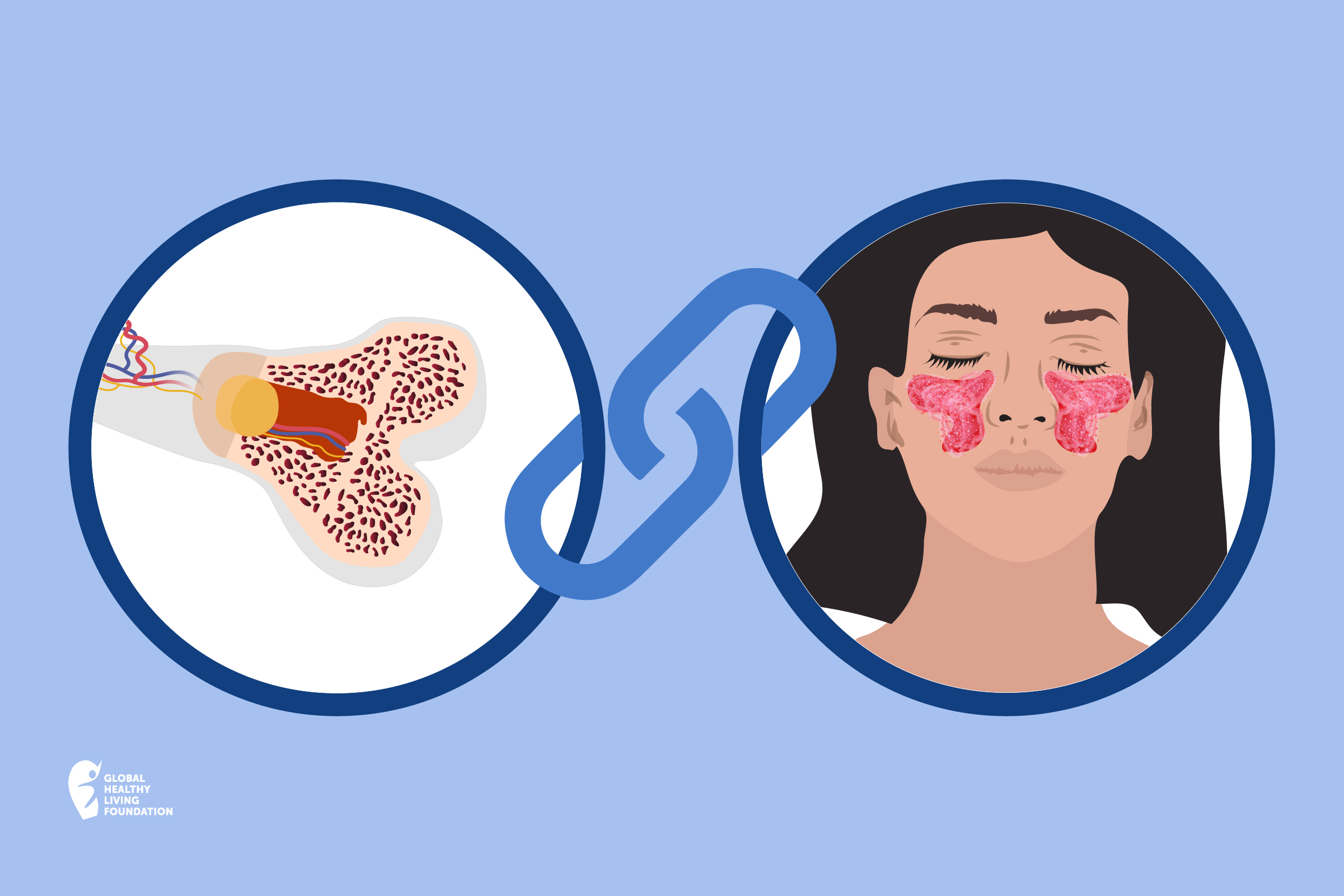
But I was sent to a rheumatologist for yet another MRI and it showed my complaining was not unfounded: There was more degeneration, pinched nerves and bone spurs in my spine, including the thoracic area (which is quite rare). And another diagnosis, to boot: psoriatic arthritis . I’d been using Google for a lot of things but I hadn’t researched that one, even though I had psoriasis . I just hadn’t seen the link.
Learning to Care for Both Body and Mind
Since then I’ve been on heavy duty meds. Physically, I am seeing things worsen. I can see the spiral of lack of activity and muscle wastage. I’ve done physio and exercises, but it hasn’t stopped the wear and tear. I’m at a stage now where I just really physically cannot do anything. One errand out of the house does me in for the day. Yesterday I popped out, went to drop off a car for servicing, popped back and that was it for the day.
I tried to carry on with work, but my boss doesn’t understand disability. I think because this kind of disability is, in most part, an invisible one, people think we should just plow through. I don’t think there’s much public understanding of what it does to the body. I’m looking to see if I’m suitable for what they call here medical or ill health retirement, which means that medically, I can’t work and can draw down elements of my pension to support me earlier.
One of the major impacts that I didn’t foresee was the mental health side of things. You can feel dragged down because you’re constantly in chronic pain. I don’t think I’ve had a day in five years without significant pain.
Mentally, I think I’m coming out of a very low ebb. When it all first started happening and I had to accept and recognize that I was classified as disabled and needed help, I went to a very dark place. I had suicidal thoughts because I felt like a burden on my family. I kept thinking about what it was like for them to see the dad and husband they’ve always known not be able to be that person anymore.
But with counseling and medication for mental health, I’ve been able to shake a lot of that off. And ultimately, the love I have for and from my family has helped take away the thoughts that they would be better off without me.
My Advice for Others Living with Chronic Pain
Be proactive . If you know there’s something wrong, don’t let someone tell you there isn’t. If I had been able to start my psoriasis arthritis medication five years sooner, I may not have lost the function in my joints.
Reach out. You’re not alone. Look for support out there, even if it’s not within your immediate cycle of friends and family, because they’ve got a journey to go on as well. By connecting with other people in a similar boat you can both give and receive support within a community that gets it. ( You can follow CreakyJoints on social media — Facebook , Instagram , Twitter , Tik Tok , YouTube — to connect with other patients who are seeking community for living with arthritis and other chronic illness.)
Ask questions. If you feel fobbed off by doctors during your early symptom days, don’t just accept it has to be that way. It’s hard to challenge medical professionals, but actually, they don’t know everything. They have a broad knowledge, but they don’t know the ins and outs, and they don’t know how you feel. You’ve got to measure yourself against your own baseline.
Be a More Proactive Patient with ArthritisPower
ArthritisPower is a patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. You can participate in voluntary research studies about your health conditions and use the app to track your symptoms, disease activity, and medications — and share with your doctor. Learn more and sign up here .
If you’re interested in being a patient advocate with ArthritisPower and helping our efforts to engage more diverse patient groups in research, check out our Patient Engagement Advisor Program.
- Was This Helpful?
Suggested Reading
What are lupus symptoms — and how do they differ from other autoimmune diseases, beyond burnout: a new chapter in disability advocacy.
- Navigating Chronic Illness: The Power of Shared Decision-Making
Just Published
Patient-friendly news you can use, browse more.
- UR PsA About
- Rheumatoid Arthritis

About CreakyJoints
CreakyJoints is a digital community for millions of arthritis patients and caregivers worldwide who seek education, support, advocacy, and patient-centered research. We present patients through our popular social media channels, our website CreakyJoints.org, and the 50-State Network, which includes nearly 1,500 trained volunteer patient, caregiver and healthcare activists.
CreakyJoints is a digital community for millions of arthritis patients and caregivers worldwide who seek education, support, advocacy, and patient-centered research. We represent patients through our popular social media channels, our website CreakyJoints.org , and the 50-State Network, which includes nearly 1,500 trained volunteer patient, caregiver and healthcare activists.
Quick Links
Press Releases
Our Partners
Our Resources
PatientSpot.org
50Statenetwork.org
FailFirstHurts.org
Terms & Conditions
Download our app, stay connected.

- Living with Arthritis
- All Categories

Kelsey Kloss

Charis Hill

Shelley Fritz

#CreakyChats: Springing Forward: Balancing Tasks and Energy with Chronic Illness
Login / register.
Only fill in if you are not human
- Share full article
Advertisement
Supported by
This Common Condition Can Damage Joints Long Before It’s Detected
Nearly 33 million Americans have osteoarthritis. Experts explain how it affects the body, and why it’s so hard to diagnose.

By Knvul Sheikh
It may start as a twinge in your knee or hip when you get out of bed. Over time, that twinge may turn into persistent pain, swelling or reduced range of motion — signs of a condition called osteoarthritis.
But as with many other chronic conditions, doctors are unable to diagnose osteoarthritis until it has already progressed significantly and has interfered with everyday activities. Scientists are racing to find ways to diagnose osteoarthritis earlier and stave off or slow some of the damage from the disease, which affects over 32.5 million adults in the United States and more than 500 million people worldwide.
Research has started to show that osteoarthritis is not caused solely by everyday wear and tear on joints, like the deterioration of rubber treads on a tire over time. In some patients, persistent, low-grade inflammation might accelerate the progression of the disease or even cause it. And scientists now believe the damage can start long before symptoms appear. In a new study published last week, researchers from Duke University identified molecules circulating in the blood of women that might serve as markers of the disease up to eight years before an X-ray picked up changes in their bones.
“This tells us that there is an osteoarthritis continuum,” said Dr. Virginia Byers Kraus, lead author of the study and a professor of medicine at Duke. “You’re already on an escalator that’s leading you up the path to symptoms and X-ray changes way before we thought.”
What happens in the body in osteoarthritis?
The disease affects cartilage, a protective tissue that serves as padding between the bones in your joints, allowing them to glide over each other when you walk, climb stairs or bend to pick up groceries. It is constantly breaking down with exercise and everyday activities. “But our body typically knows how to repair itself,” said Dr. Elaine Husni, director of the Cleveland Clinic’s Arthritis and Musculoskeletal Center. The fluid surrounding joints contains enzymes that help cut up and remove worn cartilage, while special cells fix minor damage and rebuild cartilage.
But this cycle of breakdown and repair goes awry in people with osteoarthritis, Dr. Husni said. In some patients, those enzymes may be too aggressive in removing cartilage, or the healing process may be much slower than the cartilage breakdown. In others, the body senses damage or stress in the joints, which leads to inflammation. This inflammation tells cartilage-snipping enzymes that they need to come remove worn-down tissue. But if the body can’t dial the inflammation back down after repairs are completed, it can lead to more cartilage breakdown, Dr. Husni said.
Carrying extra body weight is one of the biggest risk factors for developing osteoarthritis. Injuries from sports or repetitive motion also increase the risk of osteoarthritis, as do conditions that involve increased inflammation throughout the body, such as diabetes.
Eventually, the cartilage loses its ability to cushion the bones. This leads to pain, a crackling sensation when moving your joints, reduced range of motion and swelling. The symptoms of osteoarthritis are most common in weight-bearing joints like the knee, hip and lower spine, though they may also occur in the small joints in fingers or feet, Dr. Husni said.
How is osteoarthritis diagnosed?
When a patient shows up with joint pain, a provider might start by feeling for swelling, testing a joint’s range of motion and ordering tests to rule out other problems or types of arthritis.
The current gold standard for diagnosing osteoarthritis is an X-ray, which can show changes in joint structure associated with the disease. The more worn the joint, the narrower the gap appears between bones.
However, by the time these changes show up on an X-ray, the damage to the joint is already done, Dr. Husni said. X-ray images also don’t always correspond to the severity of symptoms or pain that patients experience. “You could have two patients with the same amount of joint space narrowing — something like two or three millimeters on an X-ray — but one patient could have a ton of pain and the other may not,” Dr. Husni said.
While Dr. Kraus’s team and other researchers are studying biomarkers that might make osteoarthritis easier to diagnose, it may take years to prove a blood test is reliable enough to use in clinical settings. Researchers are also looking at whether these and other molecular markers can be used alongside drugs in trials, to measure whether experimental treatments for osteoarthritis are working or not, she said.
For now, patients have to rely on supportive treatments to manage pain, such as heating pads, physical therapy and over-the-counter medicines, Dr. Kraus said.
And people can use the knowledge that osteoarthritis is a slowly progressing disease to take steps to reduce the risk of disease or slow the inevitable wear and tear of joints, Dr. Kraus said: Keeping off excess weight, staying active and following a balanced diet rich in anti-inflammatory foods can help support your joint health and overall well-being.
Knvul Sheikh is a Times reporter covering chronic and infectious diseases and other aspects of personal health. More about Knvul Sheikh
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
- Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Osteoarthritis
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Doug McKechnie, MRCGP Last updated 21 Nov 2022
Meets Patient’s editorial guidelines
In this series: Arthritis Reactive arthritis Septic arthritis Knee replacement
Osteoarthritis is a degenerative joint disease that causes pain and stiffness in joints. Symptoms may be helped by exercises, some physical devices and treatments and by losing weight if you are overweight. Anti-inflammatory painkillers and other medicines are sometimes advised. Joint replacement surgery is an option for severe cases.
In this article :
What is osteoarthritis, what causes osteoarthritis, how common is osteoarthritis, osteoarthritis symptoms, which joints are affected most by osteoarthritis, how is osteoarthritis diagnosed, osteoarthritis treatment, medicines used to treat osteoarthritis, surgery for osteoarthritis, other treatments that are not normally recommended, can osteoarthritis spread.
Continue reading below
Arthritis means inflammation of the joints. Osteoarthritis (OA) is the most common type of arthritis in the UK. Osteoarthritis affects the joint cartilage and the bone tissue next to the cartilage.
See the separate article called What's the difference between osteoarthritis and rheumatoid arthritis? for more information.
All normal joints and joint tissues are constantly undergoing some form of repair. This is because of the wear and tear that is placed on them through our daily activities. However, in some people, it seems that this repair process becomes faulty in some way. This occurs perhaps because of severe wear and tear to the joints or a problem with the repair process, and osteoarthritis develops.
In joints with osteoarthritis, the joint cartilage becomes damaged and worn. The bone tissue next to the cartilage can also be affected and bony growths can develop around the joint edges. These growths are called osteophytes and may be seen on X-rays. The joints and the tissues around the joints can also become inflamed. This inflammation is called synovitis.
Factors that may play a role in the development of osteoarthritis include :
Osteoarthritis becomes more common with increasing age. It may be that the state of the blood supply to the joint and the state of the natural repair mechanisms become less efficient in some people as they age.
There may be some inherited tendency for osteoarthritis to develop in some people. Obesity. Knee and hip osteoarthritis are more likely to develop, or be more severe, in people with obesity. This is because there is an increased stress on the joints and a potential for more joint damage.
Women are more likely than men to develop osteoarthritis.
Previous joint injury, damage or deformity
For example, this may include previous joint infection, a previous break (fracture) in the bone around a joint, or a previous ligament injury that caused a joint instability.
Occupational overuse of a joint
For example, osteoarthritis of the knee may be more common in elite athletes and elbow osteoarthritis may be more common in people working with pneumatic drills.
OA causes joint pain in around 8.75 million people in the UK. Around 32.5 million adults in the United States have OA, according to the Centers for Disease Control and Prevention (CDC).
Primary OA develops in previously healthy joints. Most cases develop in people aged over 50 years. By the age of 65 years, at least half of people end up developing osteoarthritis in some joint(s). It is mild in many cases; however, about 1 in 10 people aged over 65 years have a major disability due to OA. This is mainly due to OA of one or both hips or knees.
Secondary OA develops in joints already affected by previous injury, damage or deformity. This can occur in younger people.
Joint pain, stiffness, and limitation
These are typical symptoms with osteoarthritis. Osteoarthritis pain typically comes on during activities that use the joint; for example, walking or running. The joints feel painful and stiff, which tends to be worse first thing in the morning. It then tends to loosen up after half an hour or so.
Pain, swelling and inflammation
This can sometimes occur in the joints affected with osteoarthritis. However it is not very common for them to be swollen, red or warm. Tell your doctor if a joint suddenly swells up or becomes red or hot. This is a symptom of osteoarthritis that more commonly occurs with other types of arthritis.
People with osteoarthritis often experience 'flares' of symptoms - where pain, stiffness and sometimes joint swelling become worse for several days. This usually settles within a week or two. During a flare, people with osteoarthritis may need to take more pain relief than usual. A joint affected by osteoarthritis tends to look a little larger than normal. This is due to overgrowth of the bone next to damaged cartilage.
Joint deformities
Deformities of joints due to osteoarthritis are uncommon but can sometimes develop.You may have poor mobility and problems walking if a knee or hip is badly affected with osteoarthritis. This may make you more likely to have a fall and cause joint injuries.If you have bad osteoarthritis that affects your hip, you may have difficulty in putting on shoes and socks and getting in and out of a car and doing physical activities. In women, restricted movement of the hip can make having sex difficult and painful.
No symptoms
No symptoms may occur. Quite a number of people have X-ray changes that indicate some degree of osteoarthritis but have no, or only very mild, symptoms. The opposite can also be true. That is, you may have quite severe symptoms that affect your quality of life but with only minor changes seen on the X-ray.
Secondary symptoms
Some people with OA may develop other problems because of their symptoms. For example, pain can affect sleep for some people. Mobility problems may affect your ability to work and carry out family duties. Some people may get down or even depressed because of their pain and other symptoms.
Any joint can be affected by osteoarthritis (OA) but joints in the hips, knees, fingers, thumbs and lower spine are most commonly affected. The shoulders, elbows, wrists, ankles, and toe joints are less commonly affected by osteoarthritis. In many cases, just a few joints develop symptoms with one or two becoming the most troublesome. In some people, osteoarthritis develops in many joints.
Your doctor can often osteoarthritis based on your age, your typical symptoms and examination of your affected joints. Tests such as X-rays or blood tests are usually not needed. However, sometimes your doctor may suggest X-rays or other tests if they are uncertain about the diagnosis and want to exclude other problems.
There is no cure for osteoarthritis but there are a number of things that can be done to ease symptoms and reduce pain. For anyone with osteoarthritis, the aims of treatment should be:
To help you to understand the condition and how to manage it.
To reduce any pain and stiffness.
To maintain or improve the mobility of your affected joint or joints.
To limit any joint damage.
To minimise any disability that may result from your OA.
To minimise any side-effects from medicines used as treatment.
Remember, something can usually be done to help. Osteoarthritis is more common as you become older but it isn't just part of getting older. You don't have to live with pain or disability. Various treatments may help and are discussed below.
If possible, exercise regularly . This helps to strengthen the muscles around the joints affected by osteoarthritis, to keep you fit and to maintain a good range of joint movement. Exercise can reduce joint pain, swelling, and stiffness from osteoarthritis. Swimming is ideal for most joints; other good low-impact exercises include walking, cycling, rowing, and using elliptical trainers. However, any exercise is better than none. Many people can manage a regular walk.
Weight control
If you are overweight, try to lose some weight , as the extra burden placed on back, hips and knees can increase your risk of osteoarthritis or make symptoms of osteoarthritis worse. Even a modest weight loss can make quite a difference.
Shoe insoles and other devices
Some research trials have shown that the following may help to ease symptoms from osteoarthritis of the knee in some cases:
Wearing a knee brace.
Using shoe insoles.
The use of a special sticky tape which pulls the kneecap inwards.
These measures slightly alter the distribution of weight and pressure on the knee joint. This is why they are thought to ease symptoms in some cases. A person qualified to diagnose and treat foot disorders (a podiatrist) or a physiotherapist can advise exactly how to use them.
Braces or supports may also be helpful for other weight-bearing joints affected by osteoarthritis - for example, a support around the thumb for painful thumb osteoarthritis.
The goal of using these devices should be to help improve your symptoms to the point that they are not preventing you from exercising.
Walking aids
If you have osteoarthritis of your hip or knee, when walking try using a walking stick. Hold it in the hand on the opposite side of the body to the affected joint. This takes some pressure off the affected joint and helps to ease symptoms in some cases.
Physiotherapy
Sometimes advice or treatment from a physiotherapist is helpful for osteoarthritis - for example:
For advice on which exercises to do to strengthen the muscles above the knee (quadriceps muscles) if you have osteoarthritis of the knee. Strengthening the quadriceps muscles has been shown to improve symptoms caused by OA of the knee.
For advice on how to keep active and fit.
For advice on shoes, insoles, knee braces, taping to the knee, and how to use walking aids properly (to make sure you have one of the correct height).
Occupational therapy
An occupational therapist may be able to help if you need aids or modifications to your home to cope with any disability caused by osteoarthritis. Special devices, such as tap turners to help with turning on a tap, may mean you can carry out tasks around the house more easily.
Other therapies
Some people have found that transcutaneous electrical nerve stimulator (TENS) machines help to ease pain from osteoarthritis. A TENS machine delivers small electrical pulses to the body via electrodes placed on the skin.
Some people have some pain relief from using hot or cold packs on the affected joint(s). This is also called thermotherapy. You can use a hot water bottle filled with either hot or cold water and apply it to the affected area. Or, special hot and cold packs that can either be cooled in the freezer, or heated in a microwave, are also available.
Paracetamol
Paracetamol is commonly used to treat osteoarthritis (OA). However, recent research suggests that paracetamol is probably not very effective at treating pain from osteoarthritis. Paracetamol - if taken at the recommended dose - is a safe medicine with few side-effects. It may be worth trying, especially for short-term pain relief and where other pain relief options are not suitable.
Anti-inflammatory painkillers (NSAIDs)
You may find that a topical preparation of an anti-inflammatory painkiller that you rub on to the skin over osteoarthritis affected joints is helpful. These are known as "non-steroidal anti-inflammatory drugs" (NSAIDs). This can be instead of, or in addition to, paracetamol tablets. This may be particularly helpful if you have knee or hand osteoarthritis. Examples include ibuprofen gel and diclofenac (topical) .
Compared to anti-inflammatory tablets, the amount of the medicine that gets into the bloodstream is much less with topical preparations. There is also less risk of side-effects (see below).
Anti-inflammatory painkillers that are taken by mouth are not used as often as paracetamol. This is because there is a risk of serious side-effects, particularly in older people who take them regularly. However, one of these medicines is an option if paracetamol or topical anti-inflammatories do not help.
Some people take an anti-inflammatory painkiller for short spells, perhaps for a week or two when symptoms flare up. They then return to paracetamol or topical anti-inflammatories when symptoms are not too bad. There are many different brands of anti-inflammatory painkillers. If one does not suit, another may be fine. A commonly used anti-inflammatory medicine is ibuprofen .
Side-effects
Side-effects may occur in some people who take anti-inflammatory painkillers:
Bleeding from the stomach is the most serious possible side-effect:
This is more of a risk if you are aged over 65 years, or have had a duodenal or stomach ulcer, or if you are also taking low-dose aspirin.
Stop the medicine and see a doctor urgently if you develop indigestion , upper tummy (abdominal) pain, or if you are sick (vomit) or pass blood.
Anti-inflammatory painkillers are often taken together with another medicine that protects the lining of the stomach, such as omeprazole or lansoprazole .
Some people with asthma , high blood pressure , kidney failure and heart failure may not be able to take anti-inflammatory painkillers.
Read the leaflet that comes with the medicine for a list of other possible side-effects.
Opioid medicines such as codeine are sometimes used as a pain reliever for osteoarthritis if paracetamol or topical anti-inflammatory medicines are not sufficient. However the risks as well as benefits of opioid medicines need to be carefully considered, especially for elderly patients.
An injection of steroid medicine
An injection directly into a joint may be an option if a joint becomes badly swollen (inflamed) due to osteoarthritis. However, there is evidence that steroid injections may be either completely ineffective or effective for just a relatively short period of time - usually between two and ten weeks.
Herbal creams and gels
There is not a great deal of evidence from studies to show that herbal remedies are effective:
Arnica gel probably improves symptoms as effectively as a gel containing non-steroidal anti-inflammatory drugs (NSAIDs).
Comfrey extract gel probably improves pain.
There has been no strong evidence for capsicum extract gel.
However, capsaicin gels and creams have been recommended as being effective for reducing osteoarthritis (OA) pain, especially for knee or hand osteoarthritis. Capsaicin is a herbal medicine extracted from chilli peppers.
Food supplements as a treatment of osteoarthritis
Various food supplements that you can buy from health food shops and pharmacies have been recommended (advocated) to help in the treatment of osteoarthritis. In particular, glucosamine and chondroitin supplements have become popular in recent years. Glucosamine and chondroitin are chemicals that are part of the make-up of normal cartilage. The theory is that taking one or both of these supplements may help to improve and repair damaged cartilage.
However, the usefulness of glucosamine and chondroitin is controversial. For example, a large study published in 2007 concluded that chondroitin has little, or minimal, effect on reducing symptoms in people with osteoarthritis. The National Institute for Health and Care Excellence (NICE) does not recommend the use of chondroitin for the treatment of osteoarthritis. This is because they could find no clear evidence from studies to show that it is an effective treatment.
Another large study was published in the British Medical Journal (BMJ) in 2010. This analysed 10 research trials of glucosamine and chondroitin supplements, involving over 3,800 patients with knee and hip osteoarthritis. The conclusion of the study was that the supplements appeared to be no better than a dummy (placebo) tablet at relieving pain.
However, there was considerable correspondence that followed the BMJ study. Some writers were critical of the study's design and conclusions. Some cited other studies and individual cases that seemed to show some benefit from glucosamine and chondroitin.
So, it is difficult to give firm advice. What seems clear is that glucosamine and chondroitin are no wonder cures. One or both may possibly help in some cases. It may be worth discussing these supplements with your doctor. If you do try a food supplement you should assess your level of pain before you start taking it, and then again after three months. If there is no improvement, it would seem reasonable to conclude that it is unlikely to be effective and there is no point in carrying on with it.
Note : you should not take glucosamine if you are allergic to shellfish. Glucosamine may also interact with warfarin. You should talk with your doctor or pharmacist before you take glucosamine if you are on warfarin treatment.
Most people with osteoarthritis do not have it badly enough to need surgery. However, OA of a joint may become severe in some cases. Some joints can be replaced with artificial joints. Hip and knee replacement surgery has become a standard treatment for severe osteoarthritis of these joints. Some other joints can also be replaced.
Joint replacement surgery has a high success rate. However, like any operation, joint replacement surgery has risks.
Some treatments have become fashionable or popular for osteoarthritis but are not normally recommended by mainstream doctors. For example:
Hyaluronic acid
Regular injections of hyaluronic acid directly into a joint are a relatively new treatment which has been tried for osteoarthritis The theory is that it may help with lubrication and shock absorption in a damaged joint. It may produce a small beneficial effect in some people. However, NICE has looked at hyaluronic acid as a possible treatment for osteoarthritis and does not recommend its use. This is because there is little evidence that it is effective and there may be a risk of problems after the treatment.
Heat rubs (topical rubefacients)
Although widely used, NICE does not recommend their use for osteoarthritis. This is because there is little scientific evidence to say that they work.
Arthroscopic lavage and debridement
This is an operation to wash out a joint and trim cartilage from a joint. NICE recommends that this should not be offered as part of treatment for osteoarthritis.
Magnetic resonance therapy
This is a new treatment which uses a device with magnets to try to improve pain and healing in the joint. NICE in the UK looked at the evidence for this in 2021 and concluded that, although there is no evidence of this being harmful, there is also not enough evidence that it works for osteoarthritis. NICE recommends that this treatment should only be given as part of a research study.
Geniculate artery embolism
This treatment aims to reduce blood flow to the damaged part of the knee joint, aiming to reduce further damage and pain. NICE looked at the evidence in 2021, concluding that although there were no short-term safety concerns, there was not enough evidence on long-term safety, and insufficient evidence to show that it works. NICE recommends that this treatment should only be given as part of a research study.
A common wrong belief is that osteoarthritis is always a progressive and serious disease. The severity of symptoms varies. In many people, osteoarthritis is mild. It does not become worse and does not make you any more disabled than expected for your age. However, in some people, the severity of OA and the disability it causes are out of proportion with their age. One or more joints may become particularly badly affected.
Symptoms often wax and wane. Flare-ups of symptoms for days to weeks are common. Sometimes this is related to things such as the weather. Symptoms often improve in warmer months. A bad spell of symptoms may be followed by a relatively good period.
Further reading and references
- Wandel S, Juni P, Tendal B, et al ; Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010 Sep 16;341:c4675. doi: 10.1136/bmj.c4675.
- EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis ; Annals of Rheumatic Disease (April 2013)
- Cameron M, Chrubasik S ; Topical herbal therapies for treating osteoarthritis. Cochrane Database Syst Rev. 2013 May 31;5:CD010538. doi: 10.1002/14651858.CD010538.
- Osteoarthritis ; NICE CKS, August 2022 (UK access only)
- Magnetic resonance therapy for knee osteoarthritis ; NICE Interventional procedures guidance, August 2021
- Genicular artery embolisation for pain from knee osteoarthritis ; NICE Interventional procedures guidance, October 2021
- Osteoarthritis in over 16s: diagnosis and management ; NICE guideline (October 2022)
- Kolasinski SL, Neogi T, Hochberg MC, et al ; 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken). 2020 Feb;72(2):149-162. doi: 10.1002/acr.24131. Epub 2020 Jan 6.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 20 Nov 2027
21 nov 2022 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free

IMAGES
VIDEO
COMMENTS
OSTEOARTHRITIS (OA): PATIENT JOURNEY You may experience the following signs and symptoms in one or more affected joints: occasional and intermittent pain, aching, morning stiffness lasting less than 30 minutes, reduced range of movement, creaking (crepitus) in your joints and/or swelling. Osteoarthritis can occur in any
Osteoarthritis Patient Education & Resources. Traditionally thought of as a disease related to aging and "wear and tear," osteoarthritis (OA) is now recognized as a disease of the whole joint. ... Treating OA Is a Journey. Osteoarthritis may mean major surgery in your future. But first, there are options. Learn More.
Symptoms. You may experience the following signs and symptoms in one or more affected joints: occasional and intermittent pain, aching, morning stiffness lasting less than 30 minutes, reduced range of movement, creaking (crepitus) in your joints and/or swelling. Osteoarthritis can occur in any movable joint, but most commonly affects knees ...
A patient journey is the sequence of events that a person with osteoarthritis experiences, from the first signs of symptoms to diagnosis and later to treatment and management. Not all steps will be the same for everyone, but it can give you an idea of what you may expect and how to effectively manage your osteoarthritis.
Realigning bones. If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee, and then removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
Purpose: Knee osteoarthritis (OA), a leading cause of chronic pain and disability, affects an estimated 32.5 million adults in the United States. Knee OA patients receive care from various physician specialties, including orthopedists (OS), rheumatologists (RH), sports medicine (SM) physicians, and pain specialists (PS). Current treatments for knee OA target symptoms with conservative ...
Nondrug therapies. Medications. Relaxation. Impact on outcomes. Resources. Summary. The goal of osteoarthritis (OA) patient education is to give a person the information they need to optimize ...
Osteoarthritis can affect any of your joints, but most commonly develops in your: Hands. Knees. Hips. Neck (cervical spine). Lower back (lumbar spine). Types of osteoarthritis. A healthcare provider might classify osteoarthritis as one of two types: Primary osteoarthritis is the most common form of osteoarthritis that develops in your joints ...
Partial or total joint replacement surgery: Removal of part of all of the damaged joint and replacing it with a new joint made of plastic, metal, or ceramic. Other therapies such as massage can increase blood flow and bring warmth to the area. Some research shows that acupuncture may help relieve osteoarthritis pain.
Osteoarthritis (OA) is a painful condition that can affect one or more joints. It involves loss of cartilage, often along with mild inflammation and changes to the bone closest to the joint, as well as weakness of muscles surrounding the joint ( figure 1 ). This results in pain, stiffness, and trouble easily moving the joint.
Hot and cold. Heat, in the form of a heating pad, warm bath or paraffin wax bath (for hands or feet), can improve blood flow and ease joint stiffness. Using cold packs (such as bag of frozen vegetables placed on the painful joint,) reduces pain and swelling. Relaxation techniques.
Stage 1. Stage 2. Stage 3. Stage 4. There are four stages of osteoarthritis (OA): early, mild, moderate, and severe. You can also be diagnosed with a stage called pre-osteoarthritis. OA is a progressive joint disease caused by cartilage breakdown. It is the most common form of arthritis.
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time. Although osteoarthritis can damage any joint, the disorder most commonly affects joints in your hands, knees, hips and spine.
One Patient's Journey: Living with Osteoarthritis. ... Osteoarthritis (OA), sometimes called wear-and-tear arthritis, is the most common form of arthritis and can occur in any joint. Typically ...
This story was told to CreakyJoints by Will Taylor, a 53-year-old husband and father on medical leave from his work as a business manager in a special needs school in the UK. Will tells his diagnosis story and shares his experience with the mental toll of chronic disability and how he's moving forward. I've always been a big chap.
When a patient shows up with joint pain, a provider might start by feeling for swelling, testing a joint's range of motion and ordering tests to rule out other problems or types of arthritis.
The patient journey in knee osteoarthritis-variations in diagnosis, patient characteristics, and treatment by physician specialty. Osteoarthritis and Cartilage. 2021; 29 (1):281-282. [Google Scholar] 23. Wallis J.A., Taylor N.F., Bunzli S., Shields N. Experience of living with knee osteoarthritis: a systematic review of qualitative studies.
Osteoarthritis is a degenerative joint disease that causes pain and stiffness in joints. Symptoms may be helped by exercises, some physical devices and treatments and by losing weight if you are overweight. Anti-inflammatory painkillers and other medicines are sometimes advised. Joint replacement surgery is an option for severe cases.
Download Citation | On Apr 1, 2021, A.V. Bedenbaugh and others published The patient journey in knee osteoarthritis-variations in diagnosis, patient characteristics, and treatment by physician ...
Home | Arthritis Society Canada
The Patient Journey in Knee OA: Variations in Patient Characteristics and Treatment by Physician Specialty Angela V. Bedenbaugh, PharmD1, Gary Oderda, ... Knee osteoarthritis (OA) affects an estimated 32.5 million US adults. 1 Knee OA is diagnosed and treated by multiple specialties and comprises
Abstract. Rheumatoid Arthritis (RA) is a chronic disease that impacts patients' quality of life. Sophisticated organization of care delivery drives quality improvement. Therefore, the study objective was establishing a validated process map of the care cycle for RA patients. Hence, increasing transparency and optimizing care delivery and ...
Results. Panellists agreed that American College of Rheumatology classification criteria is mostly sufficient to provide an OA diagnosis in clinical practice, OA patients with ≥5 Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain or physical function score can be defined as moderate-to-severe OA if they have an additional ≥2 Kellgren-Lawrence (KL) score, a minimum ...
Vertex continued to reach more CF patients, delivering $2.7 billion in revenue in Q1, representing 13% growth versus the prior-year period. We also began our journey of revenue diversification ...